Transpedicular endoscopic surgery for lumbar spinal synovial cyst—report of two cases
Introduction
Lumbar facet cysts are a degenerative phenomenon and relatively uncommon cause for nerve root decompression. The cysts arise from the synovium of the facet joint and most often occur at the lumbar 4–5 level. The standard surgical treatment when conservative treatment has failed is a laminectomy and partial facetectomy to access the cyst which is typically found at the medial border of the facet joint (1). Minimally invasive techniques have been described and include cyst aspiration, resection through a tubular retractor by ipsilateral (2) or contralateral approach (3), and endoscopic cyst resection through a transforaminal or interlaminar approach (4). Herein we describe a novel transpedicular endoscopic approach for accessing lumbar facet cysts that are not easily accessible through a transforaminal or interlaminar approach because they arise medial to the pedicle.
Case presentation
Case 1
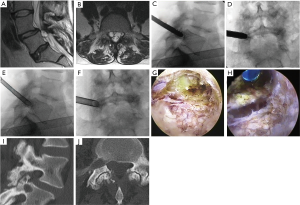
This 34-year-old woman presented with 1 year of back pain and three months of right lower extremity radicular pain in a L5 distribution and weakness in right foot and great toe dorsiflexion. Conservative treatment included epidural steroid injections and physical therapy. MRI lumbar spine (Figure 1A,B) demonstrated a right L4–5 facet cyst medial to the right L5 pedicle and a grade I spondylolisthesis. The patient refused open surgery and refused the possibility of a fusion procedure. Because of the location of the cyst, a transpedicular endoscopic approach was pursued (Figure 1C-F). Intraoperatively the yellow cyst was evident after making a hole in the pedicle (Figure 1G). After piecemeal removal of the cyst, the free floating L5 nerve was observed (Figure 1H). Immediately postoperatively the patient’s radicular pain was gone and her foot and toe dorsiflexion strength was improved. A CT lumbar spine performed the day after surgery showed no pedicle fracture (Figure 1I,J).
Case 2
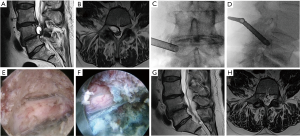
This 67-year-old male presented with 20 years of low back pain and 1 year of being only able to walk 50 meters due to pain in the right leg. The patient also suffers from diabetes, hypertension, and coronary artery disease. On examination he had a foot drop with only antigravity strength in right foot dorsiflexion. Lumbar MRI showed a large right facet cyst behind the pedicle of L4 with severe fact arthrosis and disc bulges at L3–4 and L4–5 (Figure 2A,B). The patient had tried physical therapy and interventional pain management and was considered high risk for surgery by his cardiologist. Because of his high risk for open surgery, a transpedicular endoscopic approach was pursued. Chromodiscography was performed during his procedure at L3–4 and L4–5 to help distinguish disc pathology from cyst intraoperatively, and the transpedicular endoscopic access is demonstrated in Figure 2C,D. After transpedicular cyst decompression (Figure 2E-H) the patient recovered rapidly with immediate relief of his radicular pain and complete resolution of his foot drop by six months. A lumbar spine MRI performed three months after surgery demonstrated a free spinal canal with resolution of the cyst but continued severe degeneration (Figure 2G,H).
