Accuracy of minimally invasive percutaneous thoracolumbar pedicle screws using 2D fluoroscopy: a retrospective review through 3D CT analysis
Introduction
The use of minimally invasive surgical techniques in spinal instrumentation is becoming more popular aiming to optimise patient care by minimising the amount of trauma to the surrounding structures, facilitate faster recovery whilst maintaining equivalent clinical outcomes to traditional open approaches. Technical advancements in instrumentation and intra-operative imaging now allow minimally invasive spinal fusion to be performed, utilising percutaneous insertion of pedicle screws.
The importance of accurate screw placement remains paramount as it relates to optimal patient outcomes in terms of a biomechanical construct and reduced morbidity. Pedicular screw misplacement risks injury to neural, vascular and visceral structures, as well as a potential for durotomies, and pedicular fractures (1).
Pedicle screw misplacement rates using traditional open methods, relying on direct visualised anatomical landmarks and tactile feedback range between 5% and 40% (2-6). The variation in accuracy has led to technical adjuncts, predominantly intra-operative fluoroscopy and currently computer assisted 3D navigation, aiming to maintain accurate screw placement at the time of surgery.
Minimally invasive surgery utilises small-muscle splitting approaches to allow insertion of pedicle screws into the thoracic and lumbar vertebrae using incisions as small as 15 mm. The percutaneous pedicle screw placement requires intra-operative navigation either through 2D or 3D image guidance, negating the direct visual feedback, yet maintaining the tactile feedback. Many authors have described the effects and consequences of open approaches to spinal surgery, highlighting the potential advantages of minimally invasive spinal surgery including reduced analgesic requirements, less tissue damage, reduced blood loss and faster recovery times (1,7-9).
The aim of this study was to determine the misplacement rate of percutaneously inserted thoracic and lumbar pedicle screws utilising a minimally invasive technique. The rate of misplacement for 2D fluoroscopic assisted minimally invasive technique was compared to traditional open approaches and computer assisted 3D navigation techniques.
The analysis used post-operative computed tomography (CT) scans of the patients as it is the modality of choice for evaluating pedicle screw placements. CT scanning offers the advantage of providing three-dimensional data, assessing axial, sagittal and coronal planes to identify pedicular cortical breaches in any direction.
Methods
A retrospective case study was performed on a single series of patients from one surgeon (MJW). Surgery was performed across three hospital sites. All patients who underwent a minimally invasive percutaneously inserted thoracic or lumbar pedicle screw were included in the analysis. All operations were performed between October 2012 and September 2014.
CT scans were performed on the patient as part of their routine post-operative care. The patient’s notes and operative reports were further analysed to identify any patients who developed medical complications during surgery or in the post-operative period. Ethical and cross institutional approval was obtained through St Vincent’s Hospital Ethics Committee (HREC).
Surgical technique
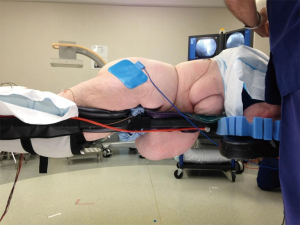
Surgery was performed by a standardised approach using Nuvasive Precept Percutaneous Pedicular Screw System (Nuvasive Pty Ltd.). The patient was anaesthetised, positioned prone on a Jackson Table with 2D fluoroscopy used for image guidance during the surgery (Figure 1). A neutral AP image was generated to ensure a linear view of the superior endplate of the vertebra being targeted enabling a clear view of pedicles bilaterally. A 15 mm incision was performed, the fascia incised and a Jamshidi needle placed under AP fluoroscopy. A Kirschner (K)-wire was inserted through the Jamshidi needle which had passed beyond the pedicle, into the vertebral body under direct fluoroscopy. The Jamshidi was removed and screws positioned over the K-wire using soft tissue protectors and sequential lateral fluoroscopic imaging. Where necessary interbody grafts were positioned, reduction of spondylolisthesis achieved and rods secured.
CT scan analysis
DICOM datasets were loaded into OsiriX (version 4.1.2, Pixmeo, Geneva, Switzerland), DICOM software viewer. A single independent observer produced multiplanar reconstructions to determine the exact screw misplacement. Misplacement was measured as millimetre (mm) breach of bony cortex of the pedicle using strict analysis and graded based on the validated system (9). Measurements were taken of the screw misplacement in multiple planes. The direction of the breach as well as other identifiable complications such as pedicle fractures or nerve root compression were recorded.
