Is cell salvage cost-effective in posterior arthrodesis for adolescent idiopathic scoliosis in the public health system?
Introduction
Blood loss is a major cause of morbidity in spinal deformity surgeries. Often arthrodesis of the spine is associated with massive bleeding (1).
In general, patients with adolescent idiopathic scoliosis (AIS) submitted to posterior spinal fusion with segment instrumentation lose a high percentage of their total blood volume (650 to 2,839 mL) (2,3). As a result, they need allogeneic blood transfusions. Despite the current diagnostic methods in blood banks, transfusion is not totally safe because of the risks and side effects, such as the transmission of viral diseases and various immunological reactions (3,4).
Several blood management techniques are used in order to reduce the need for this type of blood transfusion in posterior spinal fusion surgery: pre-donation of autologous blood, normovolemic hemodilution, hypotensive anesthesia, aminocaproic acid, tranexamic acid, preoperative Erythropoietin, and blood cell salvage (CS) systems with intraoperative reinfusion (2).
The CS is a system that collects blood from the operative field by aspiration and then washes and filters the residue, such as cellular and biochemical debris. After the filtration process the patient’s own erythrocytes can be returned to them (2).
This method may eventually eliminate the need for both preoperative collection of blood from the patient for autologous transfusion in surgery and allogeneic transfusion. Other advantages are: the lack of transmission of viral diseases, a reduced risk of alloimmunization, normal potassium concentration, considering the fact that the cells are infused at room temperature and the capacity of red blood cells (RBC) to carry oxygen at 2,3-diphosphoglycerate (2,3 DPG) levels (4). Furthermore, it is a good alternative for patients who refuse to receive donor blood due to their religious beliefs (1).
Despite the advantages of this method its effectiveness in reducing allogeneic transfusions in scoliosis surgery is not clear, neither is its cost-effectiveness in terms of public health, since some studies show a positive association and others do not.
This study aims to evaluate the effectiveness and cost-effectiveness of intraoperative blood CS as a method to reduce allogeneic transfusions in patients with idiopathic scoliosis undergoing posterior spinal arthrodesis.
Methods
This is a case-control study with a sample of 42 patients who underwent surgical treatment for AIS by posterior arthrodesis using only third generation materials (pedicle hooks and screws) as surgical instruments, in the Orthopedics Service at the General Hospital of Fortaleza (HGF), Brazil, from August 2008 to December 2014. All the surgeries were performed by the same two spine surgeons, operating in the same location under similar conditions and using similar surgical techniques.
More than one model of intra-operative blood CS system was used in the period, in view of bidding procedures for their acquisition in the public service (2009–2010: Dideco Compact Advanced; 2011–2012: Dideco Electa Essential Concept; 2013: Fresenius CATS; and 2014: Autolog Medtronic). The device was used in 27 patients (CS group) and was not used with 15 patients (control group). The patients were not randomized but each surgeon decided independently on the use of CS.
From a total of 72 people undergoing corrective surgery for scoliosis in the institution, those who met the following inclusion criteria participated in the study: individuals of both genders, diagnosed with adolescent idiopathic scoliosis and operated on by the same team of spinal surgeons at the HGF Orthopedic Service from August 2008 to December 2014 and who underwent arthrodesis by posterior approach in which, as mentioned above, third generation materials (pedicle hooks and screws) were used as surgical instruments. The following were excluded from the sample: those who presented a history of previous spinal surgery as well as revision surgery; those with a history of hemostasis disorders, a low platelet count (<100,000), changes in prothrombin time activity (TP)/international normalized ratio (INR), activated partial thromboplastin time; previous thromboembolic events prior to surgery or a family history of thromboembolism, and those whose religious beliefs (Jehovah’s Witnesses) do not allow transfusion of allogeneic blood.
