Comparison of surgical outcomes after anterior cervical discectomy and fusion: does the intra-operative use of a microscope improve surgical outcomes
Introduction
Since the advent of the anterior approach to the cervical spine, several modifications to the surgical technique including refinements made by Cloward in 1958 and Bailey-Badgley in 1960 have been described (1-5). In 1975, Hankinson and Wilson were the first to describe their experience with the use of the operating microscope for anterior cervical discectomy without fusion (5,6). The authors reported their experience with 51 patients undergoing anterior cervical discectomy without fusion and noted superior visualization of surgical anatomy, which facilitated a safer operation and more extensive decompression of neural elements (5). Whether the use of the intra-operative microscope portends a more extensive decompression with fewer intra-operative complications and superior long-term outcomes remains unknown.
The primary aim of this study was to assess and compare the complications profile as well as long-term clinical outcomes between patients undergoing an ACDF procedure with and without the use of an intra-operative microscope.
Methods
Patient selection
We queried a prospectively maintained data registry at a major academic institution. Institutional Review Board approval was obtained prior to study initiation. We included patients aged 18 years and older, (I) who presented with neck pain, radiculopathy or myelopathy; (II) underwent anterior cervical discectomy and fusion (ACDF) with or without the use of a surgical microscope; and (III) had available patient reported outcomes measures at baseline, 3-, 6-, 12-, and 24-month after surgery. Patients were excluded if they had (I) prior ACDF or (II) severe co-existent pathology that could confound the assessment of operative outcome (e.g., rheumatoid arthritis, osteoarthritis, metabolic bone disease).
Immediate postoperative complications
We assessed postoperative complications for each patient included in the study. Complications were divided into those likely or possibly associated with the surgery, including nerve root injury, durotomy, surgical site drainage or infection and reoperation. Other complications known to be associated with ACDF surgery [e.g., pulmonary embolism (PE)/deep vein thrombosis (DVT)] were also assessed.
Patient reported outcomes
Neck pain was assessed using the neck-pain visual analog scale (NP-VAS), and functional status was assessed using the neck disability index (NDI) and short-form 12 (SF-12) physical component score (PCS). The SF-12 mental component score (MCS) was used for the assessment of mental health status. These questionnaires have been validated, widely used and accepted in spine research.
Statistical analysis
We compared patient and surgical variables, pain measures and functional status between patients undergoing ACDF with and without the use of an operating microscope. Demographic variables evaluated included patient age, gender, and body mass index (BMI). Co-morbidities included hypertension, diabetes, hyperlipidemia (HLD), coronary artery disease (CAD), and myocardial infarction (MI). Surgical variables included number of vertebral levels treated, duration of surgery, and estimated blood loss (EBL).
Parametric data was expressed as means ± standard deviation (SD) and compared via the student test. Nonparametric data was expressed as median [interquartile range (IQR)] and compared via the Mann-Whitney U test. Nominal data was compared with the Chi-square test. All tests were two-sided and were statistically significant if the P value was less than 0.05.
Results
One hundred and forty patients (microscope cohort: n=59; non-microscope cohort: n=81) were enrolled in this study. We included patients 18 years and older with both clinical and radiographic indications for ACDF, and available 3-, 6-, 12-, and 24-month follow-up data. We excluded patients that had prior ACDF surgery or severe co-existent pathologies that could confound their perception of functional improvement.
There was no significant difference in age between both groups (microscope cohort: 54.50±13.29 years vs. non-microscope cohort: 51.62±12.9 years, P=0.20. Furthermore, there was no significant difference in BMI between both groups (microscope cohort: 27.78±6.14 kg/m2vs. non-microscope cohort: 29.60±7.66 kg/m2, P=0.12. More men were included in the Microscope cohort (52.54%) compared to the Non-microscope cohort (41.97%), Table 1. There were no co-morbidity differences in hypertension, diabetes, HLD, CAD, MI, or smoking status between both groups, Table 1.
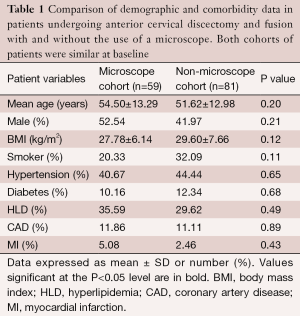
Full table
Pre-operative baseline patient-reported outcome measures
At baseline, there was no significant difference in baseline functional status between both groups. The mean ± SD NP-VAS score for the Microscope and Non-microscope cohort was 4.85±2.93 and 4.88±3.35, P=0.95, respectively, Table 2. The pre-operative mean ± SD NDI score for the Microscope- and Non-microscope cohort was 54.50±13.29 and 51.62±12.98, P=0.20, respectively, Table 2. The mean ± SD SF-12 PCS score for the Microscope- and Non-microscope cohort was 32.94±9.51 and 31.72±8.50, P=0.56, respectively, Table 2. The mean ± SD SF-12 MCS score for the Microscope cohort and Non-microscope cohort was 43.46±12.57 and 42.20±12.16, P=0.66, respectively, Table 2.
