Distal junctional failure secondary to L5 vertebral fracture—a report of two rare cases
Introduction
Junctional failure after instrumented fusion of the spine has become one of the greatest challenges in spine surgery (1,2). It can occur in patient of all ages following various forms of spinal instrumentation or fusion. This complication often results in debilitating symptoms such as pain or neurological deficit, or functional disability caused by progressive sagittal decompensation (3,4). While there are many hypotheses on the contributing risk factors and etiology of junctional failure, these causes can be broadly classified into three categories—instrument failure (5-8), problems at the instrument-bone interface (4,9), and accelerated adjacent disc level degeneration (3,4,10). Another school of thought is that a substantial number patients thought to have junctional failure in reality have preexisting degenerative changes that would have led to their presentation even without previous instrumentation (4).
Compared to proximal junctional failure (PJF), distal junctional failure (DJF) is rare, and as it is relatively unexplored in the literature, its pathophysiology remains unknown. Preferential failure at the distal end of the instrumented construct may be a result of distinct biomechanics in this region (4). In order to better understand and increase awareness of this phenomenon, further studies on such cases is necessary. In this report, we present two patients with DJF resulting from L5 vertebral fracture 6 months after instrumentation of the lumbar spine. Both cases were followed-up for 5 years. Consent for publication has been obtained from both patients.
Case presentation
Case 1
A 78-year-old woman presented with a 2-year history of low back pain and radicular pain involving the lateral aspect of the right leg and the dorsum of the right foot. This was associated with numbness over the dorsum of the right foot. The patient had symptoms of neurogenic claudication and could only walk up to 20 meters. Her past medical history included systemic lupus erythematosus (SLE) which was well-controlled with long-term corticosteroids. Other comorbidities included steroid-induced osteopenia with a pre-operative BMD T-score of −2.3, hypertension and dyslipidemia. Physical examination was unremarkable, with no focal neurological deficits in the lower limbs.
Plain radiographs of the lumbar spine showed degenerative scoliosis with a right T12 to L4 curve of 44°. Magnetic resonance imaging (MRI) of the lumbar spine showed multilevel degenerative disc disease with foraminal stenosis on the left at L2/3 and on the right at L4/5. The patient was treated with physiotherapy, but her symptoms did not improve. A subsequent decompression and instrumented posterolateral fusion (PLF) from T12 to L5 was performed, together with a right L4/5 transforaminal lumbar interbody fusion (TLIF) and a left L2/3 TLIF to improve the L2/3 and L4/5 foraminal heights. Post-operative X-rays are shown in Figure 1A. The patient experienced improvement of both her low back pain and right lower limb symptoms after her surgery, enabling her to return to her daily activities. Her Oswestry Disability Index (ODI) improved from a pre-operative score of 50.3 to 26.6 post-operatively.
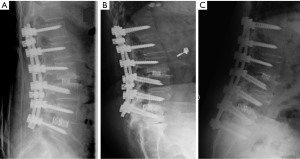
Six months after the operation, she developed acute low back pain without any precipitating trauma. There were no associated radicular symptoms. X-rays of the lumbar spine showed fracture of the L5 vertebral body (Figure 1B) and this was corroborated with a computed tomogram (CT) scan. Screw loosening at the fracture site was evident on imaging and the patient experienced pain upon truncal movement. She underwent surgical revision of both L5 pedicle screws and a left TLIF was performed at L5/S1 (Figure 1C). Thereafter, her symptoms improved and she remained asymptomatic at 5 years follow-up with an ODI score of 35.1.
Case 2
A 71-year-old woman presented with a 6-month history of low back pain, numbness in both lower limbs and a neurogenic claudication distance of 20 meters. Her medical history included diabetes mellitus, hypertension and primary osteopenia with a preoperative BMD T-score of −1.6. Physical examination was normal and there was no focal neurological deficit in the lower limbs. Plain radiographs of the lumbar spine showed grade I degenerative spondylolisthesis at L4/L5. This was associated with MRI findings of L3/4 and L4/5 disc bulges causing central canal stenosis.
In view of her persistent symptoms despite physical therapy, the patient underwent bilateral decompressions and TLIFs at L3/4 and L4/5, resulting in improvement of her symptoms (Figure 2A). Her ODI improved from a pre-operative score of 55.6 to 22.1 post-operatively.
