Malignant paraganglioma, a rare presentation with foot drop: a case report
Introduction
Extra-adrenal paragangliomas are rare neuroendocrine tumors that arise from the extra-adrenal autonomic paraganglia, small organs consisting mainly of neuroendocrine cells that are derived from the embryonic neural crest and have the ability to secrete catecholamines (1). Paragangliomas can be found in several locations. When the tumor occurs in the adrenal gland, it is called pheochromocytoma; in the head and neck region, the paragangliomas can be found in the carotid body, vagus nerve and middle ear (jugulotympanic); other locations also include the retroperitoneum, para-aortic region, bladder, filum terminale, skull, larynx, and others (2,3). Malignant paraganglioma is a very rare presentation (4,5). The majority of paragangliomas are sporadic; however, approximately one third to one half are associated with inherited syndromes (6). The annual incidence in retrospective studies is 1/10,000,000 (7).
Case presentation
A 56-year-old previously healthy lady presented to the emergency department with a 3-week history of worsening lower back pain with right-sided sciatica and new onset of right foot drop. She was recently diagnosed with hypertension and had been complaining of intermittent headaches.
Upon examination, systolic blood pressure was found in the upper normal range. The patient was walking with an obvious limping gait, with tender lower back and positive straight leg raise test on the right side. A right foot drop with weakness of ankle dorsiflexion/plantar flexion and absent right ankle reflex was also noted.
Computed tomography (CT) imaging of the lumbar, chest, abdominal and pelvic regions showed a large heterogeneous retroperitoneal abdominal mass as well as mass lesion at L5 posterior elements/pedicles with significant compression of thecal sac and severe canal compromise. Multiple spinal bony lytic lesions as well as pulmonary lymph nodes were found.
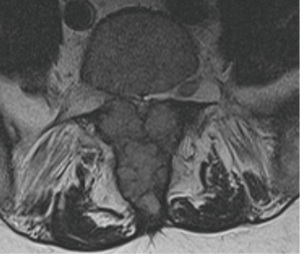
Magnetic resonance imaging (MRI) of the lumbar spine demonstrated multiple deposits within the lumbar spine, the largest within the posterior elements and pedicles of L5 causing severe central canal stenosis and compression of thecal roots and exiting right L5 nerve root (Figures 1,2,3). Three other enhancing lesions within the vertebral marrow without neural compromise were found at L1, L5 and S2.

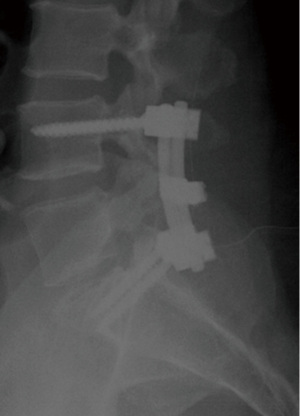
For management, the patient underwent decompressive L5 laminectomy with tumor debulking, rhizolysis and pedicle screw fixation from L4/S1 (Figure 4). Malignant hypertension crisis occurred intra-operatively and postoperatively with systolic blood pressure >250, as well as tachycardia and new left bundle branch block on electrocardiogram (ECG). Blood pressure was difficult to control. Echocardiography was normal. The patient developed hospital-acquired pneumonia with parapneumonic effusion but improved with physiotherapy and antibiotics. She also developed anemia.
Analysis of histopathological samples confirmed the diagnosis of malignant paraganglioma. The patient started to mobilize on day 3 post-operatively and her radicular pain completely resolved. Power on right foot examination returned to normal. Medical oncology team reviewed patient and tumor markers for paraganglioma/pheochromocytoma (synaptophysin, chromogranin A, CD17, CK5/6, plasma metanephrine and Ki-67) were positive. She had a staging positron emission tomography (PET) scan/I-MIBG scan that showed grade IV widespread disease with multiple bony metastases (lytic lesion of T7, L5 and NOF). These also showed liver metathesis as well as right kidney obstruction due to tumor invasion. She underwent palliative radiotherapy (8,9) for her thoracolumbar spine and right hip.
Discussion
Spinal paragangliomas are tumors of neuroendocrine origin that rarely involve the spine (usually the filum terminale and cauda equina). Paragangliomas and pheochromocytomas overall are most commonly located within the adrenal gland (pheochromocytomas) or in the head and neck. Paragangliomas are slow-growing tumors arising from non-chromaffin paraganglion cells that are scattered throughout the body from the glomus jugulotympanicum to the bladder. They are related to pheochromocytomas, which are chromaffin-positive. Paragangliomas can occur anywhere in the body there are sympathetic nerve cells (e.g., paravertebral ganglia) and they often (~50%) secrete catecholamines; thus, they are also called extra-adrenal pheochromocytomas. Other locations include organ of Zuckerkandl and bladder (rare), paraganglia related to the great vessels of the head and neck and base of skull and scattered in other tissues (bladder, ciliary ganglion, pharynx and larynx).