Statistical analysis
Statistical analyses were conducted using SPSS (IBM Corp., Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY, USA: IBM Corp.). Pearson’s Chi square and Fisher’s exact tests were used to analyse categorical data whereas student’s t-test was used with continuous data. Statistical significance was set at P<0.05. The rate of misplaced screws was calculated. In addition, differences in misplacement rate at individual vertebral levels, the direction of misplacement, if the screw was on the left or right side of the body and the angulation of the screw misplacement were calculated. The binomial test was used to determine any differences between laterally and medially misplaced screws.
Results
Total follow up was achieved in 108 out of 112 patients providing a follow up rate of 96.4%. In 108 patients, there were 614 pedicle screws placed in vertebral levels T2 to S1.
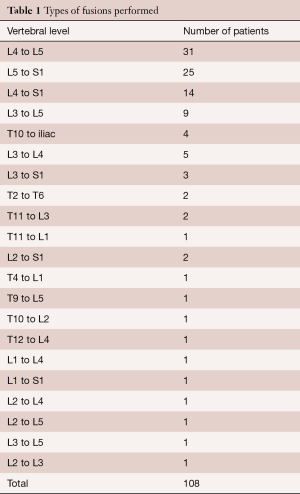
Fusions of L4 to L5 and L5 to S1 were the two most common fusions performed (Table 1). More than half of the patients (62/108, 57.4%) underwent a single level fusion, twenty-six patients (24.0%) underwent a double level fusion, five patients (4.6%) each underwent a three and eight level fusion, eight patients (7.4%) underwent a four-level fusion with two patients (0.9%) undergoing a five and nine level fusion respectively.
Full table
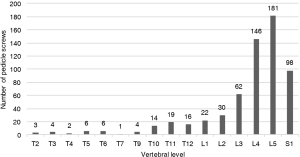
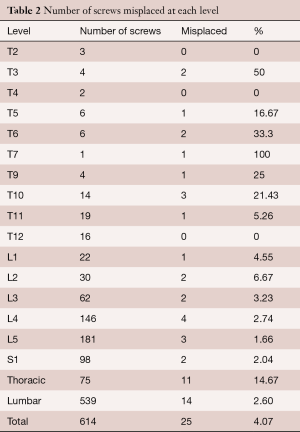
The pedicle screws were located predominantly in the lower lumbar regions where the majority of the operations were performed (Figure 2). Five hundred and eighty-nine screws were correctly placed within the pedicles. Twenty-five screws (11 thoracic, 14 lumbar) had breached the pedicular bony cortex providing a misplacement rate of 4.07% (Table 2). The misplacement rate varied across the vertebral levels with the lowest misplacement rate of 1.66% at L5 (Table 2). Overall the lumbar spine region had a low misplacement rate of 2.6%, whilst 11/75 thoracic screws had breached the cortex equating to a 14.7% misplacement rate. Thoracic and lumbar spinal level screws were compared showing significantly more misplacements in the thoracic spine pedicle screws (14.7% vs. 2.6%, χ2=24.55, P<0.001). When the thoracic spine level screws were combined and compared against individual lumbar spinal levels L3, L4, L5 and S1 had significantly fewer misplacements (Fisher’s exact test, all P<0.05) when compared to the combined thoracic spinal region.
Full table
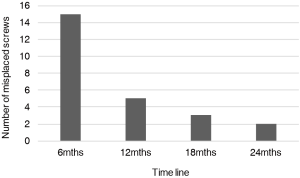
Twenty of the 25 misplaced screws took place within the first 12 months of the series. There were two screws misplaced in the last six months of the series (Figure 3).
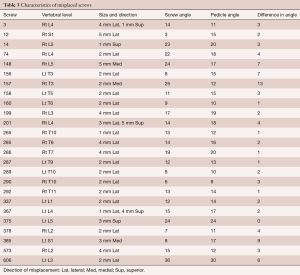
Seventeen screws were laterally misplaced by 1 to 5 mm, three screws were medially misplaced by 2 to 5 mm, three screws were superolaterally misplaced by 1 to 5 mm and two screws were superiorly misplaced by 1 to 3 mm (Table 3). More than half of the screws (14/25, 56%) in this series were misplaced 2 mm or less.
