A prospective clinical study comparing MI-TLIF with unilateral versus bilateral transpedicular fixation in low grade lumbar spondylolisthesis
IntroductionOther Section
Transforaminal lumbar interbody fusion (TLIF) was initially described by Harms and Rolinger in 1982 (1). It has become one of the standard techniques for the decompression of the ipsilateral foramen and a proper interbody fusion. This technique offers the anatomical advantage of not requiring a great retraction of the thecal sac and its contents. High fusion rates have been reported. Clinical outcomes comparable to those obtained with posterolateral fusion (PLF) and posterior lumbar interbody fusion (PLIF) have been described. This procedure is usually accompanied by the placement of bilateral transpedicular screws in the corresponding segment; this results in immediate rigid segment stabilization that will last while fusion takes places (2-4). Some authors have demonstrated that excessive stiffness of such a construct can jeopardize the fusion process due to graft resorption that is in hand due to lack of stress against end platesJeny (5-7). Scientific evidence in the literature has demonstrated that unilateral transpedicular screw fixation, after fusion, produces radiological results comparable with bilateral fixation: this is done at a lower cost because less amount of implants are used (8-12). Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) was initially described by Foley (13). It has similar radiographic fusion rates than open TLIF and a tendency to yield better clinical results in the immediate postoperative period (14). Some authors have demonstrated that unilateral transpedicular screw fixation is as effective as bilateral screw fixation after MI-TLIF (15,16).
We sought to evaluate the clinical efficacy of unilateral compared with bilateral transpedicular screw fixation after MI-TLIF technique in patients with low-grade symptomatic lumbar spondylolisthesis (Meyerding grade I, II). The main outcome measure was obtained with Oswestry Disability Index (ODI) at 12 months.
MethodsOther Section
Study characteristics and patient population
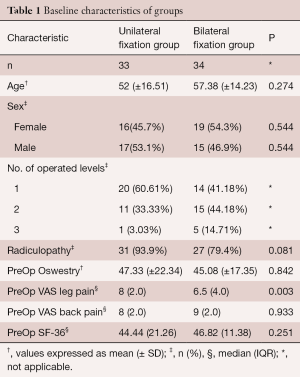
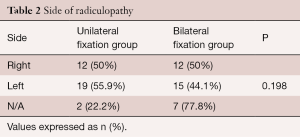
A prospective and comparative cohort study was performed in 67 patients with low-grade symptomatic lumbar spondylolisthesis (Meyerding grade I, II) with facetary joint pain. The study was carried-out from May 1, 2012 to May 1, 2015. An institutional approval for this study was obtained. All patients were diagnosed with lumbar spondylolisthesis utilizing dynamic X-ray imaging (flexion-extension) and clinical axial pain. All patients were operated by the same surgeon. We excluded patients with previous spine surgery, tumors, metastases, spine infection, and rejection to participate in the present study. Patients were allocated to unilateral fixation group (n=33) and bilateral fixation group (n=34). Allocation of patients in groups was performed by consecutive sampling. Patients were assigned to a group during the initial visit. One-hundred percent of follow-up was achieved. Baseline characteristics of both groups are presented in Table 1. Side of radiculopathy was similar in both groups prior to surgery, Table 2. Operated segments ranged from L2-L3 to L5-S1. Patients were subjected from 1 to 3 operated levels. The median age of the patients was 59 [29–81] years old. The sample by sex was 35 female patients (52.2%) and 32 male patients (47.8%). Radiculopathy was diagnosed in 58 patients (86.6%) and no diagnosed in 9 patients (13.4%).
Full table
Full table
Surgical technique
With the patient in prone position under general anesthesia, use of continuous neurophysiologic monitoring, and acquisition of intensified fluoroscopy images with C-arm, surgical approach was performed on the most symptomatic side. Progressive tubular retractors were used. Minimally invasive surgical procedure was performed through an 18 mm diameter working cannula. After a complete lateral facetectomy, discectomy, and end-plates, preparation was performed and bone graft was delivered in the lumbar intersomatic space. A rectangular bullet-nose cage was inserted. Cannulated transpedicular screws were placed afterwards.
Outcomes
Clinical outcomes were evaluated using the ODI, visual analogue scale (VAS) for leg and back pain, and short form 36 health survey (SF-36), preoperatively and at 1, 3, 6 and 12 months postoperatively. Disability at 12 months postoperatively was measured using the ODI as the main outcome measure. Change over time and differences between groups were analyzed.
