Effects of immediate post-operative pain medication on length of hospital stay: does it make a difference?
Introduction
In the past decade, there has been a national effort to decrease the soaring health care expenditures and identify quality metrics to value hospital care. In surgery, length of hospital stay (LOS) has progressively become a cost-metric that is used to value the financial impact of procedures performed by a hospital (1,2). Along with economic considerations, LOS has also been used as a proxy for quality and even a predictor of morality after particular major surgeries (3,4). Therefore, identifying variables and risk-factors that lead to increased LOS is necessary to reduce the disparaging health care costs and quality of care after surgery.
In particular, post-operative pain has been associated with increased LOS and decrease patient reported outcomes (PROs). In a retrospective study of 411 patients who underwent orthopedic surgery, Morrison et al. found that post-operative pain scores was significantly associated with increased LOS and decreased ambulation status (5). Furthermore, prior studies have associated increased post-operative narcotic consumption with increasing post-operative pain (6). Patient-controlled analgesics (PCA) morphine, fentanyl, and hydromorphone are common post-operative pain medications that are used frequently after spine surgery. Appropriately control post-operative pain, while increasing patient satisfaction is a factor that providers and institutions are becoming increasingly emphasized (7). However, as prior studies have found associations between post-operative pain and LOS, the effect of the immediate post-operative pain medication administered is relatively unknown.
The aim of this study is to determine the effects of different immediate post-operative pain medications on the post-operative complications profile, LOS, and PROs after elective spine surgery.
Methods
This was a retrospective analysis of a prospectively collected database. A total of 230 medical records patients were retrospectively reviewed of adult patients undergoing elective spine surgery at a major academic medical center from 2008 to 2010. Institutional review board approval was obtained prior to study’s initiation (Duke IRB Protocol: 00066331). All patients underwent elective spine fusion for degenerative disk disease or spinal deformity. All patients in this study had baseline, 6- and 12-month PROs data. The operating surgeon decided the postoperative pain medication with input by the anesthetist. Patients were categorized by the immediate post-operative pain medication they were given (morphine: n=98, fentanyl: n=61, hydromorphone: n=71). We identified all unplanned readmissions within 30 days of discharge after indexed spine surgery.
Demographic variables evaluated included patient age, gender, and body mass index (BMI). Co-morbidities included diabetes, chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), peripheral vascular disease (PVD), hypertension (HTN), atrial fibrillation (AFib), and congestive heart failure (CHF). Other preoperative variables collected were smoking status and baseline albumin level. Operative variables included length of surgery, number of vertebral levels involved, estimated blood loss (EBL) and urinary output (UOP). Post-operative complications included LOS, urinary tract infection (UTI), pneumonia, deep and superficial surgical site infections (SSI), deep venous thrombosis (DVT), pulmonary embolism (PE), cardio-pulmonary arrest, and 30-day readmission rate. Other post-operative variables collected were number of feet walked at first ambulation and number of feet walked at discharge date.
Patient reported outcomes metrics were collected and compared between both cohorts (morphine: n=98, fentanyl: n=61, hydromorphone: n=71) before surgery, then 3- and 6-month after surgery. Functional status was determined by the Oswestry Disability Index (ODI) (8). Neck, back and leg pain were assessed using the neck/back/leg-pain visual analog scale (VAS-NP, VAS-BP, VAS-LP) (9). SF-36 physical component score (PCS) and mental component score (MCS) was used for the assessment of physical and mental health status, respectively (10). These questionnaires have been validated, widely used and accepted in spine research.
Parametric data were expressed as means ± standard deviation (SD) and compared via ANOVA. Nominal data were compared with the chi-square test. All tests were two sided and were statistically significant if the P value was less than 0.05. Statistical analysis was performed using JMP-12.0 by SAS.
