Relationship between depression and clinical outcome following anterior cervical discectomy and fusion
Introduction
Anterior cervical discectomy and fusion (ACDF) is a commonly performed treatment for patients with symptomatic instability of the cervical spine (1,2). There has been consistent long-term evidence supporting excellent outcomes and significant improvements in quality of life in appropriately selected patients undergoing ACDF surgery (3-9). In the past several decades, nationwide epidemiological data has suggested a rapidly increasing number of ACDF procedures performed on increasingly elderly patients (10-12). As such, there has been increasing emphasis on identifying preoperative risk factors to maximize success of surgery, improve outcomes, and contain costs.
Factors including sex, age, smoking status, segmental kyphosis and preoperative pain and disability levels are preoperative baseline characteristics that have already been shown to influence outcomes after ACDF (13,14). Gruskay et al. analyzed 2,164 patients from the National Surgical Quality Improvement Project (NSQIP) database and demonstrated that elderly age, preoperative anemia, male sex, and extended surgery time were predictors of major complications and worse outcomes after ACDF (15). Other predictors of 30-day outcomes following ACDF have also been explored, including American Society of Anesthesiologists (ASA) scores, the frailty index, and insulin dependence (16-18). More recently, there have been increasing data supporting the role of preoperative psychological states affecting operative clinical outcomes, given that conditions such as depression are often prevalent in patients with chronic pain (19,20). In the context of lumbar spine surgery, a significant negative correlation has been reported by multiple studies between preoperative depression and postoperative clinical outcomes. Pakarinen et al. investigated 102 patients with lumbar spinal stenosis who underwent decompression surgery; at 5-year follow-up, preoperative depression was associated with poorer ODI scores (21), with similar trends reported by others (22-27).
The association between depression and neck pain is less clear and not well documented. Relatively few studies have explored the association between preoperative psychological states such as depression with clinical outcomes following anterior or posterior cervical surgery (28,29). One recent study (30) retrospectively analyzed 106 patients who underwent ACDF but did not find a statistically significant association between preoperative depression and postoperative health outcome. In the present study, we sought to assess the impact of preoperative depression on patient reported clinical outcomes following ACDF surgery based on the experience at our institution.
Methods
Study sample
Following institutional review board approval, a retrospective review of clinical and operative notes was performed to identify all neurosurgical patients undergoing an ACDF at a single academic institution between March 2012 and March 2014. Patients were included if they were older than 18 years undergoing ACDF for treatment of cervical spondylosis with myelopathy and/or radiculopathy. Patients undergoing ACDF following trauma, tumor resection, or primary spinal infections were not included in this study. Patients were identified as having depression if this diagnosis was mentioned in their medical record in their problem list or in their patient notes. Patients with other mood disorders were excluded. Patients were included irrespective of whether they were receiving treatment for their depression.
Covariates
Patient data such as age, sex, comorbidities, diagnosis, presenting symptoms, and Nurick scores were collected from clinical notes. Comorbidities assessed included coronary artery disease (CAD), diabetes, osteoporosis, obesity, smoking, chronic obstructive pulmonary disease (COPD) and hypertension. Diagnoses included spinal stenosis, adjacent segment disease, and degenerative disc disease (DDD). Presenting symptoms included neck pain, headaches, radiculopathy, myelopathy, motor deficit, sensory deficit, and bowel/bladder dysfunction. The primary outcome assessed was postoperative Nurick score, which was obtained from clinic notes at last available follow-up for each patient. The Nurick score is classification system that is used to assess functional status in patients with myelopathy. The score ranges from 0 to 5, with higher scores corresponding to worse dysfunction (31). The scoring system is based on a person’s ability to ambulate, with grade 0 being only radiculopathy to grade 5 being bed ridden.
Statistical analysis
Patient demographics are described with summary statistics. Patients with preoperative diagnosis of depression were compared to those without depression (Table 1). Univariate linear regression was performed to examine the relationship between all predictor variables and postoperative Nurick score. A multivariate linear regression model was selected, based on the lowest AIC score, to assess the relationship between depression and postop Nurick score, including all predictor variables as candidates for inclusion. We confirmed that there was not excessive collinearity in our model. Statistical significance was set at P≤0.05.

Full table
Results
We identified 93 patients undergoing ACDF, of whom 16 (17.2%) had a formal diagnosis of depression compared to 77 (82.8%) without depression. The groups did not significantly differ in the sex ratio. The mean age of the two groups were also comparable (52.8 vs. 54.9 years, P=0.499).
The two groups also did not differ in the prevalence of many comorbidities, including CAD (P=0.316), diabetes mellitus (P=0.368), osteoporosis (P=1.00), obesity (P=0.747), COPD (P=1.00), and hypertension (P=0.48). In terms of diagnoses, there were similar proportions of patients with spinal stenosis (P=0.901), adjacent segment disease (P=0.407) and DDD (P=0.754).
