Cervical spine immobilization in the elderly population
Introduction
For the past decades, immobilization of the spine has been a cornerstone in spinal injury management and trauma patients (1). The rationale underlying such an approach is that spinal injuries are not uncommon in the trauma setting, and thus immobilization of the spinal column will prevent or minimize further pathological damage to the spinal cord by vertebrae (2). However, there have been reports of neurologic deterioration occurring after the initial trauma, such as during transit or early management, ranging from 3–25% (1,3,4). As such, despite the common dogma and recommendations of spinal immobilization in the trauma setting, there is still controversy and a lack of high-powered clinical evidence to support these measures (5-9). Traumatic spinal column injuries generally occur over multiple vertebral levels. Prior to ruling out injury, to minimize further risk of damage, complete spinal immobilization has been recommended.
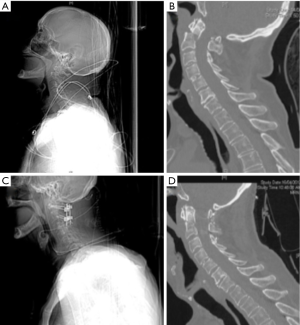
In the context of a suspected cervical spine injury, patients are immobilized in a “neutral position” based on the head and trunk resting on a flat surface (10,11). In the authors’ experience in a spinal injuries unit, elderly patients often have their cervical spine immobilized in an inappropriately over-extended position. This can lead to incorrect orthosis fitting, which may result in fracture displacement or exacerbated neurological injury (Figure 1).
It is hypothesized that the increased thoracic kyphosis and cervical hyperlordosis seen in elderly patients may require alternative cervical immobilization, compared with the standard “neutral” position. Therefore, the aim of the present study was to assess the morphology of the cervical spine in elderly patients presenting to a trauma spinal injuries unit at a major Australian tertiary institution.
Methods
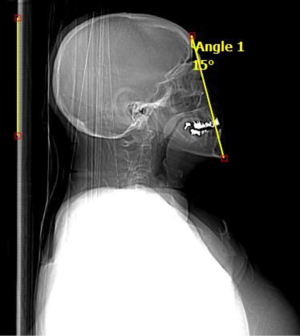
A retrospective audit of pan-scan computed tomography (CT) imaging of consecutive major trauma patients aged over 65 years was carried out over a 6-month period at the Royal North Shore Hospital (RNSH), Sydney, Australia. Utilizing the pan-CT’s localizing scout film, ‘chin-brow horizontal’ angles were independently measured by a senior spine surgeon (RJM) and a neurosurgeon (PJR) with the gantry used as a horizontal zero-degree reference. The benefit of the ‘chin-brow horizontal’ angle measure in the trauma setting is that the ‘chin-brow horizontal’ angle can be assessed from the bedside whilst the patient is immobilized against a flat surface. The ‘chin-brow horizontal’ angle was defined as the angle measured between a line from the brow to the chin to the horizontal (Figure 2).
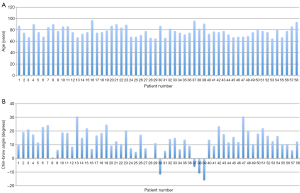
Interobserver reproducibility was calculated with a 95% confidence interval (CI). Correlations between measurements and between observers were evaluated by interclass correlation (ICC). An ICC of >0.75 was accepted as evidence of excellent agreement and a confirmation of measurement reliability. Statistical analysis was performed using SPSS, with data expressed in mean ± standard deviation (SD).
Results
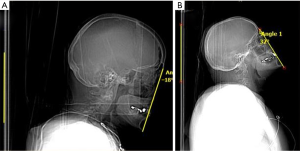
During the 6-month period, 58 patients were identified, including 30 males and 28 females, with an average age of 77.6 years (range, 65–97 years). The chin-brow angles varied widely from +15.8 degrees in flexion to −30.5 degrees in extension, with mean ‘chin-brow horizontal’ angle of −12.4 degrees in extension (SD: 9.31 degrees). The distribution of the patient age and ‘chin-brow horizontal’ angles are shown in Figure 3. The interobserver ICC was determined to be 0.997 (95% CI: 0.995–0.998). Examples of hyperlordotic and kyphotic cervical spines are shown in Figure 4.
