Practical implications of the lumbar spine and its function on total hip arthroplasty
Optimal placement of components is of significant importance in total hip arthroplasty (THA), aiming to avoid complications such as wear or dislocation (1). Acetabular cup placement has traditionally been referenced from the Lewinnek plane, a plane intersecting the anterior superior iliac spines and the pubic tubercles. Surgeons often target a ‘safe zone’ [also known as the Lewinnek zone] for acetabular orientation, defined as being in 15 degrees (±10°) of anteversion, and 40 degrees (±10°) of inclination (2). Navigated systems (allowing intraoperative placement quantification) and some patient-specific methods (where components are implanted based on jigs constructed from pre-operative three-dimensional imaging) also target the Lewinnek zone, and have been shown to result in more accurate placement compared to traditional freehand techniques, as well as diminished dislocation rates (3,4).
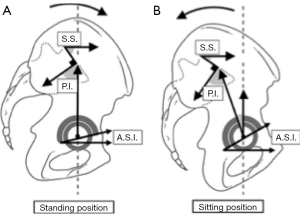
However, there is evidence that the Lewinnek zone is variable, between and within patients. This variability stems from the interplay between lumbar spine orientation and pelvic rotation, which results in alterations in pelvic position. This relationship is best demonstrated by the fact that pelvic incidence (PI) is equal to the sum of sacral slope (SS, the angle subtended by the axial plane of the superior sacrum and the horizontal) and pelvic tilt (PT, the angle subtended by a line between the sacral plate to the midpoint of the femoral head and the vertical). An increase in SS corresponds with a posterior tilt of the pelvis (5). As PI is fixed (between 48 and 53 degrees) (6,7), it follows that SS and PT are co-dependent.
In particular, Philippot et al. demonstrated the Lewinnek plane variations between sitting and standing, with cumulative imprecisions of up to 26 degrees when standing and 36 degrees in the supine position, and concluded that it may not be an ideal landmark (8). This phenomenon is a consequence of pelvic rotation about the bicoxofemoral axis resulting in either anterior or posterior tilt of the pelvis, which alters the optimal coronal orientation dictated by the Lewinnek plane (9).
Lazennec et al. and Pierrepont et al. have further quantified the variations in pelvic position in different postural environments (9,10).
In the upright position, the pelvis tilts posteriorly, whilst when supine, the pelvis is anteriorly tilted (11). These inherent transitions in PT confer a degree of variability to acetabular positioning and stability. Pelvic anteversion in the upright position is associated with a decrease in sagittal and coronal tilt of the acetabulum compared to when there is posterior PT as seen in the seated position (Figure 1). Variations have been reported at up to 14 degrees for anterior sagittal inclination and 7 degrees for frontal inclination of the acetabulum, creating a more vertically oriented cup in the seated position compared to standing (11). Functionally, this results in the range of movement arc shifting to a position of flexion when seated when the pelvis is tilted posteriorly due to an increase in acetabular sagittal inclination (ASI). This creates functional limitation, as in the standing close-packed position, the patient is in a greater degree of extension at the hip joint compared to normal, with potential posterior impingement and increased risk of anterior dislocation (9,12,13).
Disturbances to the hip-spine relationship have obvious functional ramifications. In particular, when a diseased spine is unable to undergo its regular arc of motion, the pelvic-spinal unit is unable to compensate for the positional variation experienced between the seated, supine and standing positions. Long-term age-related degeneration of the spine can induce hypolordotic posture, resulting in an increase in posterior tilt by up to 5 degrees, therefore increasing the risk of post-operative impingement and dislocation (14), suggesting that lumbar spine disease potentially worsens the outcome of THA. Buckland et al. [2015] suggest that this subset of THA patients require careful co-ordination and communication between spine and hip surgeons, after demonstrating marked reduction in PT and thus acetabular anteversion in patients with existing THAs receiving sagittal correction of their lumbar spine deformities (15). Data regarding patients with ankylosing spondylitis receiving THA’s further confirms the spino-pelvic relationship, with acetabular anteversion reported to be in excess of 10 degrees greater than the normal “recommended” maximum of 45 degrees, conferring a much greater risk of dislocation (16). However, it should be noted that abnormal pelvic motion has also been detected in a subset of subjects without any obvious lumbar deformity, so normal lumbar kinematics does not necessarily suggest normal pelvic motion.
The complex hip-spine relationship also has ramifications pre-operative planning and patient education. The lumbar spine range of motion should be factored into the decision-making process when determining the appropriate acetabular cup positioning. Patients with abnormalities of the lumbar spine, restrictions in movement or a history of lumbar spine arthrodesis should be considered for increased risk of dislocation. Additionally, computed tomography (CT) images traditionally taken to plan CT-navigated hip arthroplasty are in the supine position, and may not be representative of the true functional acetabular position. Au et al. assessed acetabular position post-operatively with supine and standing radiographs and demonstrated that despite being in the “safe zone” when assessed in the supine position, almost half of hips were outside these parameters when imaged in the standing position (17). In the context of investigating complications of THA post-operatively, standing radiographs may be more useful than supine images when assessing potential causes, particularly in the context of recurrent dislocation.
