Assessing the effectiveness of routine use of post-operative in-patient physical therapy services
Introduction
In recent years, healthcare costs have been dramatically increasing at a disparaging rate. The emphasis of quality, over quantity, of care has been a growing national effort, especially by the Centers of Medicare & Medicaid Services (CMS) in efforts to reduce soaring healthcare expenditures (1). In surgery, length of hospital stay (LOS) and 30-day readmission rates has become a proxy that is used to value both the quality and financial impact of procedures performed by hospitals (2,3). With a growing number of spinal procedures being performed yearly, identifying factors that may reduce preventable healthcare costs is necessary (1).
Immobility, or reduced mobility, after spine surgery has been associated with decreased functionality and increased LOS (3-5). Hospital services, such as physical therapy (PT), are routinely utilized to promote recovery and reduce functional declination. Previous studies have reported that early in-patient PT improved pain and disability, while decreasing the incidence of perioperative complications (4,5). In a prospective randomized trial of 60 patients who underwent surgery for hip fracture, Oldmeadow et al. demonstrated that patients participating PT ambulation re-education program starting on post-operative days 1–2, walked further, required less assistance and were more likely to be discharged earlier (6). As the number of elective spinal surgeries being performed is increasing, it is essential to understand the role of immediate post-operative in-patient PT on patient outcomes. However, the effects of in-patient PT services on post-operative outcomes after elective spine surgery remain unclear.
The aim of this study is to determine the effects of immediate in-patient post-operative ambulation with the PT on discharge ambulation distance, post-operative patient complications profiles, and 30-day readmission rates, following elective spine surgery.
Methods
This was an ambispective review of 274 medical records patients of adults undergoing elective spine at a major academic medical center from 2008 to 2010. Institutional review board (IRB) approval was obtained prior to study’s initiation (Duke IRB Protocol: 00066331). All patients underwent elective spine fusion for degenerative disk disease or spinal deformity. The patients were divided into 2 cohorts by ambulatory assistance, either formal in-patient PT services or nurse-assisted ambulation (No PT) during the post-operative in-patient stay (No PT: n=87, PT: n=187).
Demographic variables evaluated included patient age, gender, and body mass index (BMI). Co-morbidities included congestive heart failure (CHF), hypertension (HTN), hyperlipidemia (HLD), peripheral vascular disease (PVD), and atrial fibrillation (AFib). Smoking status was also collected on each patient. Operative variables included length of surgery, number of vertebral levels involved, estimated blood loss (EBL), urinary output (UOP), and the use of intraoperative steroids. Post-operative complications included LOS, urinary tract infection (UTI), pneumonia, deep venous thrombosis (DVT), pulmonary embolism (PE), post-operative time duration to consuming oral medications (post-op to oral), and 30-day readmission rate. For the PT cohort, first and last ambulation distance of hospitalization was collected.
Parametric data were expressed as means ± standard deviation (SD) and compared via the Student t-test. Pearson’s correlation was used to assess the relationship between first and last ambulatory status. All tests were two sided and were statistically significant if the P value was less than 0.05. Statistical analysis was performed using JMP®, Version 12 (SAS Institute Inc., Cary, NC).
Results
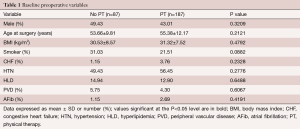
A total of 274 adult patients (No PT cohort: n=87, PT cohort: n=187) were included in this ambispective study. There was no significant difference in age between both groups (No PT: 53.66±9.81 years vs. PT: 55.38±12.17 years, P=0.2121) (Table 1). There was no significant difference in BMI between the cohorts (No PT: 30.53±8.57 kg/m2vs. PT: 31.32±7.52 kg/m2, p=0.4792) (Table 1). The proportion of males was similar between the cohorts (No PT: 49.42% male vs. PT: 43.01% male, P=0.3209) (Table 1). There were no significant differences in the prevalence of other co-morbidities, such as HTN, HLD, PVD, AFib and smoking status (Table 1).
Full table
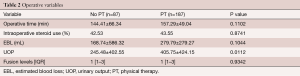
The mean ± SD operative time (minutes) was not significantly different between the cohorts (No PT: 144.407±66.34 min vs. PT: 157.29±49.04 min, P=0.1102) (Table 2). The use of intraoperative steroids was not significant between the cohorts (No PT: 42.53% vs. PT: 43.55%, P=0.8741) (Table 2). The mean ± SD EBL (mL) was not significantly different between the cohorts (No PT: 168.74±586.32 mL vs. PT: 279.79±279.27 mL, P=0.1044) (Table 2). There were differences in mean ± SD UOP (mL) between the cohorts (No PT: 245.48±402.55 mL vs. PT: 405.75±424.15 mL, P=0.0112). The operative fusion levels were similar between the cohorts (P=0.9342) (Table 2).
