Effect of employment status on length of hospital stay, 30-day readmission and patient reported outcomes after spine surgery
Introduction
Thirty-day hospital readmission rates are increasingly used as a proxy for hospital quality and accounts for approximately $17 billion US dollars in avoidable healthcare expenditure, which are largely borne by the public sector especially Medicare and Medicaid. Accordingly, understanding the drivers as well as the protective factors of unplanned hospital readmissions may help increase quality (decrease in 30-day readmission rates) and reduce healthcare costs.
Several studies have demonstrated a positive correlation between socio-demographic factors such as level of education, socio-economic status, ethnicity and gender on health outcomes. Fewer studies have explored the correlation between pre-operative employment status and post-operative complications profiles, length of hospital stay (LOS), 30-day readmission rates and patient reported outcomes (PROs) after elective spine surgery.
The aim of this study is to assess whether employment status is associated with shorter duration of hospital stay, lower 30-day readmission rates, and improved perception of health status after elective spine surgery.
Methods
The medical records of 360 adult patients undergoing elective spine surgery at a major academic medical center between 2008 and 2010 were retrospectively reviewed. Institutional Review Board approval was obtained prior to study’s initiation. All patients in this study had baseline and 12-month PROs data. The patients were divided into four cohorts by employment status at time of surgery (employed: n=174, unemployed: n=70, retired: n=40, disabled: n=76). We identified all unplanned readmissions within 30 days of discharge after indexed spine surgery.
Demographic variables evaluated included patient age, smoking status, gender, and body mass index (BMI). Co-morbidities included chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), congestive heart failure (CHF), hyperlipidemia (HLD), peripheral vascular disease (PVD), and atrial fibrillation (AFib). Operative variables included length of surgery, number of vertebral levels involved, estimated blood loss (EBL), and urinary output (UOP). Post-operative variables included LOS, urinary tract infection (UTI), pneumonia, deep and superficial surgical site infection (SSI), other infections, deep venous thrombosis (DVT), pulmonary embolism (PE), and 30-day readmission rate. Ambulatory status at discharge was also collected from physical therapy documentation.
PROs metrics were collected and compared between cohorts before surgery and 12-month after surgery. Functional status was determined by the Oswestry disability index (ODI) (1). Neck, back and leg pain were assessed using the Neck/Back/Leg-Pain Visual Analog Scale (VAS-NP, VAS-BP, VAS-LP) (2). SF-36 physical component score (PCS) and mental component score (MCS) was used for the assessment of physical and mental health status, respectively (3). These questionnaires have been validated, widely used and accepted in spine research.
Parametric data were expressed as means ± standard deviation (SD) and compared via ANOVA. Nominal data were compared with the Chi-square test. All tests were two sided and were statistically significant if the P value was less than 0.05. Statistical analysis was performed using JMP-12.0 by SAS.
Results
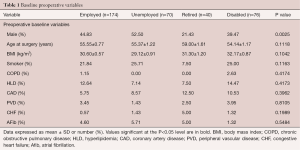
Three hundred and sixty adult patients (employed: n=174, unemployed: n=70, retired: n=40, disabled: n=76) were included in this study. There was no significant difference in age between the groups (employed cohort: 55.55±0.77 years vs. unemployed cohort: 55.37±1.22 years vs. retired cohort: 59.00±1.61 years vs. disabled cohort: 54.14±1.17 years, P=0.11) (Table 1). No significant differences in BMI between both groups were observed (employed cohort: 30.60±0.57 kg/m2vs. unemployed cohort: 29.12±0.91 kg/m2vs. retired cohort: 31.30±1.20 kg/m2vs. disabled cohort: 32.17±0.87 kg/m2, P=0.10) (Table 1). More men were included in the unemployed cohort (52.5%) compared to the employed cohort (44.83%), retired cohort (21.43%), and disabled cohort (39.47%) (Table 1). There were no significant differences between both groups in the prevalence of other co-morbidities such diabetes, COPD, CAD, CHF, HLD, PVD, AFib, and smoking status (Table 1).
