Minimally invasive endoscopic spinal cord untethering: case report
Introduction
Lipomyelomeningocele is a closed neural tube defect in which a subcutaneous lipoma extends through a defect in the fascia and attaches to an elongated and tethered spinal cord (1,2). Loss of neurologic function can occur over time and is believed to be secondary to increased stretch on the spinal cord due to patient growth. The timing of surgery is an area of debate, and disease progression can lead to irreversible nerve damage and bowel and bladder incontinence (3). The standard surgical approach is to partially resect the lipoma down to its neural attachment, section the filum terminale, and create a dural expansion graft to prevent future tethering. The complications inherent to this approach include spinal fluid leak, nerve damage, worsened bowel and bladder dysfunction, and re-tethering (4,5). Here we describe a minimally invasive endoscopic-assisted approach to untethering the spinal cord that illustrates several technical advantages to utilizing endoscopic visualization in cord untethering.
Case presentation
History and presentation
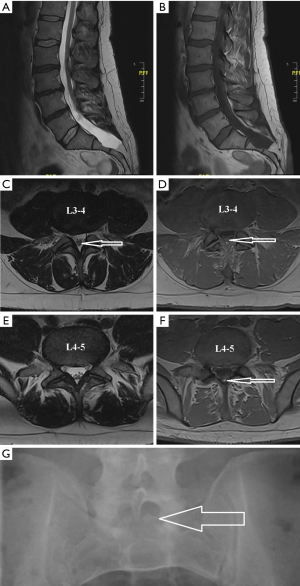
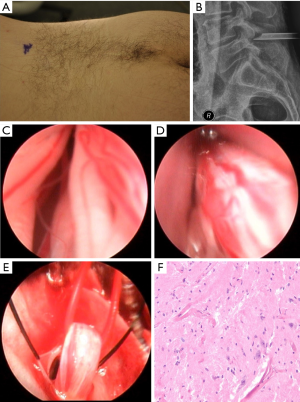
A 40-year-old male was referred for evaluation of low back and bilateral lower extremity radicular pain. The patient had undergone 18 months of conservative treatment for his lumbar 3–4 and lumbar 4–5 degenerative disc disease (Figure 1A). He noted that physical therapy only made his pain worse and a single session of lumbar traction sent electrical shocks throughout his body. A detailed history revealed that the patient had increasing urinary urgency. Magnetic resonance imaging showed spina bifida with splaying of the posterior elements from S1 caudally to S3–4 and a sacral lipomyelomeningocele at this level with fat tracking superiorly to the conus, which was tethered at the L4–L5 level, as well as expansion of the sacral spinal canal and subarachnoid space (Figure 1A-G). An AP lumbar X-ray revealed the spina bifida (Figure 1G). Physical exam revealed a 6-inch lumbar incision from a lipoma resection at birth with a patch of hair over it (Figure 2A). The patient was previously only treated for his degenerative disc disease; diagnosis of tethered cord was only made at the time of his neurosurgical evaluation.
Operative procedure
For the minimally invasive untethering procedure, the patient underwent general anesthesia and was positioned prone on the Jackson table and Wilson frame. Intraoperative monitoring electrodes were placed for both stimulated and free-run electromyograms. Motor evoked potentials were planned for bilateral quadriceps, anterior tibialis, gastrocnemius, and external anal sphincters using needle electrodes to monitor lumbosacral nerve roots. Monitoring required intravenous anesthesia using propofol and remifentanil and only short-acting muscle relaxants. A 2 cm midline vertical incision was made over the L4–5 spinous interspace. A 7 mm endoscopic tubular retractor was advanced over sequential dilators down to the ligamentum flavum using intermittent fluoroscopic guidance (Figure 2B). The Joimax TESSYS endoscopic system was used for the procedure, and the lamina, ligamentum flavum and dura were visualized endoscopically. Under endoscopic visualization, a small Lumbar 5 laminotomy was performed with the endoscopic drill and the ligamentum flavum was opened with a kerrison rongeur. At this point the endoscopic tubular retractor was removed and an expandable minimally invasive retractor was advanced. Under microscopic visualization, the laminotomy was completed and dural tacking sutures were placed on either side of the midline. A 7 mm vertical incision was then made in the dura. The endoscope was placed intradurally for visualizing the intrathecal contents. Figure 2C-E depicts the key portions of the endoscopic procedure to identify and section the filum terminale. An endoscopic grasper was used to gently pull the filum terminale out of the small dural opening. A vessel loop was then placed under it. EMG testing confirmed that there were no motor responses to stimulating the filum. Under microscopic visualization, the filum was coagulated with a bipolar electrocoagulator, then sectioned with a micro-scissor. A 3 mm piece of the filum was sent for histopathological confirmation (Figure 2F). The dura was closed under microscopic visualization with a single purse string non-resorbable suture in a water-tight fashion. The rest of the wound was closed in a standard fashion.