Full table
Post-operative complications profile and 30-day readmission rates
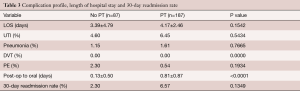
There were no significant differences in the incidence of UTI, pneumonia, DVT, and PE–UTI (No PT: 4.603% vs. PT: 6.45%, P=0.5434), pneumonia (No PT: 1.15% vs. PT: 1.61%, P=0.7665), DVT (No PT: 0.0% vs. PT: 0.0%, p=0), PE (No PT: 2.30% vs. PT: 0.54%, P=0.1934) (Table 3). There was a significant difference in post-op to oral, with the PT cohort experiencing a longer time period (No PT: 0.133±0.503 days vs. PT: 0.81±0.870 days, P<0.0001) (Table 3). There was no significant differences in LOS between the cohorts, but the PT-cohort trended to have a longer LOS (No PT: 3.39±4.79 days vs. PT: 4.17±2.46 days, P=0.1542) (Table 3). There was not a significant difference in 30-day unplanned readmission (No PT: 2.30% vs. PT: 6.57%, P=0.1349) (Table 3).
Full table
Ambulation status of patients undergoing PT
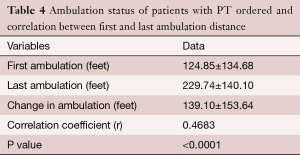
There was a 2-fold increase in ambulation status from the first and last ambulation distance of patients receiving PT services prior to discharge (1st ambulation: 124.85±134.68 feet, last ambulation: 229.74±140.103 feet, change in ambulation: 139.10±153.64 feet) (Table 4). There was a positive correlation between first and last ambulation distance in patients receiving PT services [correlation coefficient (r) =0.4683, P<0.0001] (Table 4).
Full table
Discussion
In this ambispective cohort study of patients undergoing elective spinal surgery, we demonstrate that patients that receive in-patient PT services compared to nurse assisted services had a modest increase in LOS and post-operative duration to consuming oral medications, without any significant reduction in peri-operative complications profile or 30-day readmission rates. However, we did identify that PT services lead to 2-fold increase in ambulation distance during the post-operative hospital course.
The consensus of requiring formal PT services after surgery is unclear. Previous studies have associated the use of early PT services with improved short-term outcomes and reduced LOS and time to independent mobility. In a prospective randomized control trial of 86 patients who underwent elective hip or knee arthroplasty, Munin et al. demonstrated that total LOS, time to functional milestones, and the associated cost of medical services was reduced when in-patient PT services were provided on post-operative day 3 compared to day 7 for high-risk patients (4). In another prospective randomized, single-blind, controlled trial of 30 patients who underwent lumbar microdiscectomy, Newsome et al. found that immediate PT commencing two hour following the operation led to a faster times to independent mobility upon discharge (5). Similarly, in a retrospective study of 408 patients who underwent elective total hip arthroplasty (THA), Juliano et al. determined that PT beginning the day of surgery led to a reduction of LOS with a larger percentage of the cohort achieving independence (7). Our study demonstrated that patients receiving in-patient PT services improve greatly in ambulatory status prior to discharge.
Conversely, there are other studies, which have challenged the need of formal PT services after surgery. In a multicenter randomized clinical trial of 82 patients who underwent lumbar spinal fusion, Oestergaard et al. evaluated rehabilitation starting at 6 vs. 12 weeks and determined that patients beginning PT at 12 weeks had a lower oswestry disability index (ODI) at both 6-month and 1-year follow ups compared to the 6-week cohort (8). Additionally, the authors reported that initiation rehabilitation at 6-weeks was more costly, challenging the cost-effectiveness of such programs (9). Similarly, in a systematic review of 22 randomized controlled trials (2,053 patients) assessing various rehabilitation protocol following lumbar disc surgery for lumbar disc herniation, Ooterhuis et al. concluded that there was very low quality evidence exists supporting the benefits of beginning a rehabilitation program immediately after surgery (10). Analogously, our study demonstrated that patients undergoing in-patient PT services actually had a modest increase in LOS and post-operative duration to consuming oral medications, without any significant reduction in peri-operative complications profile or 30-day readmission rates.