Operative technique
For the transpedicular endoscopic procedure the patient was positioned in that lateral decubitus position. The procedure was done under local analgesia and intravenous sedation; the level of anesthetic was titrated so the patient was able to communicate with the surgeon throughout the procedure. The Joimax® TESSYS endoscopic system with reamer and drill technique was used for the procedure. Percutaneous entry was established entering through the skin 12 cm lateral to the midline for the pedicle of L5 and 11 cm lateral to the pedicle for L4. Using intermittent fluoroscopic guidance, alternating between lateral and anterior-posterior (AP) view, a 25 cm 18 gauge needle was advanced and placed at the lateral pedicle between vertebral body and transverse process. After feeling the needle contact the bone, fluoroscopy confirmed the needle position in AP and lateral views. The needle was then replaced by a K-wire. A 6 mm skin incision was made over the needle, and sequential dilators of 4 and 8 mm were inserted down to the pedicle. Sequential dilators were removed and with the guidance of the K-wire, the Yamshidi needle was inserted down to the pedicle under fluoroscopic guidance. The access point for the Yamshidi needle is the middle of the pedicle in the AP and lateral views. The success of surgery depends on the accuracy of the targeting at this point. Penetrating the full width of the pedicle is done by simultaneously feeling by hand and using fluoroscopic confirmation. The loss of resistance and sometimes leg pain of the patient indicate that the pedicle has been penetrated. The Yamshidi needle can be replaced by 2 mm K-wire and disposable bone drill of 4 mm. The small bone hole is then increased in size by a step by step fashion with reamers and drills of increasing diameter from 5 to 8 mm (Figure 1C,D). After making a hole of 8 mm through the pedicle a final 7.2 mm tubular retractor is inserted (Figures 1E,F,2C,D). Before endoscopy in case 2 an additional puncture of the disk below and above the pedicle was made with a mixture of contrast medium (Solutrast® 3 mL) and Toluidinblau® blue dye (0.1 mL) (Figures 1I,J,2E,F). At this point the Joimax® GmbH endoscope with a 3.8 mm working channel is inserted through the tubular retractor. Under endoscopic visualization the facet cyst can be seen (Figures 1G,2E). Straight and bendable forceps are used to carefully remove the facet cyst and decompress the nerve and successful decompression is accomplished when the nerve root is seen floating freely in the epidural space (Figures 1H,2F) and when the patient is able to communicate that their preoperative symptoms have been relieved. The working channel and scope were removed, pressure was held on the 6 mm incision for 5 minutes, and the wound was closed with a single interrupted suture.
Discussion
The risks of operating on lumbar facet cysts include spinal fluid leak, cyst recurrence, and destabilization of the lumbar segment requiring later fusion. Drilling through the pedicle to access the facet cyst as described here may avoid significant facet removal that further destabilizes the lumbar motion segment but is not recommended as a replacement for other open, minimally invasive, or endoscopic surgical techniques because drilling through the pedicle to access the cyst pathology creates the potential danger of a destabilizing pedicle fracture. Cadaver and radiologic examinations reveal that the lumbar pedicle is longer and narrower at L1 and becomes gradually shorter and wider down the lumbar spine to L5 (5). Females also have slightly smaller pedicles [5]. Torun et al. found the widest lumbar pedicle was measured at L5 as 17.1±4.2 mm and the narrowest at L1 as 8.4±1.8 mm (5). That is why we would reserve transpedicular access only for L3–5 in males and L4 and L5 in females. The outer diameter of the tubular retractor for the endoscope used here is 7.5 mm, which sets up the anatomic constraint limiting which pedicles are appropriate for a transpedicular approach. Reaming or drilling a pedicle of insufficient width poses the risk of fracturing that pedicle. The technique illustrated in this case report is only suggested as a possible alternative for those experienced endoscopic spine surgeons to consider in a very select patient population.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Freidberg SR, Fellows T, Thomas CB, et al. Experience with symptomatic spinal epidural cysts. Neurosurgery 1994;34:989-93; discussion 993. [Crossref] [PubMed]
- Sandhu FA, Santiago P, Fessler RG, et al. Minimally invasive surgical treatment of lumbar synovial cysts. Neurosurgery 2004;54:107-11; discussion 111-2. [Crossref] [PubMed]
- Rhee J, Anaizi AN, Sandhu FA, et al. Minimally invasive resection of lumbar synovial cysts from a contralateral approach. J Neurosurg Spine 2012;17:453-8. [Crossref] [PubMed]
- Komp M, Hahn P, Ozdemir S, et al. Operation of lumbar zygoapophyseal joint cysts using a full-endoscopic interlaminar and transforaminal approach: prospective 2-year results of 74 patients. Surg Innov 2014;21:605-14. [Crossref] [PubMed]
- Torun F, Tuna H, Buyukmumcu M, et al. The lumbar roots and pedicles: a morphometric analysis and anatomical features. J Clin Neurosci 2008;15:895-9. [Crossref] [PubMed]


