Streptococcus intermedius: an unusual cause of spinal epidural abscess
Introduction
Spinal epidural abscess (SEA) is a localized purulent collection between the dura mater and the spinal canal that can be fatal in up to 16% of cases (1). Devastating complications such as permanent paralysis is estimated to affect 20% of patients (2). Patients typically present with acute localized neck or back pain and fever (3). As the abscess continues to exert compression, neurological impairment might develop. Fever could be absent in almost half of patients, which contributes to a high likelihood of delayed diagnosis (1). Some patients solely present with neck or back pain, making the diagnosis challenging and potentially increasing morbidity and mortality (3). Diagnosis starts with clinical suspicion and is confirmed by MR imaging, which displays 91% sensitivity to SEA (4). Intravenous (IV) antibiotics are the mainstay treatment, whereas surgery is most frequently indicated in cases of neurological deterioration, clinical or radiographic instability, lack of response to antibiotics, and need for biopsy (1,3).
SEA accounts for 0.2 to 2 cases per 10,000 hospital admissions (5). The true incidence of SEA following a dental procedure is unknown, however, it is expected to be considerably low. In one of the largest meta-analyses on SEA, researchers found that dental abscesses were a potential source of infection in less than 1% of cases, whereas skin infections compromised 15% of cases (1). SEA is most commonly found in patients with immunodeficiency (e.g., diabetes mellitus), IV drug abusers, and in those who underwent a spinal surgery or intervention (i.e., epidural injection, or intrathecal pump placement) (1,6,7). SEA following a dental tooth extraction has been described in eight cases in the literature, one of which resulted in the patient’s death (8) and two resulted in irreversible neurological deficits (9,10). To the authors’ best knowledge, this is the first report of SEA due to Streptococcus intermedius following a root canal procedure only, without tooth extraction, in a healthy patient. This case highlights the importance of the clinical suspicion of SEA in patients presenting with lower back pain and fever following a dental procedure, even in immunocompetent patients. Although hard to achieve always, early diagnosis and treatment of SEA may prevent irreversible neurological deficits.
Case presentation
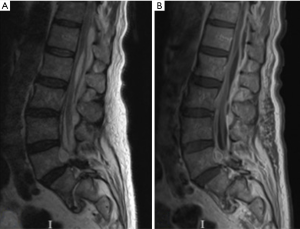
A 74-year-old man with a 7-year history of lumbar laminectomy and a baseline left foot drop was admitted to a local hospital for worsening lower back pain and inability to ambulate. Four days prior to admission, he underwent over a 2-day period, 2 root canal procedures for tooth decay and was prescribed prophylactic oral 250 mg Azithromycin after the first procedure. Lumbar magnetic resonance imaging (MRI) scans demonstrated an epidural abscess extending from L1 through L5 both ventrally and posteriorly. A broad-spectrum IV antibiotic was started and blood cultures and sensitivity were obtained and grew Streptococcus intermedius. The patient was switched to IV penicillin accordingly. In spite of appropriate coverage of his bacteremia, the patient’s back and bilateral lower extremity pain intensified, and he eventually developed urinary retention for which he required catheterization. A repeat whole spine MRI showed that the epidural abscess has extended up to the T10–T11 level (Figure 1).
The patient was transferred to our hospital on the 7th day of admission for further management. On physical examination, he was +4/5 in the lower extremities, and 0/5 in his left dorsiflexion. The rest of the exam was unremarkable; the patient denied any past or recent history of IV drug abuse. His white blood cells count was 146,500/cu mm, sedimentation rate 75 mm/h (1–20 mm/h) and C-reactive protein 7.8 mg/dL (<0.5 mg/dL). Given his lower extremity weakness and new-onset urinary retention, the patient was offered surgery. He underwent a T10 through S1 bilateral decompressive laminectomy and evacuation of the epidural abscess. Culture of pus collected during the operation was positive for Streptococcus intermedius.
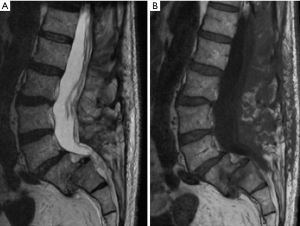
The patient’s postoperative course was uneventful as he regained baseline strength of lower extremity and bladder control. He was discharged on postoperative day 9 on IV penicillin for a 6-week course. He underwent a transthoracic and transesophageal echocardiogram that showed no evidence of endocarditis. On 3-month follow-up, MRI of the thoracolumbar spine showed resolution of the previously documented lumbar epidural abscess (Figure 2).