Discussion
Despite being a commonly performed procedure in the trauma setting, there is a lack of convincing level I and II evidence to support routine spinal immobilization. Spinal immobilization was introduced with the aim of minimizing or preventing further exacerbation to injuries to the cervical nerve roots or spinal cord (12-15). However, cervical spine immobilization also has its disadvantages, including patient discomfort, respiratory compromise due to strapping techniques, skin ulcerations, dysphagia, as well as cost of equipment and training of relevant personnel (16). It has also been suggested that cervical hard collars significantly increase intracranial pressure after head injury (17). Therefore, it is in the patient’s best interests for spinal immobilization to be delivered appropriately and optimally.
Traditionally, the cervical spine was immobilized in the “neutral position” on a flatboard. Prior studies have suggested that positioning a patient on a flatboard places patients on relative cervical extension (10). Trauma guidelines have recognized certain situations where the flat board neutral position is inappropriate. These include the young infant, where a disproportionately large head leads to relative flexion, or the shoulder padded football player, where the elevation of the trunk leads to relative neck extension. Appropriate strategies for ameliorating these effects have been proposed. The increasing incidence of traumatic injuries in the elderly should prompt closer examination of this population. We hypothesized that degenerative changes in the elderly population, particularly the development of excessive thoracic kyphosis would lead to excessive neck extension when positioned on a flatboard.
We utilized a quick method to assess spinal alignment in the trauma setting—the ‘chin-brow horizontal’ angle. The chin-brow vertical angle is already commonly used in the assessment of kyphotic deformities in patients in with ankylosing spondylitis (18). We have developed a modification, the ‘chin-brow horizontal’ angle, for use in the trauma setting. This can be easily assessed on a CT scout image or from the bedside whilst the patient is immobilized against a flat surface. In the normal individual, the ‘chin-brow horizontal’ angle is close to zero. In this study, we found that the mean ‘chin-brow horizontal’ angle in immobilized trauma patients over 65 years of age was −12.4 degrees in extension, with significant variability (range, +15.8 degrees in flexion to −30.5 degrees in extension, Figure 2).
There are several potential explanations for the results of the present study. In elderly patients, the thoracic region often undergoes kyphotic changes. In this situation, to attain a flat board neutral position, the neck must be hyper-extended. There may also be a degree of pre-existing cervical hyperlordosis where, degenerative changes lead to a more kyphotic alignment. Some patients may have cervical hyperlordosis where, to compensate for degenerative changes, the head is often moved backwards to preserve forward gaze (19). Over time, this hyperlordosis stress on the cervical spine in tandem with degenerative changes may contribute to increasing cervical hyperlordosis (20). Our results suggest that cervical spine immobilization in slight flexion may be more appropriate to bring the patients to a true neutral position.
Another consideration is the injury pattern of elderly patients which may differ from a younger population. Elderly patients typically fall from a standing height, which may lead to injuries to the atlantoaxial complex, involving the dens of the axis and odontoid process (21). Such injuries typically occur following hyperextension of the neck and may lead to fractures and spinal deformities (22). Quick assessment of the chin-brow angles and the horizontal gaze of such patients may allow the healthcare professional to decide the optimal angle to immobilize the cervical spine in order to achieve the optimal neutral position. This may require an alteration in the design of the trauma flat board or design a ‘pillow’ to add to the flat board.
Limitations
All the limitations of a retrospective study apply to this study. It is a pilot study and a study with larger population is needed. The cervical alignment is in a trauma setting on a flat board, and does not mimic the natural cervical spine alignment.
