Megacolon as an atypical presentation of cervical myelopathy
Introduction
Cervical myelopathy is a syndrome of spinal cord dysfunction caused by compression of the cervical spinal cord. Patients with cervical myelopathy commonly present with a variable pattern of neurological deficits, ranging from hand clumsiness, gait disturbances, sensory deficits, upper motor neurons signs, urinary retention or fecal incontinence. In this report, we present a case of megacolon secondary to cervical myelopathy, which is not described in literature.
Case presentation
Mr. T, an independent 61-year-old gentleman was admitted to our hospital with symptoms of cervical myelopathy. His symptoms had started several months prior, but rapidly deteriorated over the past few weeks to the extent that he was unable to ambulate independently.
His past medical history includes type 2 diabetes mellitus, hyperlipidemia and alcohol dependence. Of note, he also had an episode of sigmoid volvulus four months prior, which was reduced endoscopically. Colonoscopy and CT of his abdomen noted the presence of a chronic megacolon, without any underlying obstructive cause.
At presentation, Mr. T’s main complaint was difficulty performing fine motor tasks such as eating and buttoning his clothes. He also complained of numbness in both hands. He also had a very unsteady gait, requiring a walking stick to ambulate and sustaining multiple falls over the past few months. He did not complain of urinary or fecal incontinence. He had a Japanese Orthopaedic Association (JOA) score of 10. Clinical examination revealed upper motor neuron signs consistent with cervical myelopathy. He was hyper-reflexic in both the upper and lower limbs with a positive Hoffman’s test. He was unable to perform the tandem gait. Formal motor and sensory testing of his upper and lower limbs was normal. Rectal examination showed preservation of anal sphincter tone with no saddle anesthesia. An MRI scan of the cervical spine showed cervical cord compression at the level of C3–5 with cord signal changes (Figure 1). He was diagnosed with cervical myelopathy and was offered a posterior decompression and fusion.

However, his operation had to be delayed due to concerns about his worsening abdominal distension. On examination, his abdomen was soft and non-tender with no rigidity or guarding. An abdominal X-ray on admission showed a severely dilated large bowel, measuring up to 12 cm (Figure 2). A computed tomography scan performed excluded the presence of any intestinal obstruction or volvulus.
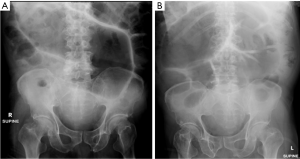
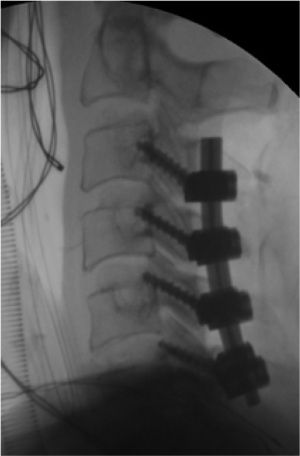
Upon consultation with the general surgery service, a flatus tube was inserted pre-operatively, with the intention to decompress his colon and abdominal distention prior to surgery. However, his abdominal distention persisted for 2 weeks without signs of any improvement. A decision was then made to proceed with surgery, despite the theoretical risk of bacterial translocation, in view of his severe and progressive myelopathy symptoms. Mr. T underwent successful C3–6 posterior decompression and fusion— laminectomy with lateral mass fixation, decortication of lateral masses and facets, followed by fusion with autograft (Figure 3). Post-operatively, Mr. T’s made good recovery and he was able to walk with minimal assist. Interestingly, his abdominal distension also improved significantly. A repeat abdominal X-ray on the second day post-surgery showed complete resolution of the megacolon (Figure 4). The flatus tube was subsequently removed with no worsening of abdominal distension. He was later transferred to a rehabilitation facility where he stayed a further 2 months before he went home. At his last review at 6 months, he required minimal assistance with ambulation and his fine motor skills had improved. His abdominal distention had not recurred.
Discussion
Megacolon is defined as a dilation of the colon in the absence of mechanical obstruction such as volvulus or obstructing mitotic lesions. While the definition of megacolon differs in literature, a cecal diameter of 12cm is usually used as a cut-off (1).
Megacolon has been described as a complication of spinal cord injury. Harari et al. found megacolon to be highly prevalent in their cohort, with 73% of patients having colonic diameter >6 cm. They found that factors predictive of megacolon include age over 50 years, SCI more than 10 years previously, a history of urinary outlet surgery, at least once weekly use of laxatives, use of anticholinergic drugs, and use of calcium-containing antacids.
Harari et al. (2) postulated that cervicothoracic spinal cord injury would cause interruption of cortical inhibitory pathways, leading to increased sympathetic stimulation. This causes increased smooth muscle tone and anorectal dyssynergia, leading to chronic fecal impaction and subsequent colonic dilation. This was further supported by a study by Faaborg et al. (3), who showed that colonic transit time is increased after spinal cord injury.
Megacolon has not previously been identified as a manifestation of cervical myelopathy. We postulate that long standing cervical cord compression may be responsible for the development of Mr. T’s “atonic” megacolon, as evidenced by the significant reduction of colonic diameter immediately post-surgery. Some authors suggest that plain abdominal radiography is a good screening method for megacolon in spinal cord injury patients and can also be considered for patients with cervical myelopathy (4).
This case report highlights that cervical cord compression may be a cause of chronic megacolon. Patients may experience relief of megacolon after undergoing cervical cord decompression. However, Megacolon should be treated as a diagnosis of exclusion. Adequate investigation to rule out other causes of intestinal obstruction should be performed, including abdominal imaging and endoscopy. Once all obstructive causes are excluded, surgical decompression of the cervical stenosis should proceed, and need not be delayed for the megacolon to resolve spontaneously.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Melling J, Makin CA. Sigmoid volvulus, acquired megacolon and pseudo-obstruction. Surgery (Oxford) 2011;29:387-90. [Crossref]
- Harari D, Minaker KL. Megacolon in patients with chronic spinal cord injury. Spinal Cord 2000;38:331-9. [Crossref] [PubMed]
- Faaborg PM, Christensen P, Rosenkilde M, et al. Do gastrointestinal transit times and colonic dimensions change with time since spinal cord injury? Spinal Cord 2011;49:549-53. [Crossref] [PubMed]
- Park HJ, Noh SE, Kim GD, et al. Plain abdominal radiograph as an evaluation method of bowel dysfunction in patients with spinal cord injury. Ann Rehabil Med 2013;37:547-55. [Crossref] [PubMed]