Solitary vertebral metastasis of primary clear cell carcinoma of the liver: a case report and review of literature
Introduction
Solitary metastasis of any malignancy poses a clinical dilemma to the surgeon who is forced to decide whether a curative resection with clear margins should be attempted at the metastatic focus, or to resort to palliative control of the tumour using non-surgical modalities, or both. The spine is the most common site for osseous metastasis from systemic neoplasia from the lung, breast, prostate, kidney and thyroid (1,2). Based on existing literature, several forms of isolated metastasis to the spine from these primaries have been described. However, no reports of isolated metastasis from primary clear cell carcinoma of liver (PCCCL) have been documented. We present a unique case of such a patient who in addition had recurrence following primary management and poor outcome, though the available literature describes favourable prognosis for this type of tumour.
Case presentation
A 71-year-old man presented with low back pain for 2 months in March 2015. Although the pain was worse with movement of the spine, it was constant in nature with substantial pain felt at rest and in the night. Due to the pain, he was only able to tolerate 5 minutes of slow ambulation for which he had to rest either by sitting or lying down. This was associated with bilateral anterior thigh pain and lower limb numbness (left > right). He also complained of progressive weakness of his lower limbs over 2 weeks prior to the presentation. He did not have any abnormal urinary or bowel symptoms.
On examination, there was midline tenderness at the mid-lumbar spine associated with paravertebral muscle spasms. Range of motion of the lumbar spine was severely limited due to low back pain. Neurological examination of the lower limb revealed weakness in both knee extensions (grade 4). His left knee jerk was hyporeflexic but his right knee jerk and both ankle jerks were normal. Femoral nerve stretch test and straight leg raise tests were unremarkable.
Plain X-rays of the lumbar spine did not show any obvious bony lesions. His serum tumour markers including alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA), CA125, beta-HCG and prostate-specific antigen (PSA) were not elevated. Other inflammatory markers including total white count, ESR and CRP levels were unremarkable. Baseline workup for his liver and kidney function was normal with laboratory tests showing normal levels of serum albumin, bilirubin (total and conjugated), aspartate transaminase (AST), alkaline phosphatase (ALP), prothrombin time (PT) and creatinine. Full body bone scan showed an isolated focus of increased radioactive tracer uptake at L3 vertebra. This was confirmed by whole body positron emission tomography (PET) scan which showed a fluorodeoxyglucose (FDG) avid lytic lesion at the L3 vertebra associated with a soft tissue mass. Again, no other FDG avid lesions could be seen elsewhere. Therefore, a presumptive diagnosis of vertebral metastasis was made and staging of the tumour was subsequently performed.
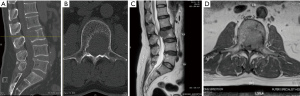
Computed tomography (CT) of the lumbar spine, thorax, abdomen and pelvis, as well as magnetic resonance imaging (MRI) of the whole spine confirmed bony destruction of L3 vertebral body and left pedicle (Figure 1A-D). On the MRI, a soft tissue mass (hypo-intense on both T1 and T2, hyperintense on STIR image) invading into the spinal canal resulted in severe left lateral recess and central canal stenosis. In addition, MRI also revealed encroachment of the tumour into the left L2/3 and L3/4 neural foramen. Triphasic CT of liver showed a 3.4 cm flash enhancing nodule in the segment 2/3 of the liver with background cirrhotic changes suggesting possibility of hepatoma. Surprisingly, this lesion was not picked by PET scan which may be due to the flash enhancing nature and background cirrhotic changes.
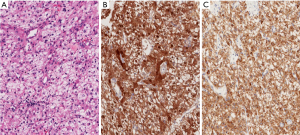
In view of the patient’s neurological deterioration, he underwent urgent angioembolisation followed by biopsy and bilateral decompression laminotomy of L3. Microscopic examination of the vertebral body biopsy showed tumour tissue composed of cells arranged in trabeculae and solid sheets. The cells had central, moderately pleomorphic nuclei and abundant clear cytoplasm (Figure 2A). Immunohistochemistry revealed strong diffuse immunostaining for arginase-1 and HepPar1, focal positivity for glypican-3 and negativity for CD10, Pax8 and vimentin (Figure 2B,C). These findings were consistent with those of a metastatic hepatocellular carcinoma with clear cell features.