Full table
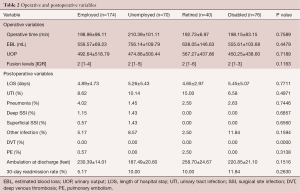
There was no significant difference in mean ± SD operative time (minutes) for the cohorts (employed cohort: 198.96±96.11 minutes vs. unemployed cohort: 210.39±101.11 minutes vs. retired cohort: 192.73±6.97 minutes vs. disabled cohort: 198.15±83.15 minutes, P=0.75) (Table 2). The mean ± SD estimated blood loss (mL) for the groups were similar (employed cohort: 556.57±69.23 mL vs. unemployed cohort: 756.14±109.79 mL vs. retired cohort: 638.05±146.63 mL vs. disabled cohort: 555.61±103.68 mL, P=0.44) (Table 2). There were no significant differences in the median number of levels operated on (P=0.11) (Table 2).
Full table
Thirty-day readmission rates and post-operative complications profile
The 30-day readmission rates were lowest in the cohort of patients that were employed at the time of surgery (employed cohort: 5.17% vs. unemployed cohort: 10% vs. retired cohort: 10% vs. disabled cohort: 11.84%, P=0.26) (Table 2). Patients in the employed- and retired-cohorts had a slightly shorter length of in-hospital stay when compared to unemployed- and disabled-cohorts (employed cohort: 4.89±4.73 days vs. unemployed cohort: 5.26±5.43 days vs. retired cohort: 4.65±2.97 days vs. disabled cohort: 5.45±5.07 days, P=0.26) (Table 2). There was no significant differences between patient cohorts in the ambulatory status at discharge. The number of feet ambulated at discharge were similar between the cohorts (employed cohort: 230.39±14.01 ft. vs. unemployed cohort: 187.49±20.60 ft. vs. retired cohort: 258.70±24.67 ft. vs. disabled cohort: 220.85±21.10 ft., P=0.15) (Table 2). The prevalence of post-operative complications were similar between all cohorts (employed vs. unemployed vs. retired vs. disabled)—UTI (8.62% vs. 10.14% vs. 15.00% vs. 6.58%, P=0.49), pneumonia (4.02% vs 1.45% vs 2.50 vs. 2.63%, P=0.74), deep SSI (1.15% vs. 1.43% vs. 0.00% vs. 0.00%, P=0.68), superficial SSI (0.57% vs. 1.43% vs. 0.00% vs. 0.00%, P=0.65), other infections (5.17% vs. 8.57% vs. 2.50% vs. 11.84%, P=0.15), PE (0.57% vs. 0.00% vs. 2.50% vs. 0.00%, P=0.31) (Table 2). No patient had a DVT (Table 2).
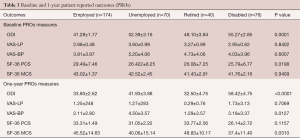
Pre-operative baseline pain, functional disability and quality of life in patients undergoing elective spine surgery with and without depression
The mean ± SD ODI score for employed-, unemployed-, retired-, and disabled-cohorts were 41.28±1.77, 52.39±3.16, 48.10±3.84, and 55.27±2.85, P=0.0001, respectively (Table 3). The pre-operative mean ± SD VAS-LP score for employed-, unemployed-, retired-, and disabled-cohorts were 2.68±0.48, 3.60±0.99, 3.27±0.99, and 2.95±0.62, P=0.84, respectively (Table 3). The pre-operative mean ± SD VAS-BP score for employed-, unemployed-, retired-, and disabled-cohorts were 3.81±3.97, 5.20±4.06, 4.73±4.06, and 4.03±3.96, P=0.60, respectively (Table 3). The pre-operative mean ± SD SF-36 PCS score for employed-, unemployed-, retired-, and disabled-cohorts were 29.49±7.46, 26.422±8.25, 26.08±7.25, and 25.79±6.77, P=0.01, respectively (Table 3). The pre-operative mean ± SD SF-36 MCS score for employed-, unemployed-, retired-, and disabled-cohorts were 43.02±1.37, 42.52±2.45, 41.43±2.91, and 41.76±2.16, P=0.05, respectively (Table 3).