Full table
Comparing the direction of misplacement, it was observed that there were significantly more laterally than medially misplaced screws (n=20:3; P<0.001). No difference was found for medial or laterally misplaced screws in the lumbar region, yet there were significantly more laterally misplaced screws in the thoracic spine (n=10:1; P=0.012).
There were no differences between left- and right-hand side screw misplacements. On the left-hand side, there were 307 (50%) screws inserted with 10 misplacements (40% of misplaced screws) (7 lateral, 1 medial, 1 superior, 1 superolaterally) compared to on the right-hand side, there were 307 (50%) screws inserted with 15 misplacements (60% of misplaced screws) (10 lateral, 2 medial, 1 superior, 2 superolaterally).
Discussion
The misplacement rate of pedicle screws is an important criterion when assessing a surgical method of spinal instrumentation. For any new technique to be adopted it must be safe, reliable and reproducible. There are many different surgical techniques used in spinal instrumentation and a large variation in the published data on misplacement rates of these techniques. It should be noted that screw misplacement is a deviation to the perfect screw position rather than a negative consequence of the surgery and does not necessarily equate with negative outcomes for the patient (10). Most laterally misplaced screws are extremely safe and raise little concern about their position. The major concerns are the medially misplaced screws which have the potential to cause neurological injury (11,12). A strong consensus exists within the literature that misplacement of screws <2 mm (either medial or lateral) are very unlikely to cause any neurological impairment (13,14). The literature pertaining to pedicle misplacement rates varies significantly based on operative technique, with several meta-analyses confirming the variability in accurate screw placement. The largest meta-analysis of 37,337 pedicle screws inserted using an open technique, reinforced the difficulties in accurately describing the misplacement rates of pedicle screws reporting an overall misplacement rate of 8.3% (15). Further stratification into the use of navigation techniques and those without navigation, yielded misplacement rates of 4.8% and 9.7% respectively (15). A smaller meta-analysis of 7,533 screws reported an overall misplacement rate of 10.8%. and depending on the type of image navigation system used the authors found median misplacement rates 2.8–14.5% (16).
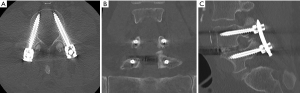
Potential confusion exists when comparing other studies results for the magnitude of pedicle screw misplacement. Weinstein et al. (17) has shown that standard plain film radiographs give significantly high rates of false-positives and false-negatives when evaluating pedicle screw placement. Our study used the exact millimetre breach of the screw to the bony cortex of the vertebral pedicle in multiple imaging planes obtained through CT. Other studies have assessed breaches in single planes, assessed breaches in categorical data groups (0–2, 2–4, >4 mm) whilst others opted to use a quarter or half a screw width as the threshold size for screw misplacement. We adopted absolute mm of screw misplacement aiming to minimise confusion and allow data to be extrapolated. The use of post-operative multiplanar imaging in this study also allowed the misplacement rate to be determined in any direction (Figure 4).
Previous studies have shown no differences in misplacement rates between the lumbar vertebral levels, corroborated by our data (9,18). Oh et al. (19) reported a non-significant higher misplacement rate in L4 and lower misplacement rate in S1 when compared to L5, possibly explained by incremental pedicular size caudally. In this series, however, the lowest misplacement rates were found at L5.
The thoracic spinal region had a significantly higher misplacement rate when compared to the lumbar spine region. This may be explained by the smaller diameter of thoracic pedicles compared to the lumbar pedicles. In all cases in this series a 4.5 or 5.5 mm diameter screw was positioned into the thoracic pedicle. The pedicle itself generally measures only 5 to 6 mm in diameter lending placement to millimetre accuracy.
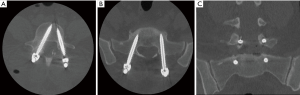
The 11 misplaced (out of 75) thoracic pedicle screws occurred in three patients. A similar study found seven out of 76 thoracic screws were misplaced with 6 screws greater than 2 mm (9). Assessing the magnitude of pedicular breach in our series only two screws were misplaced greater than 2 mm and only 1 screw was medially misplaced (2 mm) (Figure 5). Further CT analysis revealed all screws were well positioned within the vertebral body ensuring the safety of the thoracic pedicle screws. No screws required repositioning and no complications ensued suggesting that this higher misplacement rate does not appear to pose any harm to the patients, adding to the consensus that laterally placed screws will rarely cause morbidity (Figure 6).