In terms of presenting symptoms, there was no significant difference between patients with depression versus those without depression in terms of neck pain (P=0.957), headaches (P=0.583), radiculopathy (P=0.796), myelopathy (P=0.443), motor deficit (P=0.393), sensory deficit (P=0.366), or bowel/bladder dysfunction (P=0.081). Preoperative Nurick score was similar between the two groups (P=0.084), but patients with depression tended to have discectomy and fusion procedure involving more levels (P=0.000).
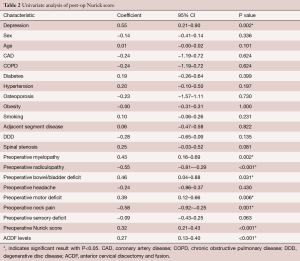
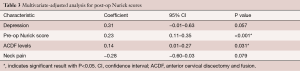
Univariate analysis indicated that depression, preoperative motor deficit, preoperative bowel/bladder deficit, preoperative myelopathy, number of ACDF levels and preoperative Nurick score were significantly associated with a higher post-operative Nurick score (Table 2). The presence of preoperative neck pain and radiculopathy were significantly associated with lower post-operative Nurick scores. After multivariate adjusted analysis, there was a trend towards patients with depression having higher post-operative Nurick scores compared to those without depression (coefficient =0.31, 95% CI: −0.01–0.63, P=0.057) (Table 3). Patients that had higher pre-operative Nurick scores and those receiving increased levels of ACDF had statistically significantly higher post-operative Nurick scores, but the effect size was less than for depression.
Full table
Full table
Discussion
Psychiatric conditions such as mood disorders represent a significant burden to society, with over 50% prevalence of depression in surgical candidates for chronic neck or low back pain (22,23,26,32). Several studies have suggested that depression may be associated with worse improvement in clinical outcome following lumbar spine surgery. Whilst the precise mechanism for this association is not clear, it has been suggested that people with depression tend to be less motivated to recover, less likely to participate in rehabilitation, and more likely to be dissatisfied with medical services (21,33). Depression has been shown to be linked with poor postoperative return to work status amongst a cohort of worker’s compensation patients undergoing lumbar fusion (34). However, the impact of depression on clinical outcomes following ACDF surgery has not been well studied. In the present analysis, we demonstrated a trend towards worse outcomes in patients with depression on multivariate analysis.
Alvin et al. (30) also investigated retrospective patients who underwent ACDF and the influence of preoperative depression on clinical outcomes. The authors found that although not statistically significant, those with greater degrees of depression trended towards lower improvements in postoperative quality of life outcome scores compared to patients with less depression. As such, these studies together suggest that it may be important to consider depression when identifying patients who would be likely to respond better from an ACDF surgery.
Few studies have directly compared the influence of preoperative depression on clinical outcomes following anterior or posterior cervical spinal fusion (35,36). However, similar trends were observed compared to the studies that focused on the lumbar spine, suggesting that the influence of depression on clinical improvement is likely to be independent of the precise spinal procedure. Adogwa et al. (26) retrospectively analysed 53 patients undergoing revision surgery for symptomatic same-level recurrent stenosis. Although there was an overall improvement in all outcome measures at two-year follow-up, patients with increased preoperative depression were less satisfied. Pakarinen et al. (21) performed a prospective observational study of 102 lumbar spine stenosis patients who underwent depression surgery. At 5-year follow-up, patients with high depressive burden were associated with significantly poorer outcomes when assessed using the Oswestry Disability Index (ODI). These results were consistent with those from a systematic review which concluded that preoperative depression is a likely prognostic factor of postoperative outcome (27). Preoperative depression in patients undergoing ACDF and other forms of spinal surgery may also have social and economic implications, with one study demonstrating that preoperative depression was an independent predictor of delayed time to return to work postoperatively (37).
The association between preoperative depression and poor clinical outcomes post ACDF surgery may be explained by altered motivation state and cognitive impairments associated with depression including low motivation for activity (38). Others have suggested that the pathophysiology of depression may involve persistent low-grade inflammatory activity (39-41), which may influence the outcomes of rehabilitation following spinal surgery. Whilst conclusions regarding causal relationships cannot be made based due to the retrospective nature of the present study, the available results collectively suggest that it may be useful to identify and stratify patients according to preoperative depression burden. It is currently unknown whether treatment of depression before surgery with either psychotherapy or antidepressant medication may improve outcomes after lumbar surgery, and this question remains to be addressed by future studies (37).
In our study, we also found that higher preoperative Nurick scores statistically significantly predicted a higher postoperative Nurick score on multivariate analysis. Essentially, patients that had worse functional ability pre-operative were more likely to have worse functional ability post-operatively. Furthermore, the number of ACDF levels was also predictive of worse post-operative Nurick scores. This could be because patients that have a larger surgery have worse pathology or because a larger surgery is associated with greater post-op morbidity.