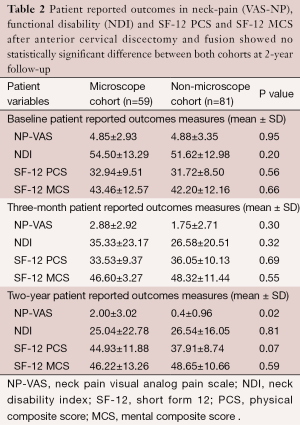
Full table
Post-operative complications profile
The only significant difference between the two groups was the duration of surgery; the mean ± SD duration of surgery (minutes) for the microscope- and non-microscope cohort was 169.34±50.79 and 98.03±42.36 minutes, P=0.01, respectively, Table 3. The mean ± SD EBL (mL) for the microscope- and non-microscope cohort was 129.31±270.00 and 78.33±151.91 mL P=0.21, respectively, Table 3.
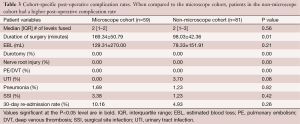
Full table
Overall, the incidence of post-operative complications was similar in both groups, Table 3. There was no incidental durotomy or nerve root injury in either cohort. In total, 3 patients had a surgical site infection (Microscope cohort: 3.38% vs. Non-microscope 1.23%, P=0.42). There were 3 patients with urinary tract infections (UTI) (Microscope cohort: 0% vs. Non-microscope: 3.7% P=0.08), and 2 patients who had pneumonia (microscope cohort: 1.69% vs. non-microscope 1.23%, P=0.82), Table 3. No patient had a peri-operative PE/DVT, Table 3.
There was no statistically significant difference between both cohorts in all patient-reported outcome metrics 3 months after ACDF with and without the use of a surgical microscope, Table 2. At 3 months, the mean ± SD NP-VAS for the microscope and non-microscope cohort was 2.88±2.92 and 1.75±2.71, P=0.30, respectively, Table 2. The mean ± SD NDI for the Microscope and Non-microscope cohort was 35.33±23.17 and 26.58±20.51 P=0.32, respectively, Table 2. The mean ± SD SF-12 PCS for the Microscope and Non-microscope cohort was 33.53±9.37 and 36.05±10.13, P=0.69, respectively, Table 2. The mean ± SD SF-12 MCS for the microscope cohort and non-microscope cohort was 46.60±3.27 and 48.32±11.44, P=0.55, respectively, Table 2.
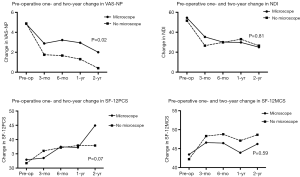
There was no statistically significant difference between the two cohorts in patient-reported outcomes measures, 2 years after index surgery (Figure 1). The mean ± SD NDI for the Microscope and Non-microscope cohort was 25.04±22.78 and 26.54±16.05, P=0.81, respectively, Table 2. The mean ± SD SF-12 PCS for the Microscope and Non-microscope cohort was 44.93±11.88 and 37.91±8.74, P=0.07, respectively, Table 2. The mean ± SD SF-12 MCS for the Microscope and Non-microscope cohort was 46.22±13.26 and 48.65±10.66, P=0.59, respectively, Table 2.
Discussion
In this 2-year longitudinal cohort analysis of ACDF with and without the use of the operating microscope, we demonstrate that there are no significant differences in the complications profile or the long-term outcomes with and without the use of an intra-operative microscope. As expected, the duration of surgery was longer in the microscope compared to the non-microscope cohort.
As ACDF procedures have been shown to be a safe and clinically effective treatment, these procedures are great comparator for examining the efficacy of different surgical techniques and equipment. ACDF has been used as a gold-standard treatment for cervical radiculopathy and myelopathy (7-9). Most ACDF procedures are performed without the use of an intra-operative microscope. Cauthen et al. in a study of 348 patients undergoing single and multilevel ACDF’s without the use of an intra-operative microscope demonstrated good outcomes in the majority of patients (10). The authors found, with a minimum of a 2-year follow-up, that 78% of the patients were satisfied with their outcomes, and 83% of the patients were able to return to work (10). Furthermore, the authors identified 2,037 patients in a literature review, from 1975 to 1996, who underwent an ACDF without the use of an intra-operative microscope and found that there was an overall fusion success rate of 92% (10). Analogous to this study, we found no differences in the complications profiles and long-term outcomes between both microscope and non-microscope cohorts.
ACDF procedures performed with the use of an operative microscope have also shown successful long-term with low complications profiles. Omidi-Kashani et al. in a recent study of 74 patients undergoing ACDF’s with the use of an intra-operative microscope demonstrated excellent outcomes in the majority of patients (11). Under Odom’s criteria, the authors found that 89.7% of patients reported functional outcomes as either good or excellent (11,12). NDI and visual analog scale (VAS) were also significantly improved, 31 months after index surgery (11). Wirth et al. in an earlier study of 25 patients undergoing ACDF’s with the use of an intra-operative microscope demonstrated successful outcomes in all of the patients (13). The authors found that 100% of the patients indicated pain improvement 2 months post-operatively (13). Furthermore, 96% of the patients returned to work by 2 months and 81% remained at work, 69 months after index surgery (13).