Two weeks following the surgery, the patient developed severe low back pain causing him to be wheelchair bound. Emergency CT scan and MRI scan of the lumbar spine showed further collapse of the L3 vertebra with possible hematoma occupying central spinal canal. His spinal instability neoplastic score (SINS) and Tokuhashi scores were 9 and 10 respectively. Following a multidisciplinary tumour board discussion, it was decided to treat this patient with a curative intent which involves radical excision of the tumour and reconstruction and further treatment of the primary with trans arterial chemo embolisation (TACE) for the hepatic nodule.
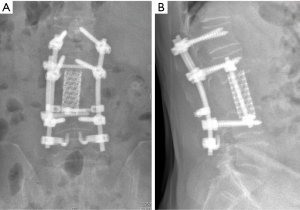
The patient then underwent preoperative embolization, followed by a single stage combined posterior and anterior approach vertebrectomy of L3. Reconstruction was performed using a mesh cage packed with demineralized bone matrix (DBM). Instrumentation was performed posteriorly from L1 to L4 and laterally from L2 to L4. Post-operatively, patient had an uneventful recovery. One month after the index surgery, he underwent radiotherapy (20 Gy in 5 daily fractions over one week) to the L3 with margins. The hepatic nodule was also treated by TACE using 75 mg of doxorubicin/lipiodol assessed over the left hepatic artery and inferior branch of the right hepatic artery. No separate biopsy was done from the liver as the biopsy from spine lesion confirmed to be metastatic clear cell carcinoma and no other lesion could be identified elsewhere. After this procedure, the patient continued to show improvement in his symptoms.
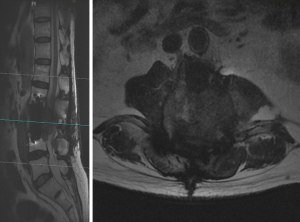
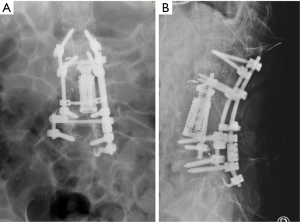
At 6 months after his second spine surgery (Figure 3), his back pain had resolved completely and his lower limbs had full power bilaterally. He was able to ambulate independently for 1km without any symptoms. However, the patient developed rapidly progressing lower limb weakness predominantly on the left side at 9 months post operatively. Examination revealed profound weakness (grade 3) in L2, L3, L4 myotomes on the left side with associated sensory deficit. Repeat MRI showed spinal tumour recurrence with obliteration of the neuroforamen from L2 to L4 and invasion into the psoas and paraspinal muscles (Figure 4). In addition, CT Thorax-abdomen-pelvis revealed a lytic lesion in the right 7th rib which was highly suggestive of metastasis.
The patient underwent a 2-stage palliative surgery spaced 1 week apart to firstly debulk the tumour with exchange of intervertebral cage through the previous lateral approach, followed by extension of posterior instrumentation caudally to L5 with pedicle hook construct (Figure 5) as it was felt that this extension would add further stability to the existing construct post debulking. Histopathology of the resected tumour again confirmed metastatic clear cell carcinoma. Postoperatively, patient received another 10 fractions of radiotherapy (20 Gy), and was started on sorafenib. His last follow-up at 1 year after the latest operation and chemotherapy showed that he had no recurrence of back pain and was able to perform his ADL independently. Despite the fact that he had sensory improvement in his left lower limb, his weakness persisted (grade 4).
Discussion
PCCCL is a rare type of hepatocellular carcinoma with an incidence of 7.5% to 12.5% amongst all liver cancer cases (3,4). Its microscopic picture is comparable to other more common clear cell cancer origins (kidney, ovarian or adrenal) and hence making its diagnosis challenging (3). Histopathologically, clear cell carcinomas can be identified based on the presence of moderate to marked cytoplasmic accumulation of glycogen and/or macro- and microvascular intracytoplasmic fat droplets which dissolve during hematoxylin-eosin staining. This dissolution leaves behind a clear cytoplasm and hence the terminology “clear cell carcinoma”.
For this group of cancers, good prognosis and improved survival is usually observed with the increasing proportion of clear cells (5,6). Compared with other histological diagnosis of HCC, PCCCL is a lower grade malignancy with good differentiation and slower growth process. In addition, the tumour tends to be more limited with capsule formation and hence is more amenable to resection (3). Limited previous studies restrict our understanding of this condition substantially especially with regard to the metastasizing ability of PCCCL. No report was found pertaining to isolated metastasis of PCCCL to the spine. In addition, no literature could be found on the treatment modality of management of metastasis from PCCCL. Ji et al. described 12 cases of lymph node metastasis in his series of 64 patients with PCCCL (3) while another larger series of 214 patients (7) by Li et al. did not report any extra hepatic metastasis. In view of these findings, it appears that surgical approach at curative resection would seem to be acceptable option for this patient. However, this was not true in our patient who had a tumour recurrence despite macroscopic clearance of metastatic spine tumour supplemented with adjuvant chemotherapy and radiotherapy.