The results of the present study are constrained by several limitations. Firstly, only one postoperative clinical score outcome was investigated in the present study. The Nurick score is a scale used to assess functional disability in patients with cervical spondylotic myelopathy, with a greater emphasis on gait function. Other scores of interest would include EQ-5D quality of life scores, visual analog scale, and ODI. Our study is also limited by the follow-up duration, with a mean follow-up of 7 months in the no-depression group versus 10-month in the depression group. Ideally, outcomes of patients followed-up for greater than 2 years should be assessed prospectively. Thirdly, the retrospective nature of this study means that there are inherent limitations in the accuracy and completion of the data. Future prospective studies of greater sample size are required to confirm the trends observed in the present study.
Conclusions
Patients with baseline depression had poorer functional Nurick scores after ACDF surgery compared to patients without depression. Further research should be performed to investigate the relationship between depression and post-operative outcomes and on whether treating depression can improve post-operative outcomes in the short and longer-term.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Johns Hopkins University School of Medicine (No. NA_00038491) and written informed consent was obtained from all patients.
References
- Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery 2005;57:753-8; discussion -8.
- Shamji MF, Cook C, Tackett S, et al. Impact of preoperative neurological status on perioperative morbidity associated with anterior and posterior cervical fusion. J Neurosurg Spine 2008;9:10-6. [Crossref] [PubMed]
- Carreon LY, Anderson PA, Traynelis VC, et al. Cost-effectiveness of single-level anterior cervical discectomy and fusion five years after surgery. Spine (Phila Pa 1976) 2013;38:471-5. [Crossref] [PubMed]
- Parker SL, Godil SS, Shau DN, et al. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine 2013;18:154-60. [Crossref] [PubMed]
- Di Capua J, Somani S, Kim JS, et al. Analysis of Risk Factors for Major Complications Following Elective Posterior Lumbar Fusion. Spine (Phila Pa 1976) 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Maharaj MM, Mobbs RJ, Hogan J, et al. Anterior cervical disc arthroplasty (ACDA) versus anterior cervical discectomy and fusion (ACDF): a systematic review and meta-analysis. J Spine Surg 2015;1:72-85. [PubMed]
- Maharaj MM, Phan K, Mobbs RJ. Anterior cervical discectomy and fusion (ACDF) autograft versus graft substitutes: what do patients prefer?—A clinical study. J Spine Surg 2016;2:105-10. [Crossref] [PubMed]
- Nambiar M, Phan K, Cunningham JE, et al. Locking stand-alone cages versus anterior plate constructs in single-level fusion for degenerative cervical disease: a systematic review and meta-analysis. Eur Spine J 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Di Capua J, Somani S, Kim JS, et al. Predictors for Patient Discharge Destination Following Elective Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Oglesby M, Fineberg SJ, Patel AA, et al. Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine (Phila Pa 1976) 2013;38:1226-32. [Crossref] [PubMed]
- Marawar S, Girardi FP, Sama AA, et al. National trends in anterior cervical fusion procedures. Spine (Phila Pa 1976) 2010;35:1454-9. [Crossref] [PubMed]
- Cowan JA Jr, Dimick JB, Wainess R, et al. Changes in the utilization of spinal fusion in the United States. Neurosurgery 2006;59:15-20; discussion 15-20. [Crossref] [PubMed]
- Peolsson A, Peolsson M. Predictive factors for long-term outcome of anterior cervical decompression and fusion: a multivariate data analysis. Eur Spine J 2008;17:406-14. [Crossref] [PubMed]
- Peolsson A, Hedlund R, Vavruch L, et al. Predictive factors for the outcome of anterior cervical decompression and fusion. Eur Spine J 2003;12:274-80. [PubMed]
- Gruskay JA, Fu M, Basques BA, et al. Factors Affecting Length of Stay and Complications After Elective Anterior Cervical Discectomy and Fusion: A Study of 2164 Patients From The American College of Surgeons National Surgical Quality Improvement Project Database (ACS NSQIP). Clin Spine Surg 2016;29:E34-42. [PubMed]
- Phan K, Kim JS, Lee N, et al. Impact of Insulin Dependence on Perioperative Outcomes Following Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:456-64. [Crossref] [PubMed]
- Phan K, Kim JS, Lee NJ, et al. Relationship Between ASA Scores and 30-Day Readmissions in Patients Undergoing Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:85-91. [Crossref] [PubMed]