Literature review
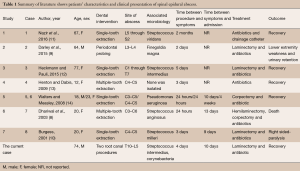
A literature review was performed to identify all articles reporting on patients developing spinal epidural infection following a dental procedure. The goal was to describe the patients’ characteristics and determine an association between individual risk factors (age, gender, immunosuppression, and a history of spinal surgery) and development of spinal epidural infection after a dental procedure. Using the MEDLINE database and the PubMed portal, we searched the following terms: (root canal OR dental procedure OR dental infection OR dental extraction OR dental abscess AND epidural infection OR epidural abscess AND english[Lang]). Human-relevant publications between 1970 and August 2016 were identified. Abstracts summaries of 1,753 articles in the search results were screened. The references of these publications were also retrieved to identify other potential studies. We excluded the articles that did not adequately describe the patients’ characteristics and the radiological findings (n=4). We also excluded articles describing only cranial infections to avoid heterogeneity (n=9). The literature review yielded 7 articles encompassing 8 cases of SEA of a potential dental origin, 5 of which were in the cervical spine, 1 in the cervicothoracic spine, and 2 in the lumbar spine (Table 1). Average (± standard deviation) age of patients was 37.63±26.69 years. Most patients were female (6:2). The majority of patients (7/8) were healthy and did not have a predisposing factor for SEA besides the dental extraction. However, 1 patient was immunocompromised (receiving methotrexate, glucocorticoids, and anti-tumor necrosis factor therapy for rheumatoid arthritis), and underwent a minimally invasive periodontal probing after which he developed lumbar SEA (case 2). None of the patients had a known concomitant infection or a history of spinal or cranial procedures. All patients presented with either neck or back pain, 75% of patients (6/8) presented with a neurological deficit (8-10,13,14), 25% of patients (2/8) presented with radiculopathy (10,14), and 1 patients (12.5%) presented with cauda equina (9). Time between tooth extraction and symptoms ranged between 24 hours and 2 months. One patient developed discitis at the same level (cases 4), and three patients developed osteomyelitis (cases 1, 5 and 6). Two patients were treated with parenteral antibiotic treatment only and 6 patients required surgical intervention after antibiotic therapy was initiated (Table 1).
Full table
Discussion
This is the first report of SEA following a root canal procedure in an immunocompetent patient. The patient’s presentation of acute localized back pain accompanied with high fevers and chills after a recent dental procedure was highly suspicious of spinal epidural infection. His blood cultures grew Streptococcus intermedius, bacteria of dental origin. Diagnosis was confirmed with the MRI scans that showed pockets of epidural abscesses in the thoracic and lumbar spine. The patient was treated with decompressive laminectomy, abscess evacuation, and IV antibiotics. Pus cultures grew the same type of bacteria. The patient made an uneventful recovery.
A hematogenous spreading of oral bacteria is known to result from both surgical and conservative dental procedures (15,16). Debelian et al. found that the incidence of bacteremia during and after endodontic therapy ranged from 31% to 54% in patients with apical periodontitis (16). Most oral microorganisms are eliminated shortly after they gain access to the blood stream, unless they find an appropriate environment to settle, such as the spinal epidural fat. The spinal epidural fat is supplied with an extensive venous plexus that provides a rich environment for bacteria to multiply and spread to other spinal levels (17). Previous studies have shown that the epidural abscesses are more common in the lumbar spine predominately because it is wider and contains more epidural fat (18). In the current patient, the epidural abscess was first documented at and adjacent to his previously operated level (performed in 2007). We suspect that his history of laminectomy with resulting scar tissue and arachnoiditis have eased the way of bacteria to reach the epidural canal and create an abscess (Figure 1A) (1,19). Darouiche et al. retrospectively reviewed data of all patients admitted to four different teaching hospitals for spinal epidural infection during an 11-year period (2). They found that the only predisposing factor in 23% of cases was an abnormality of the vertebral spine including a remote spinal surgery and degenerative disc disease, both of which were present in our patient. Other routes of infections, including lymphatic and contiguous spread, require a longer duration to be symptomatic and a concomitant infection respectively, thus are unlikely in this case.
