Enterococcus faecalis causing delayed spondylodiscitis in a case with retained intraspinal bullet
Introduction
Incidence of gunshot wounds (GSW) to the spine have shown a tremendous increase and are reported to be the third leading cause of spinal cord injury, after road traffic accidents and falls from height (1-4). Although military GSW with spine injuries are more common, civilian GSW are now reported more frequently (2-4).
Frequently gunshot injuries to the spine present immediately following the event with features of neurological dysfunction (1-3). They have a high incidence of wound infection especially when they are accompanied by large bowel perforations (5-7). Delayed presentation following gunshot injuries are reported less frequently and result in late onset neurological dysfunction due to migration of retained projectile and lead intoxication (8-10). We present a unique late onset presentation following a civilian GSW with colonic perforation that presented 4months following injury with late onset spondylodiscitis associated with a retained intraspinal bullet.
Case presentation
A 55-year-old male presented 4 months following a low velocity GSW to the abdomen which resulted in a caecal perforation and multiple tears in the ascending colon without neurological dysfunction. The patient was treated for the colonic injury with exploratory laparotomy, peritoneal lavage and ileotransverse colon anastomosis. The projectile after traversing the colon fractured the L5 vertebra and was lodged in the spinal canal at the level of S1 and was left in situ following the surgery for the colon injury. The patient was subsequently discharged 3 weeks following injury with no evidence of wound infection. The patient was asymptomatic for about 3 months and then developed progressive low back pain with neurogenic claudication and presented 4 months following initial treatment for GSW with retained intraspinal canal bullet at S1 level. The examination revealed paraspinal spasm with restriction of all range of movements of the lumbar spine. The motor power, sensory system, bowel and bladder function and distal arterial pulsations were normal.
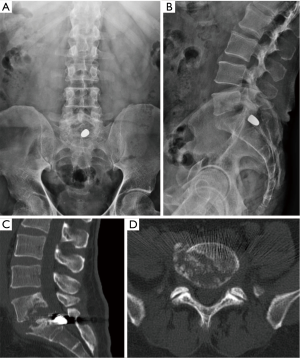
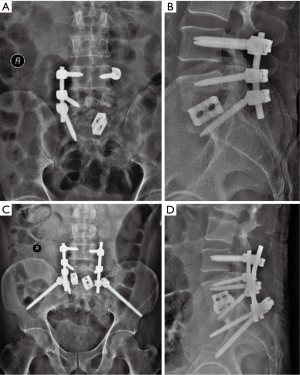
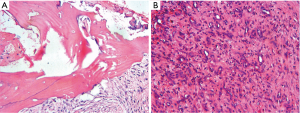
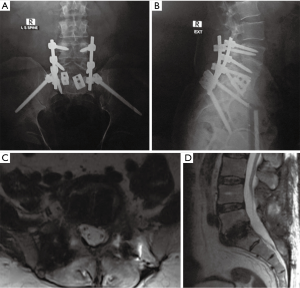
The patient was investigated with a plain radiograph and CT scan of the lumbar spine which showed the bullet with dense artefacts within the spinal canal at S1 level. (Figure 1). There was evidence of destruction of the L5–S1 endplates and subchondral bone with adjoining sclerosis suggesting a possibility of spondylodiscitis. A MRI scan though desirable was not performed for risk of migration of projectile and neurological deterioration. There was considerable destruction of the L5 right vertebral body involving more than 50% of the height. The patient underwent surgery for extraction of projectile and debridement of the infective focus (Figure 2). The patient underwent unilateral pedicular screw fixation from L4 to S1 with debridement of the disc space and temporary titanium cage was used to reconstruct the anterior column (Figure 3). Definitive fusion was deferred at this point. The tissue culture from the L5–S1 disc space isolated Enterococcus faecalis species. The patient was started on appropriate antibiotics as per sensitivity and underwent a second stage circumferential fusion 14 days later using titanium interbody cages, autologous bone grafting and posterior instrumented stabilization from L4 to ilium (Figure 3). The histopathological examination was suggestive of a pyogenic spondylodiscitis (Figure 4). The patient was treated with antibiotics for a 4-week period and discharged. The patient made an eventful recovery with no implant failure, migration or loosening at final follow up of 24 months (Figure 5).

Discussion
Rates of GSW with spine injury have been quoted to be between 13–17% (1,3,4). These injuries present acutely with neurological dysfunction and have a high risk of infective complications (1-3,5-7). Patients with GSW to the spine with perforated bowel injuries have a higher rate of abdominal and surgical wound infections and risk is most in association with large bowel injuries (5-7,11). Infections like meningitis have been frequently reported in the presence of dural breeches and CSF leaks (1,5,7).
Most of the infections occur acutely following the GSW and rarely have a delayed presentation. Romanick reported on 20 cases of GSW with spinal injuries and noted 7 of 8 cases with colon injury developed paraspinal infections, osteomyelitis or meningitis (7). They advised non-surgical treatment in the case of low velocity injuries where colonic perforations were excluded. Roffi evaluated 42 of 308 cases of GSW with spine injuries that showed an intestinal perforation (5). The authors noted abdominal infections in cases with colon injuries but suggested that prolonged antibiotic therapy can prevent infections and extraction of the projectile does not have a bearing on the risk of infection (5). Though our patient received antibiotics for 14 days during the initial treatment following GSW; we noted a delayed spondylodiscitis in this case 4 months following the GSW.