Conclusions
The study describes the use of a novel measurement, the ‘chin-brow horizontal’ angle in the assessment of spinal alignment in trauma. The results suggest that, in elderly patients, the “neutral position” adopted for cervical spine immobilization may not be appropriate. We suggest that consideration be taken in cervical spine immobilization, with patients assessed on an individual basis on their fracture morphology and on the forward gaze position to minimize the risk of fracture displacement and worsened neurological deficit.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Theodore N, Hadley MN, Aarabi B, et al. Prehospital cervical spinal immobilization after trauma. Neurosurgery 2013;72 Suppl 2:22-34. [Crossref] [PubMed]
- Fehlings MG, Louw D. Initial stabilization and medical management of acute spinal cord injury. Am Fam Physician 1996;54:155-62. [PubMed]
- Eismont FJ, Currier BL, McGuire RA Jr. Cervical spine and spinal cord injuries: recognition and treatment. Instr Course Lect 2004;53:341-58. [PubMed]
- Fenstermaker RA. Acute neurologic management of the patient with spinal cord injury. Urol Clin North Am 1993;20:413-21. [PubMed]
- Kwan I, Bunn F, Roberts I. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev 2001.CD002803. [PubMed]
- Hauswald M, Hsu M, Stockoff C. Maximizing comfort and minimizing ischemia: a comparison of four methods of spinal immobilization. Prehosp Emerg Care 2000;4:250-2. [Crossref] [PubMed]
- Main PW, Lovell ME. A review of seven support surfaces with emphasis on their protection of the spinally injured. J Accid Emerg Med 1996;13:34-7. [Crossref] [PubMed]
- Connell RA, Graham CA, Munro PT. Is spinal immobilisation necessary for all patients sustaining isolated penetrating trauma? Injury 2003;34:912-4. [Crossref] [PubMed]
- Domeier RM, Frederiksen SM, Welch K. Prospective performance assessment of an out-of-hospital protocol for selective spine immobilization using clinical spine clearance criteria. Ann Emerg Med 2005;46:123-31. [Crossref] [PubMed]
- Schriger DL, Larmon B, LeGassick T, et al. Spinal immobilization on a flat backboard: does it result in neutral position of the cervical spine? Ann Emerg Med 1991;20:878-81. [Crossref] [PubMed]
- Nypaver M, Treloar D. Neutral cervical spine positioning in children. Ann Emerg Med 1994;23:208-11. [Crossref] [PubMed]
- McGuire RA Jr. Protection of the unstable spine during transport and early hospitalization. J Miss State Med Assoc 1991;32:305-8. [PubMed]
- Garfin SR, Shackford SR, Marshall LF, et al. Care of the multiply injured patient with cervical spine injury. Clin Orthop Relat Res 1989.19-29. [PubMed]
- Moylan JA. Trauma injuries. Triage and stabilization for safe transfer. Postgrad Med 1985;78:166-71, 174-5, 177. [PubMed]
- Toscano J. Prevention of neurological deterioration before admission to a spinal cord injury unit. Paraplegia 1988;26:143-50. [Crossref] [PubMed]
- Haut ER, Kalish BT, Efron DT, et al. Spine immobilization in penetrating trauma: more harm than good? J Trauma 2010;68:115-20; discussion 120-1. [Crossref] [PubMed]
- Mobbs RJ, Stoodley MA, Fuller J. Effect of cervical hard collar on intracranial pressure after head injury. ANZ J Surg 2002;72:389-91. [Crossref] [PubMed]
- Suk KS, Kim KT, Lee SH, et al. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine (Phila Pa 1976) 2003;28:2001-5. [Crossref] [PubMed]
- Leigh JH, Cho K, Barcenas CL, et al. Dysphagia aggravated by cervical hyperlordosis. Am J Phys Med Rehabil 2011;90:704-5. [Crossref] [PubMed]
- Mori K, Nishizawa K, Nakamura A, et al. Atraumatic Occult Odontoid Fracture in Patients with Osteoporosis-Associated Thoracic Kyphotic Deformity: Report of a Case and Review of the Literature. Case Rep Orthop 2015;2015:301858.
- Lomoschitz FM, Blackmore CC, Mirza SK, et al. Cervical spine injuries in patients 65 years old and older: epidemiologic analysis regarding the effects of age and injury mechanism on distribution, type, and stability of injuries. AJR Am J Roentgenol 2002;178:573-7. [Crossref] [PubMed]
- Walid MS, Zaytseva NV. Upper cervical spine injuries in elderly patients. Aust Fam Physician 2009;38:43-5. [PubMed]