Postoperative course
The patient’s radicular pain resolved immediately after surgery, and he was discharged on the first postoperative day. He initially required urinary self-catheterization for elevated post-void residuals, but by one month after surgery, he was voiding normally. One year after his minimally invasive procedure, the patient has no clinical symptoms related to his previous cord tethering.
Discussion
Patients with tethered cord syndrome classically present with a triad of symptoms that include back and leg pain, weakness, and urologic symptoms (2). The diagnosis can easily be missed because tethered cord syndrome is much rarer than the presentation of degenerative disc disease or lumbar radiculopathy for which it can be easily mistaken, as in the case presented. The standard open surgery for cord untethering consists of a multilevel laminectomy, dural opening, identification of the filum and sectioning it (when untethering only requires filum sectioning) (1,2). Other studies have shown that minimally invasive open microscopic approaches with tubular and expandable retractors are sufficient to achieve the same goals as traditional open approaches (6,7). Surgical approaches for treating lipomyelomeningocele face significant risks for scar formation, nerve damage and spinal fluid leakage (4,5). The morphology of the lipomyelomeningocele in this case leant itself to a minimally invasive treatment because the lipoma tethered the cord to the filum instead of to the spinal cord. An endoscopic procedure would not have been possible if removal of the adipose mass from the spinal cord was necessary.
Other studies have shown that endoscopic visualization of the intrathecal contents and the filum terminale is possible in cadaver specimens (8,9) and in clinical patients (10,11). These studies utilize small endoscopic cameras that do not contain a working channel. The case presented here is the first case presented in the literature of (I) utilizing a working channel endoscope to identify the filum terminale and (II) utilizing endoscopic instruments to remove the filum from the intrathecal space.
This case highlights several important issues. First, the diagnosis of tethered cord syndrome in the evaluation of patients with back pain is something surgeons and spine-focused physicians must remember to consider. Second, minimally invasive spine techniques should be considered in the surgical treatment of tethered cord especially given the theoretical advantages of minimizing pain, spinal fluid leakage, and subsequent scarring. And third, endoscopic techniques are advancing. In the case presented here, endoscopic visualization and operative techniques made identification and transection of the filum terminale possible through a tiny dural opening. The small dural opening could theoretically pose the advantage of decreasing the risk of spinal fluid leakage.
Conclusions
Other studies have shown that minimally invasive spine surgical techniques are effective for surgically treating tethered cord syndrome. Here a minimally invasive approach that utilizes endoscopic techniques for the identification and sectioning of the filum terminale in tethered cord syndrome is suggested as a helpful addition in the minimally invasive spine surgeon’s armamentarium. One can imagine that as endoscopic instrumentation and techniques improve, the treatment of tethered cord could possibly be performed as an outpatient percutaneous procedure with minimal complications and patient down time.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Sarris CE, Tomei KL, Carmel PW, et al. Lipomyelomeningocele: pathology, treatment, and outcomes. Neurosurg Focus 2012;33:E3. [Crossref] [PubMed]
- Warder DE. Tethered cord syndrome and occult spinal dysraphism. Neurosurg Focus 2001;10:e1. [Crossref] [PubMed]
- Tu A, Hengel R, Cochrane DD. The natural history and management of patients with congenital deficits associated with lumbosacral lipomas. Childs Nerv Syst 2016;32:667-73. [Crossref] [PubMed]
- Arai H, Sato K, Okuda O, et al. Surgical experience of 120 patients with lumbosacral lipomas. Acta Neurochir (Wien) 2001;143:857-64. [Crossref] [PubMed]
- Kanev PM, Lemire RJ, Loeser JD, et al. Management and long-term follow-up review of children with lipomyelomeningocele, 1952-1987. J Neurosurg 1990;73:48-52. [Crossref] [PubMed]
- Potts MB, Wu JC, Gupta N, et al. Minimally invasive tethered cord release in adults: a comparison of open and mini-open approaches. Neurosurg Focus 2010;29:E7. [Crossref] [PubMed]
- Tredway TL, Musleh W, Christie SD, et al. A novel minimally invasive technique for spinal cord untethering. Neurosurgery 2007;60:ONS70-4; discussion ONS74.
- Mourgela S, Anagnostopoulou S, Sakellaropoulos A, et al. Sectioning of filum terminale externum using a rigid endoscope through the sacral hiatus. Cadaver study. J Neurosurg Sci 2008;52:71-4. [PubMed]
- Mourgela S, Anagnostopoulou S, Sakellaropoulos A, et al. Endoscopic anatomy of the thecal sac using a flexible steerable endoscope. J Neurosurg Sci 2007;51:93-8. [PubMed]
- Di X. Endoscopic spinal tethered cord release: operative technique. Childs Nerv Syst 2009;25:577-81. [Crossref] [PubMed]
- Woods KR, Colohan AR, Yamada S, et al. Intrathecal endoscopy to enhance the diagnosis of tethered cord syndrome. J Neurosurg Spine 2010;13:477-83. [Crossref] [PubMed]


