Does sitting versus standing radiographic assessment of odontoid fractures matter? A case report
Introduction
Odontoid fractures are the most common cervical spine injury in the geriatric population (1). Fracture displacement is a known risk factor for odontoid nonunion resulting in pain, stiffness, and potential neurologic deficit (2). Flexion and extension lateral radiographs may be used to assess spinal stability but are not feasible in patients with acute trauma due to pain, guarding, and the possibility of neurological injury. The relationship between odontoid fracture displacement and postural change has not been previously described. We present a unique case in which both sitting and standing radiographs were performed on a patient with type II odontoid fracture. Variable odontoid fracture displacement was seen in the two positions despite the patient being immobilized in a hard cervical collar. Various regional and global radiographic parameters in both sitting and standing positions were assessed to characterize and explain this finding.
Case presentation
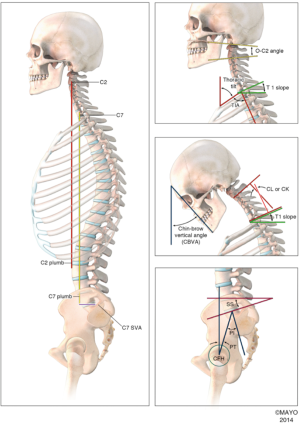
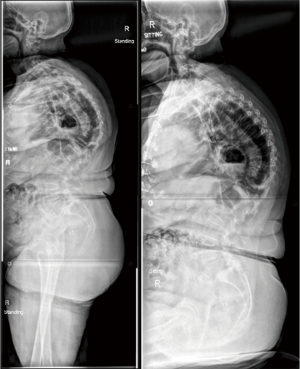
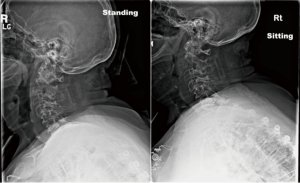
An 84-year-old female presented to the emergency department with neck pain after a ground-level fall. Physical examination revealed midline upper cervical tenderness, increased thoracic kyphosis, and no neurologic deficit. A computed tomography (CT) scan of the cervical spine demonstrated an isolated type II odontoid fracture. Upright sitting or standing cervical radiographs were ordered; misunderstanding this order, the technician obtained upright sitting and standing cervical radiographs (Figure 1). We assessed cervical spinal alignment using standard parameters as shown in Figure 2. We observed that the odontoid fragment demonstrated increased displacement and angulation on the standing compared to the sitting position (Figure 3). Initial posterior odontoid fracture displacement increased from 1.9 to 3.7 mm, occiput-C2 angle increased from 46 to 52 degrees and the C7 slope increased from 46 to 55 degrees from sitting to standing. The C2–C7 sagittal vertical axis (SVA) remained unchanged at 34 mm.
We discussed the radiographic findings and options of both surgical and non-surgical treatment with the patient and her family. Considering her age and overall medical condition, non-surgical management was elected and she was treated in a rigid cervical collar with close serial clinical and radiographic evaluations. At 10-day follow up, the patient demonstrated a similar pattern of alignment shift between sitting and standing radiographs, with the exception of C2–C7 SVA, which increased from 36 to 46 mm.
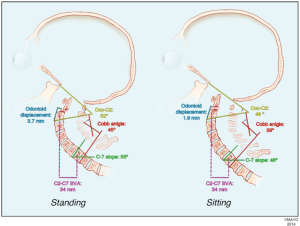
The patient was asymptomatic on last follow up at 6 months. Flexion-extension cervical radiographs demonstrated a stable nonunion without measurable displacement. Global sitting and standing films at 6 months (Figure 4) showed that thoracic kyphosis increased from 84 to 94 degrees, lumbar lordosis increased from 65 to 73 degrees, sacral slope increased from 25 to 35 degrees, and pelvic tilt decreased from 61 to 51 degrees from sitting to standing.
Discussion
Our report is the first to describe regional and global spinal alignment parameters in the sitting and standing positions in a patient with odontoid fracture. This patient demonstrated increased fracture displacement and C7 slope from sitting to standing (C7 slope was used as a surrogate for T1 slope due to image clarity); further, the occiput-C2 angle and C2–C7 lordosis increased in a concordant manner in the standing position. The relationship between sitting and standing in the thoracic and lumbar spine has been previously investigated (3-5). Vaughn et al. showed that idiopathic scoliosis patients had “straighter” spines with decreased thoracic kyphosis, lumbar lordosis, and sacral slope with sitting compared to standing (6). Cervical parameters, however, were not assessed and it was concluded that the majority of the changes occurred in the lumbar spine and pelvis.
Previous authors have shown that cervical lordosis changes in response to thoracolumbar alignment in an attempt to maintain horizontal gaze (4,7-9). We postulate that the resulting increase in cervical lordosis and occiput-C2 angle between sitting and standing on the initial radiographs was an adaptation for the patient to maintain forward horizontal gaze, due to her increased thoracic kyphosis. Subsequently, the increased lordosis in the occiput-C2 angle likely resulted in an increased posterior displacement and angulation of the cranial odontoid fragment with standing. This consideration is important as fracture displacement, a critical decision point in the management of these patients, cannot be seen as a static point in isolation but rather needs to be considered in the context of a patient’s overall spinal alignment through physiologic postures.
Conclusions
We report the first case quantifying physiologic odontoid fracture behavior with postural change and highlight the importance of regional and global spinal parameters in this growing population. Upright radiographs in both sitting and standing positions may be considered and compared with supine images when odontoid fracture stability is questioned.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Patient expired at the time of manuscript writing. Informed consent not required as per our research ethics board (Mayo Clinic).
References
- Fehlings MG, Arun R, Vaccaro AR, et al. Predictors of treatment outcomes in geriatric patients with odontoid fractures: AOSpine North America multi-centre prospective GOF study. Spine (Phila Pa 1976) 2013;38:881-6. [Crossref] [PubMed]
- Hsu WK, Anderson PA. Odontoid fractures: update on management. J Am Acad Orthop Surg 2010;18:383-94. [Crossref] [PubMed]
- Berthonnaud E, Hilmi R, Labelle H, et al. Spino-pelvic postural changes between the standing and sitting human position: proposal of a method for its systematic analysis. Comput Med Imaging Graph 2011;35:451-9. [Crossref] [PubMed]
- De Carvalho DE, Soave D, Ross K, et al. Lumbar spine and pelvic posture between standing and sitting: a radiologic investigation including reliability and repeatability of the lumbar lordosis measure. J Manipulative Physiol Ther 2010;33:48-55. [Crossref] [PubMed]
- Dunk NM, Kedgley AE, Jenkyn TR, et al. Evidence of a pelvis-driven flexion pattern: are the joints of the lower lumbar spine fully flexed in seated postures? Clin Biomech (Bristol, Avon) 2009;24:164-8. [Crossref] [PubMed]
- Vaughn JJ, Schwend RM. Sitting sagittal balance is different from standing balance in children with scoliosis. J Pediatr Orthop 2014;34:202-7. [Crossref] [PubMed]
- Cecchinato R, Langella F, Bassani R, et al. Variations of cervical lordosis and head alignment after pedicle subtraction osteotomy surgery for sagittal imbalance. Eur Spine J 2014;23 Suppl 6:644-9. [Crossref] [PubMed]
- Ha Y, Schwab F, Lafage V, et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J 2014;23:552-9. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2015;76 Suppl 1:S14-21; discussion S21.