Streptococcus intermedius is a part of Streptococcus milleri group (SMG), which are facultative oral bacteria. Whiley et al. obtained 157 strains of SMG from different infected human organs and found that 40.76% of them were isolated from dental plaques (20). This group of bacteria is notorious of invasive and resistant liver, head and neck, and brain abscesses (20,21). More importantly, they were also found to be resistant to root canal treatment, such as root canal procedure (22,23). Indeed, Narayanan et al. reviewed the articles published between 1995 and 2010 of microorganism involved in root canal pathology and found that Streptococcus milleri was one of the most common gram-positive bacteria encountered with cases of failed endodontic treatment and persistent infected canals (23). However, there was no direct correlation with Streptococcus intermedius. Due to the rarity of the bacteria, there were no studies that investigate the level of bacteremia with S. intermedius following a dental procedure. Multiple virulence factors are associated with the increased pathogenicity of Streptococcus milleri, including a polysaccharide capsule that helps penetrating the body’s defense barriers, and escaping phagocytosis (24), and hydrolytic enzymes (N-acetylmuramidase, hyaluronidase, gelatinase and collagenase) that enable the bacteria to expose and degrade extracellular matrix of connective tissues and form an abscess. Lastly, intermedilysin cytotoxic, a unique toxin to Streptococcus intermedius, can directly induce cellular apoptosis which increases its pathogenicity (25).
Eight cases of post-tooth extraction SEA were found in the literature (Table 1). The underlying assumption is this patient population is of a poor oral hygiene requiring dental extraction, which is a predisposing factor to bacteremia, compared to infection-free teeth (26). In this case, the patient had a long-standing relationship with his dentist and maintained a good oral hygiene. Moreover, poor dental hygiene has been found to predispose to brain abscesses and infective endocarditis without any dental intervention (27,28). Korfias et al. reported on a 57-year-old man who presented with neck pain, fever, and bilateral extremity weakness, and was found to have a cervical epidural abscess (29). His past medical history did not reveal any predisposing factors, such as immunodeficiency or a spinal surgery. However, the patient admitted to a dental pain 10 days prior to his presentation for which he did not seek treatment. A computerized tomography (CT) scans revealed a dental abscess, after which two teeth were extracted.
Interestingly, the literature review revealed 2 cases of spinal epidural abscess secondary to a contaminated injection or equipment to be the source of infection (Table 1, cases 5 and 6). These 2 patients underwent tooth extraction by the same dentist, contracted the same infective agent, and had an identical presentation of cervical epidural infection within 24 hours of the procedure. Additionally, the blood cultures in both cases grew microorganism that was not part of oral microflora (Pseudomonas aeruginosa). In comparison, the microorganism that was found in blood and pus cultures in the current case is a typical oral facultative bacterium.
MRI is the gold standard as it clearly outlines the location of the abscess and differentiates from other spinal lesions and pathologies (4). Empirical antimicrobial treatment should be initiated to prevent further bacterial growth, and be switched to the susceptible drug after culture and sensitivity test (30). Surgery, with or without stabilization, is reserved for patients with neurological deterioration, clinical and/or radiographic instability, need for biopsy, and lack of response to antibiotics treatment.
Conclusions
In this article, the authors present the first report of a SEA following a root canal procedure in an immunocompetent patient. Streptococcus intermedius is an unusual cause of spinal infection of dental origin. Treatment is typically medical with IV antibiotics unless the patient exhibit neurological deficits and/or instability, at which point surgery should be considered.
Acknowledgements
None.