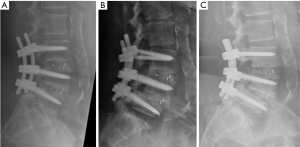
However, 6 months after her surgery, her low back pain recurred. The pain radiated to her buttocks and posterior thighs bilaterally, causing difficulties while walking. Lumbar X-rays and a CT scan demonstrated interval fracture of the L5 vertebral body with loosening of L5 screws (Figure 2B). Although revision surgery was offered, the patient declined. She was commenced on Teriparatide for her osteoporosis.
Five years after the DJF event, the patient’s fracture has healed (Figure 2C), although she continues to experience intermittent low back pain and bilateral posterior thigh pain. She remains homebound and ambulates with a walking frame. Her 5-year ODI score was 44.0.
Discussion
Unlike PJF which is common and hence discussed extensively in the literature (1,2), DJF is a relatively rare complication, usually occurring after long instrumentation (11). In a study of 13 patients with DJF by Kwon et al. (9), the most common mode of DJF was screw loosening and migration associated with intervertebral cage subsidence. Fractures of the vertebral body are rarely seen, and the English literature currently only contains descriptions of fractures involving the inferior endplate or pedicles (4,9). Our two cases are therefore unique as they both involve fractures of the L5 lowest instrumented vertebra (LIV) at 6 months following index surgery.
There are many potential contributing factors for DJF. However, bone fragility and bony stress risers at the LIV are likely the two predominant factors in these two cases since the mechanism of failure is vertebral fracture. Both patients have inherently weak bone suggested by their ages, medical comorbidities, chronic medications and an objective BMD T-score of −2.3 and −1.6 respectively. While this complication may not be totally unavoidable, surgery should ideally be deferred to allow medical optimization of bone quality (12). Unfortunately, both patients had severe symptoms and surgery was allowed to proceed following detailed discussions and counseling with the patients on the increased risk of junctional failure and revision surgery.
Apart from osteoporosis, we hypothesize that the location of LIV at L5 may also play a substantial role. Bridwell et al. (13) noted that the L5 pedicles are shorter, wider, contain more cancellous bone than other lumbar vertebra, and are more medially angulated. This may result in the placement of long, oversized pedicle screws, inadvertently weakening both pedicles and bony cortex, increasing the risk of fracture. As such, it is suggested that the L5 vertebra may not be the ideal choice for the LIV. For this reason and a multitude of other reasons including the need to gain distal fixation strength and preventing L5/S1 accelerated degeneration, many authors have suggested extending the fixation to the ilium which increases the distal construct rigidity, pullout strength and mechanical lever arm (4,9,13,14). However, no strong evidence in the literature supports this even though it is widely practiced. Extending fusion into the sacrum or pelvis despite lack of clinical indication is not generally favored as it abolishes movement at the L5-S1 segment which contributes 15% of the total lumbar angular range of motion (15,16). Other potential complications include increased length and morbidity of surgery, with the potential need for other fixation points, either at the distal sacrum or ilium (17), potential pseudoarthrosis of L5 and S1 and subsequent degeneration of the sacroiliac joint (18).
In a recent retrospective review of 74 patients with previous long spinal fusion requiring revision by O’Neill et al., extension of fusion into the sacrum resulted in improvements in the ODI, Scoliosis Research Society scores (SRS) and spinal alignment (P<0.05) up to 5 years of follow-up (19). These outcomes are comparable with outcomes of patients undergoing revision surgery for failed lumbar spinal fusion in general (i.e., LIV not specified) (20). However, there are studies showing high major complications rates (30%) and revision rates (20%) with extension of fusion into the sacrum (19). This makes routine instrumentation into the pelvis a weighty consideration. In fact, revision surgery for adult spinal deformity has also been shown to increase the average cost of surgery by more than 70% (21), suggesting the need to consider each patient thoroughly on a case-by-case basis.
Lastly, it has recently been found that the lumbar spine changes its alignment in various different postures (22,23) with both the L4/5 and L5/S1 levels of the spine moving into flexion together with pelvic retroversion. By rendering the spine immobile during fusion and creating a lordosis ending at L5, high mechanical stress can happen in the LIV of L5 or the remaining L5/S1 joint during pelvic retroversion when sitting. This may also lead to DJF either through a fracture in L5 or accelerated degeneration in L5/S1. To better understand these phenomena, future studies should investigate the biomechanics of the distal lumbar spine in attempts to understand DJF and formulate reliable selection criteria for LIV. These two cases highlight DJF as an entity that deserves more attention in future studies. They also emphasize the importance of optimizing bone quality prior to spinal instrumentation and fusion, particularly in situations where fusion ends above the pelvis. Finally, selection of the LIV should always be individualized, and the risk of DJF must be discussed with the patients preoperatively.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consents were obtained from the patients for publication of this manuscript and any accompanying images.