Results
A total of 230 adult patients (morphine: n=98, fentanyl: n=61, hydromorphone: n=71) were included. There was no significant difference in age between all groups (morphine: 56.53±12.62 years vs. fentanyl: 58.80±13.56 years vs. hydromorphone: 54.32±13.85 years, P=0.1555) (Table 1). No significant differences in BMI between groups were observed (morphine: 29.65±6.19 vs. fentanyl: 30.80±7.42 vs. hydromorphone: 29.87±7.63, P=0.5882) (Table 1). More males were in the morphine cohort, compared to the fentanyl and hydromorphone cohorts (morphine: 42.86% male vs. fentanyl: 40.98% male vs. hydromorphone: 36.62% male, P=0.7134) (Table 1). No significant differences in albumin between groups were observed (morphine: 3.72±0.17 vs. fentanyl: 3.47±0.18 vs. hydromorphone: 3.51±0.16, P=0.5465) (Table 1). No significant differences in chronic steroid use between groups were observed (morphine: 12.24% vs. fentanyl: 11.48% vs. hydromorphone: 14.08%, P=0.8944) (Table 1). There were no significant differences between groups in the prevalence of other co-morbidities such diabetes, COPD, HLD, CAD, PVD, CHF HTN, AFib, and smoking status (Table 1).

Full table
There was no significant difference in mean ± SD duration of surgery (minutes) for the cohorts (morphine: 176.12±8.48 mins vs. fentanyl: 202.57±10.74 mins vs. hydromorphone: 194.94±9.96 mins, P=0.1211) (Table 1). The mean ± SD EBL (mL) for the groups were (morphine: 523.2±641.34 mL vs. fentanyl: 883.83±1,289.27 mL vs. hydromorphone: 714.09±1,049.27 mL, P=0.0871) (Table 1). There were no significant difference in the median number of levels operated on (P=0.0672) and UOP (P=0.4617) between patient cohorts (Table 1).
30-day readmission rates and post-operative complication profile
There was no significant difference in 30-day readmission rates between patient cohorts, but morphine patients tended towards lower rates (morphine: 5.10% vs. fentanyl: 11.48% vs. hydromorphone: 11.27%, P=0.2492) (Table 1). The morphine-cohort had a decreased length of in-hospital when compared to the fentanyl and hydromorphone cohorts (morphine: 4.18±0.43 days vs. fentanyl: 5.56±0.54 days vs. hydromorphone: 5.69±0.50 days, P=0.0376) (Table 1). Number of feet ambulated at discharge were similar between the cohorts (morphine: 244.88±16.49 ft. vs. fentanyl: 195.60±20.32 ft. vs. hydromorphone: 215.26±18.4 ft., P=0.1566) (Table 1). However there was a significance difference in number of feet first ambulated (morphine: 118.44±18.15 ft. vs. fentanyl: 59.26±20.78 ft. vs. hydromorphone: 125.91±19.85 ft., P=0.0420) (Table 1).
The prevalence of post-operative complications were similar between all cohorts except UTI which was significant (morphine vs. fentanyl vs. hydromorphone) UTI (5.15% vs. 16.39% vs. 5.63%, P=0.0277), pneumonia (1.03% vs. 3.28% vs. 2.82%, P=0.5830), deep SSI (1.02% vs. 3.28% vs. 1.41%, P=0.5522), superficial SSI (0.87% vs. 1.64% vs. 0.00%, P=0.5863), other infections (5.10% vs. 6.56% vs. 5.63%, P=0.9280) (Table 1). No patient had a DVT or PE (Table 1).
Pre-operative baseline pain, functional disability and quality of life in patients undergoing elective spine surgery
There were no significant differences in baseline functional disability and quality of life between the cohorts. The mean ± SD ODI score for morphine, fentanyl, and hydromorphone cohorts were 47.16±2.55, 45.00±3.20, 50.16±3.16, P=0.5152, respectively (Table 2). The mean ± SD VAS-NP score for morphine, fentanyl, and hydromorphone cohorts were 2.74±1.35, 5.68±2.18, 6.71±1.75, P=0.1750, respectively (Table 2). The mean ± SD VAS-LP score for morphine, fentanyl, and hydromorphone cohorts were 4.09±0.70, 2.67±1.19, 3.88±1.00, P=0.5845, respectively (Table 2). The mean ± SD VAS-BP score for morphine, fentanyl, and hydromorphone cohorts were 4.56±0.69, 5.17±1.15, 5.83±0.94, P=0.5484, respectively (Table 2). The mean ± SD SF-36 PCS score for morphine, fentanyl, and hydromorphone cohorts were 28.07±1.09, 28.64±1.33, 26.00±1.30, P=0.3192, respectively (Table 2). The mean ± SD SF-36 MCS score for morphine, fentanyl, and hydromorphone cohorts were 45.14±1.72, 43.21±2.11, 41.20±2.10, P=0.3496, respectively (Table 2).