Footnote
Conflicts of Interest: Ali Bydon is a recipient of a research grant from DePuy Spine, and serves on the clinical advisory board of MedImmune, LLC.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev 2000;23:175-204; discussion 5. [Crossref] [PubMed]
- Darouiche RO, Hamill RJ, Greenberg SB, et al. Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore) 1992;71:369-85. [Crossref] [PubMed]
- Darouiche RO. Spinal epidural abscess. N Engl J Med 2006;355:2012-20. [Crossref] [PubMed]
- Hlavin ML, Kaminski HJ, Ross JS, et al. Spinal epidural abscess: a ten-year perspective. Neurosurgery 1990;27:177-84. [Crossref] [PubMed]
- Baker AS, Ojemann RG, Swartz MN, et al. Spinal epidural abscess. N Engl J Med 1975;293:463-8. [Crossref] [PubMed]
- Knight JW, Cordingley JJ, Palazzo MG. Epidural abscess following epidural steroid and local anaesthetic injection. Anaesthesia 1997;52:576-8. [Crossref] [PubMed]
- Rubinstein E. Staphylococcus aureus bacteraemia with known sources. Int J Antimicrob Agents 2008;32 Suppl 1:S18-20. [Crossref] [PubMed]
- Dhariwal DK, Patton DW, Gregory MC. Epidural spinal abscess following dental extraction--a rare and potentially fatal complication. Br J Oral Maxillofac Surg 2003;41:56-8. [Crossref] [PubMed]
- Darley MD, Saad D, Haydoura S, et al. Spinal epidural abscess following minimally invasive dental examination in a rheumatoid arthritis patient receiving methotrexate, glucocorticoids, and anti-tumor necrosis factor therapy. J Clin Rheumatol 2015;21:52-3. [Crossref] [PubMed]
- Burgess BJ. Epidural abscess after dental extraction. Emerg Med J 2001;18:231. [Crossref] [PubMed]
- Nazir S, Lohani S, Tachamo N, et al. Low back pain after a dental procedure: a case of Streptococcus viridans vertebral osteomyelitis. BMJ Case Rep 2016.2016. [PubMed]
- Heckmann JG, Pauli SU. Epidural abscess after dental extraction. Age Ageing 2015;44:901. [Crossref] [PubMed]
- Henton JM, Dabis HS. Discitis and epidural abscess after dental extraction in a pediatric patient: a case report. Pediatr Emerg Care 2009;25:862-4. [Crossref] [PubMed]
- Walters HL, Measley R. Two cases of Pseudomonas aeruginosa epidural abscesses and cervical osteomyelitis after dental extractions. Spine (Phila Pa 1976) 2008;33:E293-6. [Crossref] [PubMed]
- Tomás I, Alvarez M, Limeres J, et al. Prevalence, duration and aetiology of bacteraemia following dental extractions. Oral Dis 2007;13:56-62. [Crossref] [PubMed]
- Debelian GJ, Olsen I, Tronstad L. Anaerobic bacteremia and fungemia in patients undergoing endodontic therapy: an overview. Ann Periodontol 1998;3:281-7. [Crossref] [PubMed]
- Tacconi L, Johnston FG, Symon L. Spinal epidural abscess--review of 10 cases. Acta Neurochir (Wien) 1996;138:520-3. [Crossref] [PubMed]
- Lanfermann H, Heindel W, Gierenz M, et al. The MR tomographic diagnosis of intra- and paraspinal abscesses. Rofo 1996;165:36-42. [Crossref] [PubMed]
- Du Pen SL, Peterson DG, Williams A, et al. Infection during chronic epidural catheterization: diagnosis and treatment. Anesthesiology 1990;73:905-9. [Crossref] [PubMed]
- Whiley RA, Fraser H, Hardie JM, et al. Phenotypic differentiation of Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus strains within the "Streptococcus milleri group". J Clin Microbiol 1990;28:1497-501. [PubMed]
- Mishra AK, Fournier PE. The role of Streptococcus intermedius in brain abscess. Eur J Clin Microbiol Infect Dis 2013;32:477-83. [Crossref] [PubMed]
- Pinheiro ET, Gomes BP, Ferraz CC, et al. Evaluation of root canal microorganisms isolated from teeth with endodontic failure and their antimicrobial susceptibility. Oral Microbiol Immunol 2003;18:100-3. [Crossref] [PubMed]
- Narayanan LL, Vaishnavi C. Endodontic microbiology. J Conserv Dent 2010;13:233-9. [Crossref] [PubMed]
- Whiley RA, Beighton D, Winstanley TG, et al. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. J Clin Microbiol 1992;30:243-4. [PubMed]
- Nagamune H, Ohnishi C, Katsuura A, et al. Intermedilysin, a novel cytotoxin specific for human cells secreted by Streptococcus intermedius UNS46 isolated from a human liver abscess. Infect Immun 1996;64:3093-100. [PubMed]
- Takai S, Kuriyama T, Yanagisawa M, et al. Incidence and bacteriology of bacteremia associated with various oral and maxillofacial surgical procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:292-8. [Crossref] [PubMed]
- Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc 2009;140:1238-44. [Crossref] [PubMed]
- Azenha MR, Homsi G, Garcia IR Jr. Multiple brain abscess from dental origin: case report and literature review. Oral Maxillofac Surg 2012;16:393-7. [Crossref] [PubMed]
- Korfias S, Alexiou GA, Vlachakis E, et al. Cervical epidural abscess of odontogenic origin. Neurol Sci 2015;36:1017-8. [Crossref] [PubMed]
- Mackenzie AR, Laing RB, Smith CC, et al. Spinal epidural abscess: the importance of early diagnosis and treatment. J Neurol Neurosurg Psychiatry 1998;65:209-12. [Crossref] [PubMed]