Statistical analysis
Variables were tested for normality. Parametric variables were expressed as mean (standard deviation), non-parametric as median (interquartile range). Categorical variables were described as absolute and relative frequencies. Overall change over time for repeated measures was analyzed with Friedman test. Comparison between groups was carried out with a Student’s t-test and Mann-Whitney’s U for parametric and non-parametric variables, respectively. Effect sizes were calculated between group analyses for parametric variables with Cohen’s d. Analyses, graphs, and tables were performed with R Statistical Software V.3.1.0 (R Foundation for Statistical Computing, Vienna, Austria) and Microsoft Excel 2010. A two-tailed P value of <0.05 was considered significant.
ResultsOther Section
Baseline values and change over time
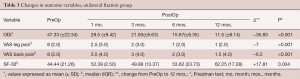
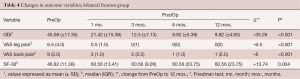
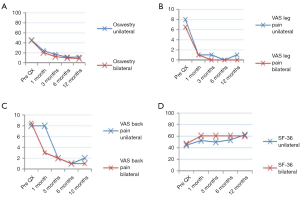
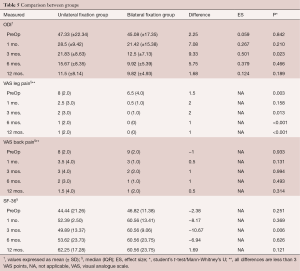
Along the evaluated period of 12 months, the unilateral fixation group had a diminution for the four clinical outcomes scales used: ODI (P<0.001), VAS leg pain (P<0.001), VAS back pain (P<0.001), and SF-36 (P=0.004), Tables 3,4. In the bilateral fixation group we also observed a decrease in the values of the same clinical scales: ODI (P<0.001) (Figure 1A), VAS leg pain (P<0.001) (Figure 1B), VAS back pain (P<0.001) (Figure 1C), and SF-36 (P=0.004) (Figure 1D).
Full table
Full table
Comparisons between groups
ODI was similar preoperatively (P=0.842) and so kept at 1 (P=0.210), 6 (P=0.466), and 12 months (P=0.189); at month 3, unilateral fixed group scored 9.33 points higher than the bilateral fixation group (P=0.023). VAS leg pain. Patients in the unilateral fixation group had an initial pain 1.5 VAS points higher than the bilateral group (P=0.003). At 1-month there was no significant difference (P=0.158). At 3, 6 and 12 months, the unilateral fixation group remained with 2 (P=0.013), 1 (P<0.001) and 1 (P<0.001) VAS points higher respectively than the bilateral fixation group. VAS back pain. Baseline VAS score was similar between groups (P=0.933), and thus maintained in the following evaluations at 1 (P=0.131), 3 (P=0.994), 6 (P=0.493) and 12 months (P=0.314). SF-36 values were alike between groups before surgery (P=0.251) and so continued to be at 1 (P=0.369), 6 (P=0.626) and 12 months (P=0.121); at month 3 patients in the unilateral fixation group had 10.67 less points (P=0.006) than the patients in the bilateral fixation group, Table 5.
Full table
DiscussionOther Section
TLIF is a standard surgical option for patients with isthmic spondylolisthesis and axial pain. Screw fixation accompanies this procedure to provide stability. Bilateral screw fixation was first introduced but further research has demonstrated that unilateral screw fixation is a good option for maintaining stability of the spine. In 1992, Kabins reported similar clinical and radiographic fusion results between unilateral (16 patients) and bilateral (20 patients) procedures in a retrospective series of 36 patients with isolate L4–L5 fusions (8). In 2000, Suk designed a prospective study with 87 patients to compare bilateral with unilateral pedicle screw fixation in one or two fused segments (9). The conclusion was that unilateral is as effective as bilateral screw fixation in all items evaluated: blood loss, operating time, duration of hospital stay, clinical outcomes, complication rates and medical expenses. Recently, Xue compared clinical and radiographic outcomes of 37 patients fixed with unilateral pedicle screws and 43 patients fixed bilaterally; the study was carried-out with randomized methodology concluding that TLIF with unilateral transpedicular screw fixation is a viable treatment option with better results in terms of operative time, blood loss, and hospital stay for single level disease (12). It is clear that in in-vitro models, the rigidity obtained by a bilateral fixation is superior than unilateral. Nevertheless, it has been demonstrated that the absence of certain degree of movement can yield to a fusion failure (7). In our study we found similar results between both groups treated, specially one year after surgery. MI-TLIF with unilateral transpedicular screw fixation is an excellent surgical option to treat patients with low-grade symptomatic lumbar spondylolisthesis (Meyerding grade I, II) and diarthrosis with facetary joint pain. We appreciate that VAS leg pain remained slightly higher in unilateral fixation group compared to the bilateral group. However, this can be explained because unilateral group patients had higher scores indicated in the preoperatively VAS leg pain score. Figure 1B depicts the decrease of radicular pain in both groups evaluated. We also consider that a difference below 3 points in a VAS pain scale might not be clinically significative due to subjective appreciation of pain. We calculated effect sizes for differences between groups for the only parametric variable: ODI. In the Table 5, there are some statistically significant differences among VAS for back and leg scores. However, those differences are very minute (1-2 VAS points); this is a clear case where a statistically significant difference does not represent a meaningful clinical difference. Disability was the main outcome measured. It was evaluated at 1 year after surgical procedure in both groups. Upon the two group comparison, the difference found in the last ODI evaluation at 12 months was 1.68 points which translates to no clinical significance between unilateral and bilateral fixation groups. Although this is not a cost-effectiveness study, it is evident that MI-TLIF with unilateral screw fixation requires less hardware which in turn results in less cost. Finally, the main limitation of this study was the non-randomized nature by itself. Important strengths were that all patients were operated by the same surgeon and that there was a homogenous nature of the sample.