The duration of surgery appears to be longer with the use of an intra-operative microscope. In a recent study of 116 thyroidectomies with and without the use of an intraoperative microscope, Davidson and colleagues reported a significant increase (P<0.001) of 30 minutes in procedures with the use of an intra-operative microscope (14). The authors attributed the increased operative time to the time used to adjust the microscope for visualization of the surgical field (14).
Along with the increase in length of surgery, there is also an increase in surgical cost with the use of an intra-operative microscope. In a recent systematic review of 10 ACDF studies, Alvin colleagues observed that direct costs ranged from $5,396 to $29,898; with increased costs of surgical instruments and longer duration of surgery consistently associated with increased total cost of surgery (15). Damodaran et al. in a recent review suggested that one of the prime limitations of using an operating microscope for spine surgery is the expensive cost; however, the authors suggest that the cost benefit may be worth the better surgical outcomes (16).
This study has limitations, ensuing possible implications for its interpretation. While pre- and perioperative variables were prospectively recorded into the study registry at the time of surgery, these variables were retrospectively analyzed for the purposes of this study and are subject to the weaknesses of a retrospective analysis. Additionally, the duration of symptoms preoperatively could not be assessed and could presumably impact the patient-reported outcomes. Despite these limitations, this study has demonstrated that the use of an intra-operative microscope does not lead to superior outcomes.
Conclusions
The intra-operative use of a microscope enhances the visualization of surgical anatomy, however, the results of this study indicate that it does not improve overall surgery-related outcomes, nor does it lead to superior long-term outcomes in pain and functional disability, 2 years after index surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Baskin DS, Ryan P, Sonntag V, et al. A prospective, randomized, controlled cervical fusion study using recombinant human bone morphogenetic protein-2 with the CORNERSTONE-SR allograft ring and the ATLANTIS anterior cervical plate. Spine (Phila Pa 1976) 2003;28:1219-24; discussion 1225. [Crossref] [PubMed]
- Papadopoulos EC, Huang RC, Girardi FP, et al. Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine (Phila Pa 1976) 2006;31:897-902. [Crossref] [PubMed]
- Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg 1958;15:602-17. [Crossref] [PubMed]
- Madawi AA, Powell M, Crockard HA. Biocompatible osteoconductive polymer versus iliac graft. A prospective comparative study for the evaluation of fusion pattern after anterior cervical discectomy. Spine (Phila Pa 1976) 1996;21:2123-9; discussion 2129-30. [Crossref] [PubMed]
- Nandoe Tewarie RD, Bartels RH, Peul WC. Long-term outcome after anterior cervical discectomy without fusion. Eur Spine J 2007;16:1411-6. [Crossref] [PubMed]
- Hankinson HL, Wilson CB. Use of the operating microscope in anterior cervical discectomy without fusion. J Neurosurg 1975;43:452-6. [Crossref] [PubMed]
- Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431-4. [Crossref] [PubMed]
- Korinth MC. Treatment of cervical degenerative disc disease - current status and trends. Zentralbl Neurochir 2008;69:113-24. [Crossref] [PubMed]
- Muheremu A, Niu X, Wu Z, et al. Comparison of the short- and long-term treatment effect of cervical disk replacement and anterior cervical disk fusion: a meta-analysis. Eur J Orthop Surg Traumatol 2015;25 Suppl 1:S87-100. [Crossref] [PubMed]
- Cauthen JC, Kinard RE, Vogler JB, et al. Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine (Phila Pa 1976) 1998;23:188-92. [Crossref] [PubMed]
- Omidi-Kashani F, Ghayem Hasankhani E, Ghandehari R. Impact of Age and Duration of Symptoms on Surgical Outcome of Single-Level Microscopic Anterior Cervical Discectomy and Fusion in the Patients with Cervical Spondylotic Radiculopathy. Neurosci J 2014;2014:808596.
- Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc 1958;166:23-8. [Crossref] [PubMed]
- Wirth FP, Dowd GC, Sanders HF, et al. Cervical discectomy. A prospective analysis of three operative techniques. Surg Neurol 2000;53:340-6; discussion 346-8. [Crossref] [PubMed]
- Davidson BJ, Guardiani E, Wang A. Adopting the operating microscope in thyroid surgery: safety, efficiency, and ergonomics. Head Neck 2010;32:154-9. [PubMed]
- Alvin MD, Miller JA, Lubelski D, et al. Variations in cost calculations in spine surgery cost-effectiveness research. Neurosurg Focus 2014;36:E1. [Crossref] [PubMed]
- Damodaran O, Lee J, Lee G. Microscope in modern spinal surgery: advantages, ergonomics and limitations. ANZ J Surg 2013;83:211-4. [Crossref] [PubMed]