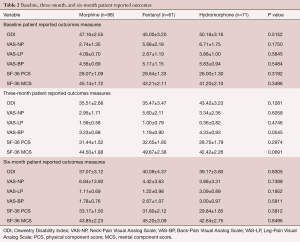
Full table
3-month post-operative pain, functional disability and quality of life in patients undergoing elective spine surgery
There were no significant differences in 3-month post-operative pain, functional disability and quality of life between the cohorts. The mean ± SD ODI score for morphine, fentanyl, and hydromorphone cohorts were 35.51±2.68, 35.47±3.47, 43.42±3.23, P=0.1281, respectively (Table 2). The mean ± SD VAS-NP score for morphine, fentanyl, and hydromorphone cohorts were 2.95±1.71, 5.60±2.11, 3.34±2.36, P=0.6058, respectively (Table 2). The mean ± SD VAS-LP score for morphine, fentanyl, and hydromorphone cohorts were 1.59±0.58, 1.00±0.79, 0.36±0.82, P=0.4746, respectively (Table 2). The mean ± SD VAS-BP score for morphine, fentanyl, and hydromorphone cohorts were 3.23±0.68, 1.19±0.90, 4.33±0.93, P=0.0545, respectively (Table 2). The mean ± SD SF-36 PCS score for morphine, fentanyl, and hydromorphone cohorts were 31.44±1.52, 32.65±1.85, 28.75±1.79, P=0.2974, respectively (Table 2). The mean ± SD SF-36 MCS score for morphine, fentanyl, and hydromorphone cohorts were 44.50±1.88, 49.87±2.38, 42.42±2.26, P=0.0691, respectively (Table 2).
6-month post-operative pain, functional disability and quality of life in patients undergoing elective spine surgery
There were no significant differences in in 6-month post-operative pain, functional disability and quality of life between the cohorts. The mean ± SD ODI score for morphine, fentanyl, and hydromorphone cohorts were 37.07±3.12, 40.09±4.37, 39.17±3.80, P=0.8305, respectively (Table 2). The mean ± SD VAS-NP score for morphine, fentanyl, and hydromorphone cohorts were 6.84±13.90, 4.42±3.63, 3.88±3.31, P=0.7388, respectively (Table 2). The mean ± SD VAS-LP score for morphine-, fentanyl-, and hydromorphone-cohorts were 1.11±0.69, 1.22±0.98, 3.09±0.89, P=0.1952, respectively (Table 2). The mean ± SD VAS-BP score for morphine-, fentanyl-, and hydromorphone-cohorts were 1.78±0.76, 2.67±1.07, 3.00±0.97, P=0.5811, respectively (Table 2). The mean ± SD SF-36 PCS score for morphine-, fentanyl-, and hydromorphone-cohorts were 33.17±1.50, 31.80±2.12, 29.84±1.85, P=0.3812, respectively (Table 2). The mean ± SD SF-36 MCS score for morphine-, fentanyl-, and hydromorphone-cohorts were 43.85±2.23, 45.20±3.09, 42.84±2.75, P=0.8496, respectively (Table 2).
Discussion
In this retrospective cohort study, our study demonstrates that the choice of immediate post-operative pain medication administered was associated with varying LOS after elective spine surgery. Specifically, we found that patients who are administered PCA morphine immediately after surgery had a shorter LOS, compared to patients administered fentanyl or hydromorphone.