Epidemiology
The age at presentation for spinal paragangliomas varies from 13 to 70 years. The mean age at presentation is 47 years (10). Males are more commonly affected than females.
Clinical presentation
The patient often presents with local mass effects of neuroendocrine symptoms. The most common presenting symptoms are lower back pain and sciatica from the mass effect of the tumor (11). Cauda equina paragangliomas frequently actively secrete neuropeptides, particularly 5-hydroxytryptamine and somatostatin, although symptoms related to this chemical production are usually absent. Additionally these lesions may be a rare source of superficial siderosis, and thus patients may present with sensory neural impairment, cranial nerve dysfunction and myelopathy.
Pathology
All paragangliomas consist of nests (Zellballen) of chief cells (polygonal) enclosed by trabeculating fibrous components and sustentacular cells. They are highly vascular WHO grade I neoplasms. The majority (75%) of paragangliomas are encapsulated.
Radiographic features
Plain films are unlikely to demonstrate any abnormalities, although vertebral scalloping or rarely calcification may be seen. Conventional angiography demonstrates an intense early blush that persists into the late arterial and early venous phases. Spinal paragangliomas appear as soft tissue masses inferior to the conus. If contrast is administered, they enhance vividly, as do paragangliomas elsewhere. Large lesions may rarely demonstrate osseous erosion or remodelling of the adjacent vertebrae (vertebral scalloping). Rarely these lesions calcify. Similarly, on MRI these masses usually appear as well-circumscribed masses, inferior to the conus. With some lesions, the characteristic ‘salt-and-pepper’ appearance of neck and skull base paragangliomas may also be seen. Associated syringohydromyelia has been reported in some cases. Reported signal characteristics include: T1 isointense, T2 hyperintense flow voids are typically seen along the surface of and within the tumor nodule; hemorrhage is common (12), leading to a ‘cap sign’ (13); T1 C+ (Gd): intense enhancement is virtually always seen.
Treatment and prognosis
Surgical resection is the treatment of choice, sometimes with preoperative embolization to reduce intra-operative blood loss. Post-resection recurrence rate is less than 5%. In metastatic disease, prognosis is very poor.
Conclusions
In summary, we reported a rare case of foot drop due to metastatic malignant paraganglioma. Urgent decompressive spine surgery led to complete resolution of the foot paresis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interests to declare.
References
- Lin D, Carty SE, Young WF. Paragangliomas: Epidemiology, clinical presentation, diagnosis, and histology. In: Wen PY, Loeffler JS, Lacroix A, eds. Waltham: UpToDate, 2015.
- Yu L, Wang J. Malignant paraganglioma of the rectum: the first case report and a review of the literature. World J Gastroenterol 2013;19:8151-5. [PubMed]
- Flitsch J, Schröder F, Hagel C, et al. Cranial neuroendocrine carcinoma primarily diagnosed as malignant paraganglioma with rapid progress to a fatal outcome. Acta Neurochir (Wien) 2001;143:523-4. [PubMed]
- Lázaro B, Klemz M, Flores MS, et al. Malignant paraganglioma with vertebral metastasis: case report. Arq Neuropsiquiatr 2003;61:463-7. [PubMed]
- Sasaki K, Inose H, Kawabata S, et al. Combined surgical and radiosurgical treatment for a symptomatic cervical metastasis in a case of malignant paraganglioma: a case report. BMC Res Notes 2013;6:494. [PubMed]
- Boedeker CC. Paragangliomas and paraganglioma syndromes. GMS Curr Top Otorhinolaryngol Head Neck Surg 2011;10:Doc03. [PubMed]
- Siddiqui MZ, Von Eyben FE, Spanos G. High-voltage irradiation and combination chemotherapy for malignant pheochromocytoma. Cancer 1988;62:686-90. [PubMed]
- Yu L, Fleckman AM, Chadha M, et al. Radiation therapy of metastatic pheochromocytoma: case report and review of the literature. Am J Clin Oncol 1996;19:389-93. [PubMed]
- van Hulsteijn LT, Niemeijer ND, Dekkers OM, et al. (131)I-MIBG therapy for malignant paraganglioma and phaeochromocytoma: systematic review and meta-analysis. Clin Endocrinol (Oxf) 2014;80:487-501. [PubMed]
- Erickson D, Kudva YC, Ebersold MJ, et al. Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. J Clin Endocrinol Metab 2001;86:5210-6. [PubMed]
- Ayala-Ramirez M, Palmer JL, Hofmann MC, et al. Bone metastases and skeletal-related events in patients with malignant pheochromocytoma and sympathetic paraganglioma. J Clin Endocrinol Metab 2013;98:1492-7. [PubMed]
- Luiz HV, da Silva TN, Pereira BD, et al. Malignant paraganglioma presenting with hemorrhagic stroke in a child. Pediatrics 2013;132:e1709-14.
- Mishra T, Goel NA, Goel AH. Primary paraganglioma of the spine: A clinicopathological study of eight cases. J Craniovertebr Junction Spine 2014;5:20-4. [PubMed]