Quigley analysed 114 GSW injuries with 27 cases suffering concomitant bowel injury. They noted 23 wound infections and 4 spine infections in their series. The 4 spine infections were associated with intestinal injuries and occurred within one week of the injury with no delayed presentations (11). However, none of the above series of GSW with bowel injuries report occurrence of delayed spondylodiscitis in their follow up. The reported case had a colonic perforation with the bullet proceeding to fracture L5 and was lodged in the spinal canal at the S1 level. Enterococcus from the colonic perforation caused a spondylodiscitis at the L5–S1 level with a delayed presentation 4 months following the GSW.
There is considerable variation in antibiotic protocols in the management of GSW (1,2,11). Prolonged antibiotics have been advised in the management of GSW especially in the scenario of coexisting bowel injury. Pasupuleti however noted that 92% of the cases in their series received antibiotics for 48 hours or less and did not show any increased incidence of infections (12). There is lack of high quality evidence to guide antibiotic protocol in the management of GSW. Quigley analysed the debridement and antibiotic protocols in GSW and concluded that further randomized control trials may be needed to establish evidence based guidelines (11).
Smugar evaluated 19 cases with retained projectile with MRI and noted no discomfort or change in the position of the projectile following MRI (13). However, they advised MRI may be performed in cases with retained projectile with complete neurological injury. Our case had no neurological deficit hence in view of the risk of migration of projectile we did not perform a MRI which could have useful in the preoperative evaluation.
Delayed presentations in cases with retained projectiles have been reported previously (8-10). These include lead intoxication and new onset neurological dysfunction following late migration of projectile. Scuderi evaluated 12 cases with retained projectile at an average follow up of 7.8 years and documented lead intoxication in one case (9). They advised careful observation and periodic evaluation of levels in such clinical scenarios. Late presentation with claudication and radiculopathy are ascribed to projectile migration and development of reactive fibrosis around the foreign body (10). Velmahos and Demetriades anlaysed the risk of retained projectile as a causative factor for infection in 81 retained bullet injuries and concluded that retained bullets do not increase the likelihood of infection (14). This case report however, suggested that delayed infection in cases with retained projectile may occur; with a resulting need to extract the projectile.
Conclusions
Late onset infections should be included in the differential diagnosis of patients presenting with delayed pain and neurological symptoms in cases with retained projectiles following GSW. Removal of the projectile, thorough debridement of infective focus and fusion may be needed in such scenarios.
Acknowledgements
The project was funded by Ganga Orthopaedic Research & Education Foundation, Coimbatore.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Bono CM, Heary RF. Gunshot wounds to the spine. Spine J 2004;4:230-40. [Crossref] [PubMed]
- Jakoi A, Iorio J, Howell R, et al. Gunshot injuries of the spine. Spine J 2015;15:2077-85. [Crossref] [PubMed]
- Sidhu GS, Ghag A, Prokuski V, et al. Civilian gunshot injuries of the spinal cord: a systematic review of the current literature. Clin Orthop Relat Res 2013;471:3945-55. [Crossref] [PubMed]
- Jaiswal M, Mittal RS. Concept of gunshot wound spine. Asian Spine J 2013;7:359-64. [Crossref] [PubMed]
- Roffi RP, Waters RL, Adkins RH. Gunshot wounds to the spine associated with a perforated viscus. Spine (Phila Pa 1976) 1989;14:808-11. [Crossref] [PubMed]
- Rabinowitz RP, Tabatabai A, Stein DM, et al. Infectious complications in GSW's through the gastrointestinal tract into the spine. Injury 2012;43:1058-60. [Crossref] [PubMed]
- Romanick PC, Smith TK, Kopaniky DR, et al. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg Am 1985;67:1195-201. [Crossref] [PubMed]
- Cristante AF, de Souza FI, Barros Filho TE, et al. Lead poisoning by intradiscal firearm bullet: a case report. Spine (Phila Pa 1976) 2010;35:E140-3. [Crossref] [PubMed]
- Scuderi GJ, Vaccaro AR, Fitzhenry LN, et al. Long-term clinical manifestations of retained bullet fragments within the intervertebral disk space. J Spinal Disord Tech 2004;17:108-11. [Crossref] [PubMed]
- Ajmal S, Enam SA, Shamim MS. Neurogenic claudication and radiculopathy as delayed presentations of retained spinal bullet. Spine J 2009;9:e5-8. [Crossref] [PubMed]
- Quigley KJ, Place HM. The role of debridement and antibiotics in gunshot wounds to the spine. J Trauma 2006;60:814-9; discussion 819-20. [Crossref] [PubMed]
- Pasupuleti LV, Sifri ZC, Mohr AM. Is extended antibiotic prophylaxis necessary after penetrating trauma to the thoracolumbar spine with concomitant intraperitoneal injuries? Surg Infect (Larchmt) 2014;15:8-13. [Crossref] [PubMed]
- Smugar SS, Schweitzer ME, Hume E. MRI in patients with intraspinal bullets. J Magn Reson Imaging 1999;9:151-3. [Crossref] [PubMed]
- Velmahos G, Demetriades D. Gunshot wounds of the spine: should retained bullets be removed to prevent infection? Ann R Coll Surg Engl 1994;76:85-7. [PubMed]