Previous studies have demonstrated various associations between the efficacies of different pain medications on post-operative pain and complication profiles after surgery. However, most studies do not find any differences. In a prospectively, randomized-controlled trial of 636 patients who underwent a major surgery, Viscusi et al. found that there was no significant differences in pain satisfaction after 24 hrs between PCA fentanyl versus PCA morphine (P=0.36) (11). Furthermore, the authors also found no significant differences in the last VAS score measured (P=0.45) (11). Similarly, in another prospective study of 50 gynecological surgery patients receiving either PCA morphine or PCA hydromorphone after surgery, Hong et al. found no significant differences in the side effect profiles between the cohorts, which included nausea, vomiting, or pruritus (12). Furthermore, the authors showed no differences in post-operative pain scores 8 hours after surgery (12). Conversely, there are some studies that identified differences in complication profiles between different post-operative pain medications. In a prospective study of 90 children who were administered either morphine vs. fentanyl vs. hydromorphone after orthopedic surgery, Goodarzi et al. demonstrated that patients administered morphine after surgery experienced higher rates of respiratory depression, prolonged somnolence, urinary retention than patients who were administered fentanyl or hydromorphone (13). Furthermore, the authors concluded that hydromorphone was associated with the least side-effects compared to morphine and fentanyl (13). Our study did not demonstrate a difference in post-operative PROs, but did show an increased complication incidence of UTI in the fentanyl cohort compared to the other cohorts.
There are not many studies that have demonstrated differences in LOS based on the type of post-operative pain medication administered. In a retrospective cohort study of 329 patients who underwent abdominal surgery and whose post-operative pain regiment was either acetaminophen versus non-acetaminophen (i.e., morphine, fentanyl, and hydromorphone), Madere et al. showed no significant differences in LOS between the cohorts. However, the authors did observe a significant difference in pain scales, with the non-acetaminophen cohort having lower pain (14). Interestingly, in a study of 174 patients who underwent total joint arthroplasty, Sing et al. demonstrated that patients who are preoperatively opioid users have significantly longer LOS when compared to patients who were not opioid users (15). Our understanding of how pain medications effect LOS remains relatively unknown. However, our study demonstrated that patients who were administered morphine had a shorter LOS, compared to patients who were administered fentanyl or hydromorphone.
Other various studies have attempted to find an association between different administration techniques of pain medication regiments and LOS; however, there are conflicting results. In a retrospective study of 198 undergoing surgery, Brown et al. did not find a significant difference in LOS between patients who were administered their pain medication PCA vs. non-PCA (16). However, the authors did show that patients on PCA used significantly more medication than patients on a non-PCA (16). Conversely, in another study identifying the use of PCA and intramuscular (IM) analgesia, Conner et al. demonstrated that patients that used PCA had a shorter LOS compared to patients who received their analgesia via IM (17). In a retrospective study of 50 consecutive patients who underwent posterior spinal instrumentation and fusion, Van Boerum et al. found that patients who received their analgesia via epidural were discharged earlier than patients who were on PCA (18). Conversely, in a prospective study of 74 patients who underwent lumbar spinal fusion, Fisher et al. demonstrated no significant difference in overall patient satisfaction and LOS between patients receiving their analgesia via PCA versus epidural (19).
Overall, there is no consensus on the type and administration technique of post-operative pain medications to significantly reduce post-operative pain. The selection of post-operative analgesia is a complex decision made by the provider that may need to incorporate various factors including patient characteristics and surgical approach to identify the optimal regiment. There have been some studies suggesting that preoperative subjective pain tolerance strongly predicts acute pain level after surgery (20). However, further studies are necessary to adequately identify the most appropriate pain regiment and type of pain medication that will achieve superior post-operative outcomes and decrease LOS after surgery.
This study has limitations, ensuing possible implications for its interpretation. Patients were not randomized to the three test conditions (morphine, fentanyl, hydromorphone), which may contribute to biased selection. Additionally, the amount of analgesic titrated into each patient were not standardized for each group. The duration and quality of pain were not observed in this study. While pre- and perioperative variables were prospectively recorded into the study registry at the time of surgery, these variables were retrospectively analyzed for the purpose of this study and are subject to the weakness of a retrospective analysis. Despite these limitations, this study has demonstrated that the choice of opioid analgesic might have implications in postoperative recovery and LOS.