References
- Hostin R, McCarthy I, O’Brien M, et al. Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976) 2013;38:1008-15. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 2008;33:2179-84. [Crossref] [PubMed]
- Denis F, Sun EC, Winter RB. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 2009;34:E729-34. [Crossref] [PubMed]
- Arlet V, Aebi M. Junctional spinal disorders in operated adult spinal deformities: present understanding and future perspectives. Eur Spine J 2013;22 Suppl 2:S276-95. [Crossref] [PubMed]
- Farcy JP, Schwab FJ. Management of flatback and related kyphotic decompensation syndromes. Spine (Phila Pa 1976) 1997;22:2452-7. [Crossref] [PubMed]
- La Grone MO. Loss of lumbar lordosis. A complication of spinal fusion for scoliosis. Orthop Clin North Am 1988;19:383-93. [PubMed]
- Lagrone MO, Bradford DS, Moe JH, et al. Treatment of symptomatic flatback after spinal fusion. J Bone Joint Surg Am 1988;70:569-80. [Crossref] [PubMed]
- Moe JH, Denis F. The iatrogenic loss of lumbar lordosis. Orthop Trans 1977;1:131.
- Kwon BK, Elgafy H, Keynan O, et al. Progressive junctional kyphosis at the caudal end of lumbar instrumented fusion: etiology, predictors, and treatment. Spine (Phila Pa 1976) 2006;31:1943-51. [Crossref] [PubMed]
- Lafage V, Ames C, Schwab F, et al. Changes in thoracic kyphosis negatively impact sagittal alignment after lumbar pedicle subtraction osteotomy: a comprehensive radiographic analysis. Spine (Phila Pa 1976) 2012;37:E180-7. [Crossref] [PubMed]
- Kuhns CA, Bridwell KH, Lenke LG, et al. Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5-S1 disc, minimum 5-year follow-up. Spine (Phila Pa 1976) 2007;32:2771-6. [Crossref] [PubMed]
- Lubelski D, Choma TJ, Steinmetz MP, et al. Perioperative Medical Management of Spine Surgery Patients With Osteoporosis. Neurosurgery 2015;77:S92-S97. [Crossref]
- Bridwell KH, Edwards CC 2nd, Lenke LG. The pros and cons to saving the L5-S1 motion segment in a long scoliosis fusion construct. Spine (Phila Pa 1976) 2003;28:S234-42. [Crossref] [PubMed]
- Edwards CC 2nd, Bridwell KH, Patel A, et al. Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5-S1 disc. Spine (Phila Pa 1976) 2003;28:2122-31. [Crossref] [PubMed]
- Tan Y, Aghdasi BG, Montgomery SR, et al. Kinetic magnetic resonance imaging analysis of lumbar segmental mobility in patients without significant spondylosis. Eur Spine J 2012;21:2673-9. [Crossref] [PubMed]
- Hey HW, Lau ET, Tan KA, et al. Lumbar Spine Alignment in 6 Common Postures - a ROM Analysis With Implications for Deformity Correction. Spine (Phila Pa 1976) 2017. [Epub ahead of print]. [Crossref] [PubMed]
- McCord DH, Cunningham BW, Shono Y, et al. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976) 1992;17:S235-43. [Crossref] [PubMed]
- Cho KJ, Suk SI, Park SR, et al. Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative lumbar scoliosis. Eur Spine J 2009;18:531-7. [Crossref] [PubMed]
- O’Neill KR, Bridwell KH, Lenke LG, et al. Extension of spine fusion to the sacrum following long fusions for deformity correction. Spine (Phila Pa 1976) 2014;39:953-62. [Crossref] [PubMed]
- Djurasovic M, Glassman SD, Howard JM, et al. Health-related quality of life improvements in patients undergoing lumbar spinal fusion as a revision surgery. Spine (Phila Pa 1976) 2011;36:269-76. [Crossref] [PubMed]
- McCarthy IM, Hostin RA, Ames CP, et al. Total hospital costs of surgical treatment for adult spinal deformity: an extended follow-up study. Spine J 2014;14:2326-33. [Crossref] [PubMed]
- Hey HW, Teo AQ, Tan KA, et al. How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Hey HW, Wong CG, Lau ET, et al. Differences in erect sitting and natural sitting spinal alignment-insights into a new paradigm and implications in deformity correction. Spine J 2017;17:183-9. [Crossref] [PubMed]