Pre-donated autologous blood, intraoperative isovolumetric hemodilution or erythropoietin were not used on any patient during the pre and postoperative periods. Of the antifibrinolytic drugs, tranexamic acid and aminocaproic acid were only used in twelve patients (7 who used CS and 5 who did not). All the patients were placed prone on the operating table, leaving the abdomen free to decrease the abdominal venous pressure. Hypotensive anesthesia was used during all the surgeries to maintain a mean arterial pressure around 60 mmHg. During the spinal reduction process around 80 mmHg was used to prevent ischemic injury to the spinal cord. The parameters for blood transfusion included the signs and symptoms of anemia: a reduced urinary volume <30 mL/h measured by urinary catheter, tachycardia (>100 beats/min) and hypotension (<100 mmHg systolic blood pressure) refractory to volumetric expansion and a hemoglobin level below 8 mg/dL for blood gas or a hemoglobin level below 7 mg/dL independently of signs or symptoms of anemia. The need for allogeneic transfusion during surgery was a joint decision between the surgeon and the anesthesiologist.
Intra-operative neurophysiological monitoring through the somatosensory evoked potentials was not used on any of the patients; only the wake-up test was employed.
All the surgical wounds were closed with two suction drains, one deep and the other subcutaneous; both were removed when drainage over 24 h was less than 100 mL. On average this was around the third postoperative day.
In the postoperative period the patients remained in the intensive care unit for around 48 h after surgery. At that time, the same parameters for blood transfusion were adopted and the decision to transfuse was made jointly by the surgeon and the intensive care doctor. After this phase, the patient was discharged to the ward leaving the decision to transfuse to the surgeon in charge.
The groups were compared according to the following data from medical records: sex; age at surgery; preoperative weight; duration of the surgical procedure in minutes; intraoperative use of CS; volume of postoperative blood drainage; blood volume reinfused by CS; pre and postoperative hemoglobin (Hb) and hematocrit (Hct) levels; the amount of intra and postoperative concentrated allogeneic RBCs transfused, and the cost of the procedures.
We processed the data using SPSS 20.0 License No. 10101131007 to calculate the average, median and standard deviation measures. The comparison of the means according to the general characteristics of the CS and non-CS groups, the erythrocyte levels (Hb and Hct) and the need for blood transfusions (intra and postoperative) were carried out using the Student t, Mann-Whitney and Friedman tests, with multiple comparisons performed by the Conover test. In the associations between the variable CS and non-CS and the independents, the χ2 tests and likelihood ratio were applied, their force was calculated by their 95% CI. The confidence level was set at 0.05.
In accordance with Resolution 466/2012 of the Brazilian National Health Council the present study was approved by the Research Ethics Committee of the institution through norm 1.444.279. All the participants in the study signed a consent form.
Results
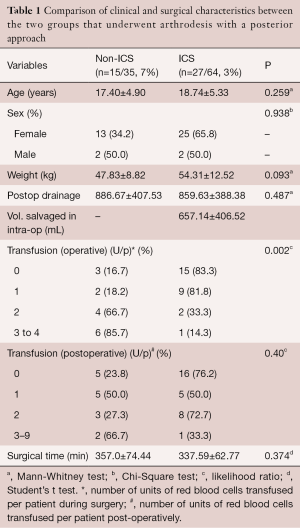
As shown below, the average age of the patients was 17.40±4.90 years in the control group and 18.74±5.33 years in the CS group (P>0.05). For the other variables there were no significant differences between the groups: gender, preoperative weight, postoperative blood drainage, and surgical time. In the CS group the average blood volume recovered intra-operatively and reinfused in the patient was 657.14±406.52 mL (Table 1).
Full table
In the patients who used the intraoperative CS system there was less allogeneic blood transfusion during the intra-operative period compared to the control group (P=0.002) (Table 1).
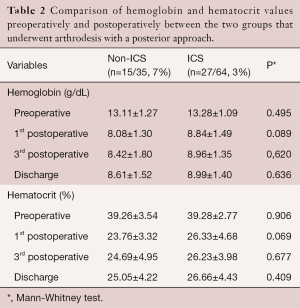
When evaluating the erythrocyte levels of the patients in the two groups, we noted that the final hemoglobin and hematocrit values (on the 1st and 3rd postoperative days and at discharge) were higher in the group that used the ICS intraoperatively (P>0.05) (Table 2).
Full table
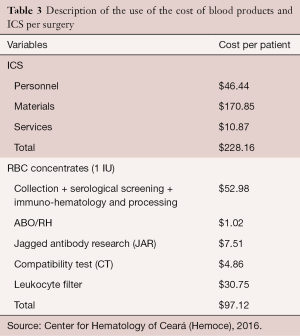
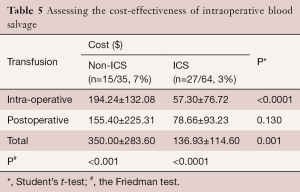
The cost of using the intraoperative CS system per surgery is shown in Table 3, as well as the cost to the State of a concentrate of allogeneic RBCs per patient of on average 280 mL.