- Shin JI, Kothari P, Phan K, et al. Frailty Index as a Predictor of Adverse Postoperative Outcomes in Patients Undergoing Cervical Spinal Fusion. Spine (Phila Pa 1976) 2017;42:304-10. [Crossref] [PubMed]
- American Society of Anesthesiologists Task Force on Chronic Pain M. American Society of Regional A, Pain M. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology 2010;112:810-33. [Crossref] [PubMed]
- Miller JA, Derakhshan A, Lubelski D, et al. The impact of preoperative depression on quality of life outcomes after lumbar surgery. Spine J 2015;15:58-64. [Crossref] [PubMed]
- Pakarinen M, Vanhanen S, Sinikallio S, et al. Depressive burden is associated with a poorer surgical outcome among lumbar spinal stenosis patients: a 5-year follow-up study. Spine J 2014;14:2392-6. [Crossref] [PubMed]
- Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine (Phila Pa 1976) 2000;25:2616-21. [Crossref] [PubMed]
- LaCaille RA, DeBerard MS, Masters KS, et al. Presurgical biopsychosocial factors predict multidimensional patient: outcomes of interbody cage lumbar fusion. Spine J 2005;5:71-8. [Crossref] [PubMed]
- Vaccaro AR, Ring D, Scuderi G, et al. Predictors of outcome in patients with chronic back pain and low-grade spondylolisthesis. Spine (Phila Pa 1976) 1997;22:2030-4; discussion 2035. [Crossref] [PubMed]
- Aalto TJ, Malmivaara A, Kovacs F, et al. Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine (Phila Pa 1976) 2006;31:E648-63. [Crossref] [PubMed]
- Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung depression scale predicts patient satisfaction independent of the extent of improvement after revision lumbar surgery. Spine J 2013;13:501-6. [Crossref] [PubMed]
- McKillop AB, Carroll LJ, Battie MC. Depression as a prognostic factor of lumbar spinal stenosis: a systematic review. Spine J 2014;14:837-46. [Crossref] [PubMed]
- Stoffman MR, Roberts MS, King JT Jr. Cervical spondylotic myelopathy, depression, and anxiety: a cohort analysis of 89 patients. Neurosurgery 2005;57:307-13; discussion 307-13. [Crossref] [PubMed]
- He J, Xiong W, Li F, et al. Depression influences pain and function after cervical disc arthroplasty. J Neurosurg Sci 2017;61:39-45. [PubMed]
- Alvin MD, Miller JA, Lubelski D, et al. The Impact of Preoperative Depression and Health State on Quality-of-Life Outcomes after Anterior Cervical Diskectomy and Fusion. Global Spine J 2016;6:306-13. [Crossref] [PubMed]
- Nurick S. The natural history and the results of surgical treatment of the spinal cord disorder associated with cervical spondylosis. Brain 1972;95:101-8. [Crossref] [PubMed]
- Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung Depression Scale predicts outcome after revision lumbar surgery for adjacent segment disease, recurrent stenosis, and pseudarthrosis. Spine J 2012;12:179-85. [Crossref] [PubMed]
- Vialle E, de Oliveira Pinto BM, Vialle LR, et al. Evaluation of psychosomatic distress and its influence in the outcomes of lumbar fusion procedures for degenerative disorders of the spine. Eur J Orthop Surg Traumatol 2015;25 Suppl 1:S25-8. [Crossref] [PubMed]
- Anderson JT, Haas AR, Percy R, et al. Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers' compensation subjects. Spine (Phila Pa 1976) 2015;40:748-56. [Crossref] [PubMed]
- Goldberg EJ, Singh K, Van U, et al. Comparing outcomes of anterior cervical discectomy and fusion in workman's versus non-workman's compensation population. Spine J 2002;2:408-14. [Crossref] [PubMed]
- George SZ, Fritz JM, Erhard RE. A comparison of fear-avoidance beliefs in patients with lumbar spine pain and cervical spine pain. Spine (Phila Pa 1976) 2001;26:2139-45. [Crossref] [PubMed]
- Parker SL, Godil SS, Zuckerman SL, et al. Extent of preoperative depression is associated with return to work after lumbar fusion for spondylolisthesis. World Neurosurg 2015;83:608-13. [Crossref] [PubMed]
- Sinikallio S, Aalto T, Airaksinen O, et al. Depression is associated with a poorer outcome of lumbar spinal stenosis surgery: a two-year prospective follow-up study. Spine (Phila Pa 1976) 2011;36:677-82. [Crossref] [PubMed]
- Dantzer R, O'Connor JC, Freund GG, et al. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 2008;9:46-56. [Crossref] [PubMed]
- Pace TW, Hu F, Miller AH. Cytokine-effects on glucocorticoid receptor function: relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav Immun 2007;21:9-19. [Crossref] [PubMed]
- Miller GE, Rohleder N, Cole SW. Chronic interpersonal stress predicts activation of pro- and anti-inflammatory signaling pathways 6 months later. Psychosom Med 2009;71:57-62. [Crossref] [PubMed]