While prior studies associated the effectiveness of PT services, other studies analyzed the differences in healthcare cost. In a randomized clinical trial evaluating the cost-effectiveness of accelerated peri-operative care and rehabilitation clinical pathway 9-month post-operatively of 87 patients who underwent THA, total knee arthroplasty (TKA), or unicompartmental knee arthroplasty, Larsen et al. found that patients the cost of the accelerated cohort was significantly lower than the rehabilitation pathway (11). Similarly, in a systematic review of 11 prospective and retrospective studies (3,995 patients) assessing the cost-effectiveness of accelerated clinical pathways for TKA and THA pat, Kim et al. determined the median reduction of cost was 11% and standard care (12). In another retrospective analysis evaluating the relationship between the utilization of PT and clinical outcomes of 7,495 patients undergoing THA, Freburger et al. demonstrated that, on average, PT services accounted for 3% of the total cost of inpatient care, ranging from 1% to 14% (13). Furthermore, the authors found that for every 1% increase in PT spending there was an associated $76 reduction in total health care cost (13).
In spine, more studies are necessary to understand the cost-benefits and effectiveness of utilizing in-patient PT services after spine surgery. Other surgical specialties, such as orthopedic joint replacement surgery, have implemented early-ambulation protocols in-patient PT services to improve patient recovery time after surgery (4,7,14). However, there is a limited number of studies evaluating the effectiveness of in-patient PT services and early-ambulation in spine surgery (10). Further studies are needed in order determine the effects of early PT on LOS, ambulation, and 30-day readmission rate; as well as, short- and long-term clinical outcomes.
This study has limitations, ensuing possible implications for its interpretation. While pre- and perioperative variables were prospectively collected, data was retrospectively analyzed for the purposes of this study, therefore are subject to the weaknesses of a retrospective analysis. Physical therapy was not standardized for each patient and was determined individually by the interactions with the PT team and the patient. All patients were required to reach a desired threshold met for safe discharge from the hospital. Despite these limitations, this study has demonstrated that in-patient PT services compared to nurse assisted led to a slight increase in hospital LOS with no significant reductions in post-operative complication profile and 30-day readmission rates.
Conclusions
Our study suggests that the routine use of the PT services compared to nurse-assisted ambulation programs is associated with a modest increase in the duration of hospital stay without any significant reduction in peri-operative complications profile. In a health conscious healthcare climate, appropriate screening mechanisms and risk stratification should be performed to optimize utilization of post-operative in-patient PT services.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ugiliweneza B, Kong M, Nosova K, et al. Spinal surgery: variations in health care costs and implications for episode-based bundled payments. Spine (Phila Pa 1976) 2014;39:1235-42. [Crossref] [PubMed]
- Krell RW, Girotti ME, Dimick JB. Extended length of stay after surgery: complications, inefficient practice, or sick patients? JAMA Surg 2014;149:815-20. [Crossref] [PubMed]
- Cohen ME, Bilimoria KY, Ko CY, et al. Variability in length of stay after colorectal surgery: assessment of 182 hospitals in the national surgical quality improvement program. Ann Surg 2009;250:901-7. [Crossref] [PubMed]
- Munin MC, Rudy TE, Glynn NW, et al. Early inpatient rehabilitation after elective hip and knee arthroplasty. JAMA 1998;279:847-52. [Crossref] [PubMed]
- Newsome RJ, May S, Chiverton N, et al. A prospective, randomised trial of immediate exercise following lumbar microdiscectomy: a preliminary study. Physiotherapy 2009;95:273-9. [Crossref] [PubMed]
- Oldmeadow LB, Edwards ER, Kimmel LA, et al. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg 2006;76:607-11. [Crossref] [PubMed]
- Juliano K, Edwards D, Spinello D, et al. Initiating physical therapy on the day of surgery decreases length of stay without compromising functional outcomes following total hip arthroplasty. HSS J 2011;7:16-20. [Crossref] [PubMed]
- Oestergaard LG, Nielsen CV, Bünger CE, et al. The effect of early initiation of rehabilitation after lumbar spinal fusion: a randomized clinical study. Spine (Phila Pa 1976) 2012;37:1803-9. [Crossref] [PubMed]
- Oestergaard LG, Christensen FB, Nielsen CV, et al. Early versus late initiation of rehabilitation after lumbar spinal fusion: economic evaluation alongside a randomized controlled trial. Spine (Phila Pa 1976) 2013;38:1979-85. [Crossref] [PubMed]
- Oosterhuis T, Costa LO, Maher CG, et al. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev 2014.CD003007. [PubMed]
- Larsen K, Hansen TB, Thomsen PB, et al. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am 2009;91:761-72. [Crossref] [PubMed]
- Kim S, Losina E, Solomon DH, et al. Effectiveness of clinical pathways for total knee and total hip arthroplasty: literature review. J Arthroplasty 2003;18:69-74. [Crossref] [PubMed]
- Freburger JK. An analysis of the relationship between the utilization of physical therapy services and outcomes of care for patients after total hip arthroplasty. Phys Ther 2000;80:448-58. [PubMed]
- Larsen K, Sørensen OG, Hansen TB, et al. Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop 2008;79:149-59. [Crossref] [PubMed]