Full table
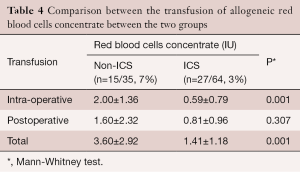
When comparing the transfusion of allogeneic RBC concentrates between the two groups we noted that those who used the CS had fewer units transfused during surgery than the control group (P=0.01). In the postoperative period this difference was not significant (P>0.05). When considering the sum of the (intra and postoperative) periods there was a significant reduction in the total allogeneic concentrates transfused in patients using the device when compared to the control group (P=0.01) (Table 4).
Full table
As shown in Table 5, there was a lower cost with the transfusion of allogeneic RBC concentrates in the group using the CS than in the control group (P<0.0001) during the intra-operative period. Although the cost was higher in the control group of patients in the postoperative period this difference was not significant (P>0.05). When considering the total cost of allogeneic transfusions by adding the two periods together, the cost was lower in patients who used the intra-operative blood salvage device (P=0.001). When analyzing the average costs of the group that used the CS, there was no difference between the values of the intra and postoperative periods, but there was a difference between them and the total (P=0.001).
Full table
Discussion
In a meta-analysis published in 2010 (3), the results were analyzed to evaluate the effect of intra-operative blood salvage during spinal surgery based on three retrospective studies (one on lumbar arthrodesis in degenerative disease, the second on lumbar arthrodesis in adults and the third on scoliosis employing Harrington rods); according to the authors all three share a low quality methodology. This systematic review found little evidence in the literature in favor or against the use of this system in elective spinal surgery.
Some authors (5) evaluated the benefit of intra-operative blood salvage in surgery for scoliosis comparing two groups, one of 58 patients in which the device was used and another 37 patients in which it was not used. Based on the findings, the blood volume recovered by the equipment must be at least 500 mL to justify its use in surgery. The surgeon can use this number to make a better estimate of whether to use the device or not. If a blood loss of less than 500 mL is expected, this study shows that the cost of using the device is not justified. Moreover, as concluded, the case group of patients had the same chance of receiving allogeneic transfusions compared to the control group.
In our study, blood volume recovered by CS and reintroduced to the patient was on average 657 mL. According to scholars (5), this in itself would justify the adoption of the device.
In a retrospective study, researchers (6) evaluated the efficacy of intra-operative blood CS in patients with idiopathic scoliosis undergoing surgical treatment. There were two groups; one with sixteen patients which used the system and another with seventeen patients which did not. The authors found that there was no difference between the groups in the evaluation of allogeneic transfusion. They suggest that the use of hypotensive anesthesia in all the patients coupled with a shorter operative time when compared to other series of cases may have been responsible for reducing the effectiveness of the CS in this case.
However, another study (7) measuring the effectiveness of CS in 54 pediatric patients with idiopathic scoliosis submitted to posterior arthrodesis with segment instrumentation, showed that the use of CS was significantly associated with the reduction of intra-operative and perioperative allogeneic blood transfusion. To this end, the group that used the device (21 patients) was compared with the group that did not (33 patients).
According to these authors, the divergent findings of different studies regarding the efficacy of the intra-operative blood CS system can be explained by the manner in which the equipment was handled, as well as the perioperative blood management strategies. These authors report a uniform perioperative strategy in blood management: no patient in their study was submitted to a pre-donation of autologous blood, isovolumetric hemodilution or received antifibrinogenic intraoperative medications. They only used hypotensive anesthesia.
Another survey (2) adopted a perioperative blood management approach that was similar to the cited authors, who evaluated 45 patients undergoing posterior spinal fusion with segmented instrumentation for AIS with or without the use of CS. They showed that a reduced amount of allogeneic blood transfusion was required in the perioperative period in the group of patients who used the CS (23 patients) than in the control group (22 patients).