Conclusions
Our study demonstrates that the choice of immediate post-operative pain medication can make a difference in the hospital course for patients. Identifying these types of factors might help increase patient care and reduce health care costs.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional review board approval was obtained prior to study’s initiation (Duke IRB Protocol: 00066331).
References
- Krell RW, Girotti ME, Dimick JB. Extended length of stay after surgery: complications, inefficient practice, or sick patients? JAMA Surg 2014;149:815-20. [Crossref] [PubMed]
- Cohen ME, Bilimoria KY, Ko CY, et al. Variability in length of stay after colorectal surgery: assessment of 182 hospitals in the national surgical quality improvement program. Ann Surg 2009;250:901-7. [Crossref] [PubMed]
- Wright CD, Gaissert HA, Grab JD, et al. Predictors of prolonged length of stay after lobectomy for lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database risk-adjustment model. Ann Thorac Surg 2008;85:1857-65; discussion 1865.
- Farjah F, Lou F, Rusch VW, et al. The quality metric prolonged length of stay misses clinically important adverse events. Ann Thorac Surg 2012;94:881-7; discussion 887-8. [Crossref] [PubMed]
- Morrison RS, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain 2003;103:303-11. [Crossref] [PubMed]
- Rivkin A, Rivkin MA. Perioperative nonopioid agents for pain control in spinal surgery. Am J Health Syst Pharm 2014;71:1845-57. [Crossref] [PubMed]
- Uquillas CA, Capogna BM, Rossy WH, et al. Postoperative pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 2016;25:1204-13. [Crossref] [PubMed]
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- Zanoli G, Strömqvist B, Jönsson B. Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine (Phila Pa 1976) 2001;26:2375-80. [Crossref] [PubMed]
- Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976) 2000;25:3130-9. [Crossref] [PubMed]
- Viscusi ER, Reynolds L, Chung F, et al. Patient-controlled transdermal fentanyl hydrochloride vs intravenous morphine pump for postoperative pain: a randomized controlled trial. JAMA 2004;291:1333-41. [Crossref] [PubMed]
- Hong D, Flood P, Diaz G. The side effects of morphine and hydromorphone patient-controlled analgesia. Anesth Analg 2008;107:1384-9. [Crossref] [PubMed]
- Goodarzi M. Comparison of epidural morphine, hydromorphone and fentanyl for postoperative pain control in children undergoing orthopaedic surgery. Paediatr Anaesth 1999;9:419-22. [Crossref] [PubMed]
- Madere Tyler C., Mendez Jennifer B., Nordmeyer Sarah T., et al. Evaluation of intravenous acetaminophen on length of stay in abdominal surgery patients. Hospital Pharmacy 2016;51:230-6. [Crossref]
- Sing DC, Barry JJ, Cheah JW, et al. Long-Acting Opioid Use Independently Predicts Perioperative Complication in Total Joint Arthroplasty. J Arthroplasty 2016;31:170-4:e1.
- Brown ST, Bowman JM, Eason FR. A comparison of patient-controlled analgesia versus traditional intramuscular analgesia in postoperative pain management. J Intraven Nurs 1993;16:333-8. [PubMed]
- Conner M, Deane D. Patterns of patient-controlled analgesia and intramuscular analgesia. Appl Nurs Res 1995;8:67-72. [Crossref] [PubMed]
- Van Boerum DH, Smith JT, Curtin MJ. A comparison of the effects of patient-controlled analgesia with intravenous opioids versus Epidural analgesia on recovery after surgery for idiopathic scoliosis. Spine (Phila Pa 1976) 2000;25:2355-7. [Crossref] [PubMed]
- Fisher CG, Belanger L, Gofton EG, et al. Prospective randomized clinical trial comparing patient-controlled intravenous analgesia with patient-controlled epidural analgesia after lumbar spinal fusion. Spine (Phila Pa 1976) 2003;28:739-43. [Crossref] [PubMed]
- Cuff DJ, O'Brien KC, Pupello DR, et al. Evaluation of factors affecting acute postoperative pain levels after arthroscopic rotator cuff repair. Arthroscopy 2016;32:1231-6. [Crossref] [PubMed]