Full table
One-year post-operative pain, functional disability and quality of life in patients undergoing elective spine surgery with and without depression
There were significant differences in 1-year post-operative pain, functional disability and quality of life between the cohorts. The mean ± SD ODI score for employed-, unemployed-, retired-, and disabled-cohorts were 33.80±2.62, 41.93±3.88, 32.50±4.75, and 58.42±4.75, P<0.0001, respectively (Table 3). The pre-operative mean ± SD VAS-LP score for employed-, unemployed-, retired-, and disabled-cohorts were 1.25±248, 1.27±283, 0.29±0.76, and 1.73±3.13, P=0.70, respectively (Table 3). The pre-operative mean ± SD VAS-BP score for employed-, unemployed-, retired-, and disabled-cohorts were 2.11±2.80, 4.50±3.57, 1.29±3.57, and 3.18±3.37, P=0.01, respectively (Table 3). The pre-operative mean ± SD SF-36 PCS score for employed-, unemployed-, retired-, and disabled-cohorts were 33.31±1.49, 31.05±2.22, 33.77±2.56, and 26.14±2.72, P=0.11, respectively (Table 3). The pre-operative mean ± SD SF-36 MCS score for employed-, unemployed-, retired-, and disabled-cohorts were 45.52±14.63, 40.06±15.14, 48.83±10.17, and 37.4±11.40, P=0.03, respectively (Table 3).
Discussion
In this retrospective cohort study of patients undergoing elective spine surgery, our study demonstrates that pre-operative employment status was associated with shorter duration of hospital stay and lower 30-day readmission rates.
Few studies have investigated the relationship between employment status prior to surgery and post-operative clinical outcomes, with mixed results. In a prospective observational study of 109 patients undergoing anterior lumbar fusion, Anderson et al. demonstrated that patients working prior to surgery had a greater degree of pain relief than nonworking patients (4). North et al., in a retrospective 5-year follow-up study of 102 patients undergoing repeated operation for failed back surgery syndrome found that preoperative employment status was associated with favorable outcomes (5). In another retrospective study evaluating 71 cases of posterior lumbar arthrodesis, Agazzi et al. demonstrated a significant association between preoperative employment status and superior clinical outcomes (P=0.03) (6). Similarly, In a study of 496 patients that underwent coronary bypass surgery, Zyzanski et al. demonstrated that patients who were employed preoperatively and returned to work after surgery had decreased re-hospitalizations and bedridden days when compared to unemployed patients (7). Analogous to these studies, our study demonstrated that employed patients had lower 30-day hospital readmission rates as well as lower post-operative functional disability scores compared to unemployed patients.
Conversely, in a systematic review of 25 studies evaluating outcomes after lumbar spine surgery, Celestin et al. found no consistent relationship between employment status and treatment outcomes (8). Silvers et al. in a retrospective study of 258 consecutive patients that underwent decompressive lumbar laminectomies observed no significant correlation between employment status and clinical outcomes (9). Similarly, Bourne et al. in another retrospective study of 1,703 patients who underwent primary total knee arthroplasty, found no significant differences in post-operative satisfaction based on perioperative employment status (10).
There is a paucity of data investigating the effect of pre-operative employment status on duration of hospital stay and 30-day readmission rates. In a retrospective study of 112 patients who underwent revision posterior lumbar spine surgery, Zheng et al. found an association with unemployment status and increased LOS (11). In another retrospective study of 1,222 consecutive patients who underwent Roux-en-Y gastric bypass surgery, Kellogg et al. demonstrated that unemployed, disabled, or retired patients were more likely to be readmitted or seen in the ED than employed, non-disabled, or non-retired patients (12). Our findings, which are consistent with these studies, demonstrates that employed patients had a shorter duration of in-hospital stay as well as lower 30-day hospital readmission rate after elective spine surgery.