With a system similar to the two afore mentioned studies, some researchers (8) retrospectively evaluated children and school-age adolescents with scoliosis undergoing posterior spinal fusion with segmented instrumentation. They evaluated two groups, one using CS (67 patients) and a control group (180 patients). They found that the use of a red blood CS system significantly reduced the need for intraoperative allogeneic transfusion but failed to reduce total perioperative allogeneic blood transfusion.
Our study observed a significant reduction of allogeneic blood transfusions during surgery in patients who used CS when undergoing arthrodesis by posterior approach with segment instrumentation compared to the control group. No significant difference was found in the transfusion of concentrated RBCs between the two groups in the postoperative period. When considering the sum of the (intra and postoperative) periods there was a significant reduction in the amount of transfused allogeneic concentrates in patients using the device compared to the control group (P=0.01).
Despite the presence of higher erythrocyte levels (hemoglobin and hematocrit) on the 1st and 3rd postoperative days and at discharge in CS patients when compared with the control group, this difference was not significant.
The authors of the article under review corroborate the interpretation (7) that the divergent conclusions in different studies regarding the effectiveness of the intra-operative blood CS system can be explained by the specific ways CS is used, as well as the strategies for perioperative blood management. In our study, there was no pre-donation of autologous blood or isovolumetric dilution. We only used hypotensive anesthesia and in some cases an antifibrinolytic aminocaproic acid agent, in a loading dose of 100 mg/kg (maximum dose of 6 g) during anesthetic induction (in 7 patients who used the CS and in 5 patients who did not).
In one study (9), the aim was to assess the cost-effectiveness of the CS in posterior lumbar arthrodesis surgery with segment instrumentation in adults. In the group that used the intraoperative autotransfusion system the cost was $512.00 per patient. In the control group, the cost of a pre-donated blood autotransfusion was around $270.00 per patient, while the cost per unit of transfused allogeneic blood was around $250.00. The findings show that the expense of the blood replacement proved to be significantly higher for the case group than for the control group as such a device has a fixed cost regardless of the amount of blood collected and reinfused.
In their study (8), the authors evaluated the cost-effectiveness of intraoperative blood CS in school-age patients with scoliosis undergoing posterior spinal fusion with segment instrumentation in a reference center in China. As noted, the cost for each allogeneic blood transfusion unit was $70.49. This includes ABO and RH types, research of irregular antibodies, cross matching, concentrated RBCs, filtration of white blood cells and administrative expenses. The cost of the intra-operative autotransfusion system is a flat rate of $311.00. It covers the costs of the piping, equipment, bag, the liner and the anticoagulant solution.
The authors above found (8) that the costs of allogeneic blood transfusion in China are relatively low compared to the costs in the USA ($70.49 vs. $250.00). Moreover, the concentrate of RBCs is equivalent to 200 mL of blood in China and 500 mL in the United States. Therefore, assuming that the use of CS is the same in the USA and China ($311.00), the total cost of transfusion for each patient was calculated under the premise of the American standard. According to this standard, there was no significant difference between the total costs of blood products in the CS and control group (8).
In a randomized prospective study (4) at a Chinese hospital the cost of CS for arthrodesis spinal surgery was around $350.00 per case; while 1-day hospital stay in that country costs about $100.00. Patients undergoing pre-donation of blood for autotransfusion will remain in hospital for at least seven days before this surgical procedure. As a result, using the CS led to a significant cost reduction: there was a net saving of at least $350.00 per patient. Multiplying this by the number of cases treated in a year represents even greater savings.
In our study, the blood volume salvaged by CS and reintroduced to the patient was an average of 657 mL, which according to some authors (5) is in itself sufficient justification for using the device. Considering that the average volume of concentrated RBCs provided by the State Blood Bank (Hemoce) is approximately 280 mL, the volume recovered by the device is equivalent to 2.35 units of concentrated erythrocytes. Furthermore, the fixed cost of the device per surgery is around $ 228.00 and a bag of concentrated RBCs costs $97.00. If the device retrieves 2.35 units, this amount multiplied by the cost of the RBC gives a total of $228.00. This association shows that if only the volume recovered and reinfused by the device is taken in to account there is no onus to the State. At this point, our study differs from those reported by other authors (9).
As noted when evaluating the total cost of the intra-operative and postoperative RBC transfusion between the two groups, the total expenditure was higher in the control group when compared to the CS (P=0.01). Faced with this difference ($350.00 to $136.93) we obtained a value of $213.07, which corresponds to the net saving for each patient that used the device. Multiplying this value by the 27 patients who used the device there was a reduction of $5,752.89 in State spending on the transfusion of RBCs. Our results corroborate the study mentioned above (4).