Advancing technology allows the ability to diagnose the proliferating cancerous cells at a site away from the primary foci early and leads to what many term as “isolated metastasis”. The dilemma therefore lies in whether these cancerous deposits should be treated using a curative intent or a palliative approach. Factors that influence these decisions include patient condition, the behaviour of the cancer and its response to various treatment modalities, availability and feasibility of both surgical and medical treatments as well as patient expectations.
When feasible, complete resection of the tumour is generally a big undertaking as it challenges the surgeon to not only remove the entire tumour en bloc without injuring adjacent vital neurovascular structures, but also to reconstruct the spine for immediate and long-term stability. In terms of surgical resection techniques, intralesional curettage using posterolateral or extracavitary approaches were commonly employed in the past and had high incidence of local recurrences ranging from 20% to 50% (8). En bloc resections which aimed at complete tumour removal have been subsequently developed to address these concerns. Stener in 1980, described for the first time, a technique of en bloc spondylectomy through a posterior approach for osteosarcoma arising from seventh thoracic vertebra (9). This concept of treating primary tumours with en bloc spondylectomy was extended to the treatment of solitary vertebral metastasis of specific tumour types by Tomita et al. (10-12) who described a technique of ventral vertebrectomy following a dorsal en bloc resection after transpedicular osteotomy. With regards to the outcomes, Sundaresan et al. showed that only 17% of the 80 patients with solitary vertebral metastasis (breast, kidney, sarcoma, GI tract, liver, prostate, miscellaneous) who underwent en bloc resection experienced local recurrence with a median survival time of >30 months and 20% surviving >5 years. This is in contrast to 32% recurrence rate in those cases treated with gross resection of tumour (8). Another study of 12 patients with solitary spine metastasis showed that the risk of recurrence is higher after en bloc spondylectomy if there is paraspinal extension and recommends that this technique should only be limited to tumours which are confined to the bony margins of vertebra only (13). A series of 12 patients reported no local recurrence after en bloc resection with dorsoventral reconstruction (14). Also, another series of 20 patients after total en bloc spondylectomy reported no local recurrences at an average follow up of 13 months (10).
The technique of total en bloc spondylectomy (TES) and circumspinal decompression as described by Tomita et al. includes two steps: (I) en bloc laminectomy with posterior spinal instrumentation for stabilization; and (II) en bloc corpectomy and reconstruction using vertebral prosthesis (11). The following criteria are vital in the careful selection of patients for en bloc spondylectomy (14): (I) no underlying tumor type, which is considered to be a systemic disease; (II) tumor types that are known to be biologically favorable and to have a prolonged course (e.g., renal cell or breast carcinoma); (III) radical treatment of the original/primary tumor; (IV) long period between treatment of primary tumor and diagnosis of solitary metastatic disease; and (V) verification of isolated/solitary metastatic disease in CT scans, bone scan and/or PET. Although our patient with PCCCL met the mentioned criteria above and was successfully treated following the mentioned principles above, recurrence occurred at 9 months. The reason for recurrence in our patient could be due to poorly understood metastatic features of clear cell carcinoma of liver. Thus, the treatment results may still be substantially dependent on histological types. Sundaresan et al. in his series of 80 patients with solitary vertebral metastasis, reported significant improvement of pain in 95% of the patients, for which 76% having complete pain relief (8). Similarly, our patient had excellent pain relief and good postoperative outcome following surgical extirpation of tumour and radiotherapy up to 9 months post-operatively.
The management of recurrent spinal tumours both primary and metastatic is not clear as all available scientific evidence is based on some case reports. This is further compounded by the deranged anatomy, presence of implants from previous surgery, difficult radiological assessment of extent because of metal artifacts, extensive intra/paraspinal scarring due to surgery and radiotherapy, and lastly, topographic vicinity of major vessels and spinal cord. All these lead to surgical management of recurrent spinal tumours difficult. As described by Boriani et al., local recurrence is the worst complication in the management of spine tumours because this significantly affects quality of life and prognosis (15,16). Multilevel en bloc spondylectomy up to 4 levels have been described with good functional outcome and low recurrence rates for primary malignant and benign aggressive tumours and recurrent tumours of these. However, the long-term outcome is still not known. In the context of an isolated metastasis, a dilemma always exists—whether to treat with a curative or palliative intent. Nevertheless, it remains prudent to emphasize that treatment strategies should always consider the likely prognosis of the patient (17) to ensure that the pros outweigh the cons and the best possible quality of life can be achieved for the patient (18).