It is important to note that association does not imply causality, and as such one can only speculate as to the reasons for the higher readmission rates in the unemployed cohort. Several quantitative studies have demonstrated the correlation between employment and an individual’s physical and mental well-being. Employment affects key components of mental health including a patient’s sense of self-worth, purpose and identity. Presumably, employed patients may have a greater desire to return to their social and professional networks, and as such, may have more realistic post-operative expectations and may be more likely to adhere with post-operative treatment regiments; all of which contribute to shorter duration of hospital stay, lower readmission rates and improved patient satisfaction with healthcare received.
This study has limitations, ensuing possible implications for its interpretation. First, this data was acquired via chart reviews and are limited by what was recorded during the episode of care and are subject to the weaknesses of a retrospective analysis. Second, it is possible that patients may have been readmitted to other hospitals, underestimating the observed readmission rates. Third, the number of patients that re-presented to the hospital but were placed in an observational status rather than readmitted was not known for this study. The duration and quality of employment status was also not known which precludes us from making firm conclusions based on the observed results. Despite these limitations, this study suggests that employment status was associated with decreased in-patient hospital stays and 30-day readmission rates. More studies are needed to corroborate our findings.
Conclusions
Our study suggests that employment status may be associated with shorter duration of hospital stay, lower 30-day readmission rates and a greater extent of functional improvement after elective spine surgery. Future interventions to reduce unplanned readmission should consider pre-operative employment status.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board approval was obtained prior to study’s initiation (No. Pro00066331) and written informed consent was obtained from all patients.
References
- Fairbank JC. Oswestry disability index. J Neurosurg Spine 2014;20:239-41. [Crossref] [PubMed]
- Zanoli G, Strömqvist B, Jönsson B. Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine (Phila Pa 1976) 2001;26:2375-80. [Crossref] [PubMed]
- Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976) 2000;25:3130-9. [Crossref] [PubMed]
- Anderson PA, Schwaegler PE, Cizek D, et al. Work status as a predictor of surgical outcome of discogenic low back pain. Spine (Phila Pa 1976) 2006;31:2510-5. [Crossref] [PubMed]
- North RB, Campbell JN, James CS, et al. Failed back surgery syndrome: 5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery 1991;28:685-90; discussion 690-1. [Crossref] [PubMed]
- Agazzi S, Reverdin A, May D. Posterior lumbar interbody fusion with cages: an independent review of 71 cases. J Neurosurg 1999;91:186-92. [PubMed]
- Zyzanski SJ, Rouse BA, Stanton BA, et al. Employment changes among patients following coronary bypass surgery: social, medical, and psychological correlates. Public Health Rep 1982;97:558-65. [PubMed]
- Celestin J, Edwards RR, Jamison RN. Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation: a systematic review and literature synthesis. Pain Med 2009;10:639-53. [Crossref] [PubMed]
- Silvers HR, Lewis PJ, Asch HL. Decompressive lumbar laminectomy for spinal stenosis. J Neurosurg 1993;78:695-701. [Crossref] [PubMed]
- Bourne RB, Chesworth BM, Davis AM, et al. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57-63. [Crossref] [PubMed]
- Zheng F, Cammisa FP Jr, Sandhu HS, et al. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine (Phila Pa 1976) 2002;27:818-24. [Crossref] [PubMed]
- Kellogg TA, Swan T, Leslie DA, et al. Patterns of readmission and reoperation within 90 days after Roux-en-Y gastric bypass. Surg Obes Relat Dis 2009;5:416-23. [Crossref] [PubMed]
Contributions: (I) Conception and design: O Adogwa, AA Elsamadicy, J Cheng, CA Bagley; (II) Administrative support: J Fialkoff, AI Mehta, RA Vasquez, IO Karikari; (III) Provision of study materials or patients: O Adogwa, AA Elsamadicy, J Cheng, CA Bagley; (IV) Collection and assembly of data: J Fialkoff, AI Mehta, RA Vasquez, IO Karikari; (V) Data analysis and interpretation: O Adogwa, AA Elsamadicy, J Cheng, CA Bagley; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.