It is noteworthy that in addition to eliminating the need for blood collection from the patient before surgery for autologous transfusion during surgery, as well as the need for allogenic transfusion, this device has other advantages, such as the absence of transmission of viral diseases, a reduced risk of alloimmunization, and normal potassium concentration due to the cells being infused at room temperature (4).
The limitations regarding a retrospective study are clear, such as the lack of randomization of patients and the presence of confounding variables. In our view, further studies are needed, particularly at the national level, to assess both the effectiveness of CS and its cost-effectiveness in public health.
Conclusions
This study found that intra-operative recovery was effective in reducing allogeneic blood transfusion during surgery and in the whole (intra and postoperative) period in patients undergoing posterior arthrodesis with segment instrumentation for the treatment of idiopathic scoliosis. Furthermore, the method proved to be cost-effective in terms of public health by reducing spending on allogeneic blood transfusions in this type of treatment. The reduction in the transmission of viral diseases and the reduced risk of alloimmunization provided by intraoperative blood salvage should also be taken into account.
Acknowledgements
The authors would like to thank Dr. Samuel Ximenes Feijão, who helped collect patient data and Dr. Luciana Maria de Barros Carlos for providing information on the costs of cell salvage and red blood cells concentrate.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: In accordance with Resolution 466/2012 of the Brazilian National Health Council the present study was approved by the Research Ethics Committee of the institution through norm 1.444.279. All the participants in the study signed a consent form.
References
- Joseph SA Jr, Berekashvili K, Mariller MM, et al. Blood conservation techniques in spinal deformity surgery: a retrospective review of patients refusing blood transfusion. Spine (Phila Pa 1976) 2008;33:2310-5. [Crossref] [PubMed]
- Ersen O, Ekıncı S, Bılgıc S, et al. Posterior spinal fusion in adolescent idiopathic scoliosis with or without intraoperative cell salvage system: a retrospective comparison. Musculoskelet Surg 2012;96:107-10. [Crossref] [PubMed]
- Elgafy H, Bransford RJ, McGuire RA, et al. Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine (Phila Pa 1976) 2010;35:S47-56. [Crossref] [PubMed]
- Liang J, Shen J, Chua S, et al. Does intraoperative cell salvage system effectively decrease the need for allogeneic transfusions in scoliotic patients undergoing posterior spinal fusion? A prospective randomized study. Eur Spine J 2015;24:270-5. [Crossref] [PubMed]
- Weiss JM, Skaggs D, Tanner J, et al. Cell Saver: is it beneficial in scoliosis surgery? J Child Orthop 2007;1:221-7. [Crossref] [PubMed]
- Akgül T, Dikici F, Ekinci M, et al. The efficacy of cell saver method in the surgical treatment of adolescent idiopathic scoliosis. Acta Orthop Traumatol Turc 2014;48:303-6. [Crossref] [PubMed]
- Bowen RE, Gardner S, Scaduto AA, et al. Efficacy of intraoperative cell salvage systems in pediatric idiopathic scoliosis patients undergoing posterior spinal fusion with segmental spinal instrumentation. Spine (Phila Pa 1976) 2010;35:246-51. [Crossref] [PubMed]
- Miao YL, Ma HS, Guo WZ, et al. The efficacy and cost-effectiveness of cell saver use in instrumented posterior correction and fusion surgery for scoliosis in school-aged children and adolescents. PLoS One 2014;9:e92997. [Crossref] [PubMed]
- Reitman CA, Watters WC 3rd, Sassard WR. The Cell Saver in adult lumbar fusion surgery: a cost-benefit outcomes study. Spine (Phila Pa 1976) 2004;29:1580-3; discussion 1584. [Crossref] [PubMed]
Contributions: (I) Conception and design: JA Oliveira, FA Filho, SR Lima Verde, PC Almeida, VF de Oliveira; (II) Administrative support: None; (III) Provision of study materials or patients: FV Fernandes, SR Verde; (IV) Collection and assembly of data: FV Fernandes, SR Verde; (V) Data analysis and interpretation: JA Oliveira, PC Almeida, FA Filho; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.