ConclusionsOther Section
In conclusion, our statistical analysis demonstrated that patients with low-grade symptomatic lumbar spondylolisthesis (Meyerding grade I, II) treated with MI-TLIF with unilateral transpedicular screw fixation had similar clinical results than those treated with bilateral at 12 months postoperatively.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: The approval for this work has the number ISCCVM201602, and the informed consent of each patient within the study.
ReferencesOther Section
- Harms J, Rolinger H. A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl). Z Orthop Ihre Grenzgeb 1982;120:343-7. [Crossref] [PubMed]
- Xiao YX, Chen QX, Li FC. Unilateral transforaminal lumbar interbody fusion: a review of the technique, indications and graft materials. J Int Med Res 2009;37:908-17. [Crossref] [PubMed]
- Harris BM, Hilibrand AS, Savas PE, et al. Transforaminal lumbar interbody fusion: the effect of various instrumentation techniques on the flexibility of the lumbar spine. Spine (Phila Pa 1976) 2004;29:E65-70. [Crossref] [PubMed]
- Potter BK, Freedman BA, Verwiebe EG, et al. Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech 2005;18:337-46. [Crossref] [PubMed]
- McAfee PC, Farey ID, Sutterlin CE, et al. The effect of spinal implant rigidity on vertebral bone density. A canine model. Spine (Phila Pa 1976) 1991;16:S190-7. [Crossref] [PubMed]
- McAfee PC, Farey ID, Sutterlin CE, et al. 1989 Volvo Award in basic science. Device-related osteoporosis with spinal instrumentation. Spine (Phila Pa 1976) 1989;14:919-26. [Crossref] [PubMed]
- Goel VK, Lim TH, Gwon J, et al. Effects of rigidity of an internal fixation device. A comprehensive biomechanical investigation. Spine (Phila Pa 1976) 1991;16:S155-61. [Crossref] [PubMed]
- Kabins MB, Weinstein JN, Spratt KF, et al. Isolated L4-L5 fusions using the variable screw placement system: unilateral versus bilateral. J Spinal Disord 1992;5:39-49. [Crossref] [PubMed]
- Suk KS, Lee HM, Kim NH, et al. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine (Phila Pa 1976) 2000;25:1843-7. [Crossref] [PubMed]
- Beringer WF, Mobasser JP. Unilateral pedicle screw instrumentation for minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus 2006;20:E4. [Crossref] [PubMed]
- Deutsch H, Musacchio MJ Jr. Minimally invasive transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Neurosurg Focus 2006;20:E10. [Crossref] [PubMed]
- Xue H, Tu Y, Cai M. Comparison of unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in degenerative lumbar diseases. Spine J 2012;12:209-15. [Crossref] [PubMed]
- Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine 2003;28:S26-35. [Crossref] [PubMed]
- Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 2005;18 Suppl:S1-6. [Crossref] [PubMed]
- Tuttle J, Shakir A, Choudhri HF. Paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Technical note and preliminary report on 47 cases. Neurosurg Focus 2006;20:E5. [Crossref] [PubMed]
- Sonmez E, Coven I, Sahinturk F, et al. Unilateral percutaneous pedicle screw instrumentation with minimally invasive TLIF for the treatment of recurrent lumbar disk disease: 2 years follow-up. Turk Neurosurg 2013;23:372-8. [PubMed]
Contributions: (I) Conception and design: JA Soriano-Sánchez; (II) Administrative support: JA Soriano-Sánchez; (III) Provision of study materials or patients: JA Soriano-Sánchez; (IV) Collection and assembly of data: JA Soriano-Sánchez, J Quillo-Olvera, S Soriano-Solis, ME Soriano-Lopez; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.