The key features of this case report include the first time presentation of PCCCL with spine metastasis which has not been reported before and aggressive nature of metastatic lesion with recurrence, although the literature quotes good prognosis for this histological type of primary.
Conclusions
PCCCL is a rare type of hepatocellular carcinoma which can present as “solitary metastasis” to the spine. Although the literature appears to suggest a good prognosis for this histological type, this case did not have a good outcome. In addition to providing information for the management of similar cases in the future, this case report highlights that every patient has to be managed on a case-by-case basis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Hatrick NC, Lucas JD, Timothy AR, et al. The surgical treatment of metastatic disease of the spine. Radiother Oncol 2000;56:335-9. [Crossref] [PubMed]
- Jacobs WB, Perrin RG. Evaluation and treatment of spinal metastases: an overview. Neurosurg Focus 2001;11:e10. [Crossref] [PubMed]
- Ji SP, Li Q, Dong H. Therapy and prognostic features of primary clear cell carcinoma of the liver. World J Gastroenterol 2010;16:764-9. [Crossref] [PubMed]
- Takahashi A, Saito H, Kanno Y, et al. Case of clear-cell hepatocellular carcinoma that developed in the normal liver of a middle-aged woman. World J Gastroenterol 2008;14:129-31. [Crossref] [PubMed]
- Lai CL, Wu PC, Lam KC, et al. Histologic prognostic indicators in hepatocellular carcinoma. Cancer 1979;44:1677-83. [Crossref] [PubMed]
- Liu JH, Tsai HL, Hsu SM, et al. Clear cell and non-clear cell hepatocellular carcinoma: a case report and literature review. Kaohsiung J Med Sci 2004;20:78-82. [Crossref] [PubMed]
- Li T, Fan J, Qin LX, et al. Risk Factors, Prognosis, and Management of Early and Late Intrahepatic Recurrence After Resection of Primary Clear Cell Carcinoma of the Liver. Ann Surg Oncol 2011;18:1955-63. [Crossref] [PubMed]
- Sundaresan N, Rothman A, Manhart K, et al. Surgery for solitary metastases of the spine: rationale and results of treatment. Spine 2002;27:1802-06. [Crossref] [PubMed]
- Stener B. Complete removal of vertebrae for extirpation of tumors. A 20-year experience. Clin Orthop Relat Res 1989.72-82. [PubMed]
- Tomita K, Kawahara N, Baba H, et al. Total en bloc spondylectomy for solitary spinal metastases. Int Orthop 1994;18:291-8. [Crossref] [PubMed]
- Tomita K, Toribatake Y, Kawahara N, et al. Total en bloc spondylectomy and circumspinal decompression for solitary spinal metastasis. Paraplegia 1994;32:36-46. [Crossref] [PubMed]
- Tomita K, Kawahara N, Kobayashi T, et al. Surgical strategy for spinal metastases. Spine 2001;26:298-306. [Crossref] [PubMed]
- Sakaura H, Hosono N, Mukai Y, et al. Outcome of total en bloc spondylectomy for solitary metastasis of the thoracolumbar spine. J Spinal Disord Tech 2004;17:297-300. [Crossref] [PubMed]
- Melcher I, Disch AC, Klostermann CK, et al. Primary malignant bone tumours and solitary metastases of the thoracolumbar spine: results by management with total en bloc spondylectomy. Eur Spine J 2007;16:1193-202. [Crossref] [PubMed]
- Boriani S, Bandiera S, Donthineni R, et al. Morbidity of en bloc resections in the spine. Eur Spine J 2010;19:231-41. [Crossref] [PubMed]
- Druschel C, Disch AC, Melcher I, et al. Surgical management of recurrent thoracolumbar spinal sarcoma with 4-level total en bloc spondylectomy: description of technique and report of two cases. Eur Spine J 2012;21:1-9. [Crossref] [PubMed]
- Tokuhashi Y, Matsuzaki H, Oda H, et al. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 2005;30:2186-91. [Crossref] [PubMed]
- Quan GM, Vital JM, Aurouer N, et al. Surgery improves pain, function and quality of life in patients with spinal metastases: a prospective study on 118 patients. Eur Spine J 2011;20:1970-8. [Crossref] [PubMed]