An understanding of the implications of the complex interaction between the lumbar spine and pelvic kinematics have allowed for the development of practical tools which use a more “patient specific” paradigm when determining ideal acetabular component placement. Novel pre-operative planning tools have surfaced which are able to factor in patient-specific anatomy in the seated and sitting positions to determine the optimal angles and component placement on a case by case basis (18). Patient-specific acetabular guides have been developed and are able to perform at a satisfactory level of accuracy and reliability with regards to the placement of the acetabular cup (19), although the clinical verification of the purported improvement in functional outcomes is yet to be published.
Conclusions and practical recommendations
It is well-established that lumbar spine alignment, position and physiology have definite consequences on pelvic rotation and acetabular positioning. This has practical ramifications for hip surgeons, who should pay particular attention to the functional capacity of patients’ lumbar spine when planning for THA, as there is a definite and complex kinematic between the two. In particular, patients with any evidence of lumbar spine deformity or pathology are at greater risk of dislocation and poorer outcomes. Comprehensive pre-operative assessment of this relationship allows for a more patient-specific approach to component placement, which may potentially improve functional outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: J Pierrepont is a paid employee for Corin Group. W Bruce has received research support for Corin Group. And other authors have no conflicts of interest to declare.
References
- Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 2009;91:128-33. [Crossref] [PubMed]
- Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978;60:217-20. [Crossref] [PubMed]
- Verdier N, Billaud A, Masquefa T, et al. EOS-based cup navigation: Randomised controlled trial in 78 total hip arthroplasties. Orthop Traumatol Surg Res 2016;102:417-21. [Crossref] [PubMed]
- Xu K, Li YM, Zhang HF, et al. Computer navigation in total hip arthroplasty: a meta-analysis of randomized controlled trials. Int J Surg 2014;12:528-33. [Crossref] [PubMed]
- Phan D, Bederman SS, Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J 2015;97-B:1017-23. [Crossref] [PubMed]
- Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 2006;15:415-22. [Crossref] [PubMed]
- Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99-103. [Crossref] [PubMed]
- Philippot R, Wegrzyn J, Farizon F, et al. Pelvic balance in sagittal and Lewinnek reference planes in the standing, supine and sitting positions. Orthop Traumatol Surg Res 2009;95:70-6. [Crossref] [PubMed]
- Lazennec JY, Brusson A, Rousseau MA. Hip-spine relations and sagittal balance clinical consequences. Eur Spine J 2011;20 Suppl 5:686-98. [Crossref] [PubMed]
- Pierrepont JW, Feyen H, Miles BP, et al. Functional orientation of the acetabular component in ceramic-on-ceramic total hip arthroplasty and its relevance to squeaking. Bone Joint J 2016;98-B:910-6. [Crossref] [PubMed]
- Lazennec JY, Boyer P, Gorin M, et al. Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res 2011;469:1103-9. [Crossref] [PubMed]
- Stephens A, Munir S, Shah S, et al. The kinematic relationship between sitting and standing posture and pelvic inclination and its significance to cup positioning in total hip arthroplasty. Int Orthop 2015;39:383-8. [Crossref] [PubMed]
- Kanawade V, Dorr LD, Wan Z. Predictability of Acetabular Component Angular Change with Postural Shift from Standing to Sitting Position. J Bone Joint Surg Am 2014;96:978-86. [Crossref] [PubMed]
- Esposito CI, Miller TT, Kim HJ, et al. Does Degenerative Lumbar Spine Disease Influence Femoroacetabular Flexion in Patients Undergoing Total Hip Arthroplasty? Clin Orthop Relat Res 2016;474:1788-97. [Crossref] [PubMed]
- Buckland AJ, Vigdorchik J, Schwab FJ, et al. Acetabular Anteversion Changes Due to Spinal Deformity Correction: Bridging the Gap Between Hip and Spine Surgeons. J Bone Joint Surg Am 2015;97:1913-20. [Crossref] [PubMed]
- Tang WM, Chiu KY. Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthroplasty 2000;15:52-8. [Crossref] [PubMed]
- Au J, Perriman DM, Neeman TM, et al. Standing or supine x-rays after total hip replacement - when is the safe zone not safe? Hip Int 2014;24:616-23. [Crossref] [PubMed]
- Marel E, Walter L, Solomon M, et al. Patient-specific acetabular cup orientation in functional positions using musculoskeletal modelling: a pre-operative planning tool. Orthopaedic Proceedings 2016;98-B:19.
- Spencer-Gardner L, Pierrepont J, Topham M, et al. Patient-specific instrumentation leads to accurate acetabular component placement in total hip arthroplasty. Bone Joint J 2016;98-B:1342-6. [Crossref] [PubMed]