The magnitude of the screw misplacement is an important factor in determining the clinical significance. More than half of the screws (14/25, 56%) in this series were misplaced 2 mm or less. It has been shown that screws with less than 2 mm misplacement are unlikely to cause any damage to surrounding structures (20).
More importantly the clinical relevance of a suboptimal screw placement is determined by the axial trajectory. Medially misplaced screws are potentially more dangerous as they are more likely to impact nerves and dura within the spinal canal (11,12). This study found 3 medial placed screws (0.49%) with significantly more laterally misplaced screws. As such, anatomically this will be of little immediate clinical concern to the patient and considered safe (12). There were statistically more laterally misplaced screws in the thoracic spine compared to the single medially misplaced screw. This finding was not observed in previous data utilising computer assisted navigation for the insertion of pedicular screws where no differences were observed in direction of misplacement in the thoracic spine. (9)
Assessing the lumbar spine, no difference was identified between medial and lateral misplaced screws. Previous observed data for lumbar percutaneous screws has reported more medial misplacement (18,19), with others reporting more laterally misplaced screws (9).
Operative variables
Obesity is a contributing factor to screw misplacement as surgery is technically more difficult in obese patients (21,22). Obesity affects image quality; the density of the patient’s fat and BMI will degrade the image quality of image intensifier used intraoperatively to confirm screw placement. Park et al. (23) assessed body habitus as factors for the misplacement of percutaneous lumbar pedicle screws. The authors found a higher rate of misplaced screws in the overweight group compared to the obese and normal weight groups. However, this difference was not significant, possibly due to the small size of patients (23). The screws which were misplaced and symptomatic were observed in the overweight and obese groups of patients.
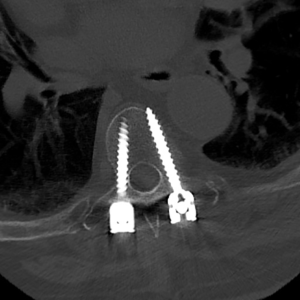
In this series, even when using the maximum allowable radiation dose, satisfactory images were able to be obtained with a low misplacement rate and very few complications. The only screw that required revision in this series of 614 pedicle placed crews was in a patient with a BMI of 42.4 (Figure 7). The image quality was degraded at the time of surgery given the patient’s habitus, yet despite this, three of the four screws were seen in optimal position (Figure 8).
Learning curve
Any new technique requires a learning curve to reach the desired goal of a reproducible, safe and reliable procedure. Percutaneous screw placement is such a technique with multiple authors confirming reduced error over time (24-27). Our consecutive series showed that 20/25 screws were misplaced within the first 12 months of the series, with two screws misplaced in the last 6 months of the series. The data supports the improved accuracy over a 2-year period. Based on our data it is not possible to determine the exact numbers of screws that are required to reach an acceptable level of accuracy and reduced morbidity. Studies have estimated that approximately 30 cases are required in minimally invasive discectomy procedures (28) and perhaps one can extrapolate this to MIS percutaneous screw placement using fluoroscopy with initial studies showing a learning curve at between 40 to 50 cases (25,26). We have analysed our own data relating to fellowship training for the accuracy of pedicle screw placement and seen statistically significant differences once trainees place more than 45 screws. The learning curve is however longer for the placement of thoracic pedicle screws.
Complications
Following insertion of 614 pedicle screws, only a single screw required revision for a clinically relevant misplacement. The L5 screw was positioned medially by 5 mm and the patient developed foot pain with no weakness in the early post-operative period. The screw was repositioned the following day and all symptoms resolved. The BMI of this patient was 42.4, making accurate fluoroscopic imaging more challenging when targeting a pedicle percutaneously. There were no other neurological complications from the remaining 613 screws.
A single patient was found to have a fractured pedicle on post-operative CT assessment. The pedicle was identified as very sclerotic at the time of surgery and despite careful surgical technique and incremental pedicular tapping prior to screw placement, the pedicle still fractured. A total of 27 sclerotic pedicles were listed, with a single fracture recorded suggesting it represents a rare event.
Limitations
Despite 614 screws placed, only a relatively small number of these were thoracic pedicle screws [75]. Of these, 11 misplaced screws were seen (10 lateral), resulting in a misplacement rate of 4.07%. The data would appear skewed towards lumbar pedicle screws yet this is simply a reflection of a particular practice, as shown by 108 consecutive patients. If thoracic screws were eliminated then the misplacement rate for lumbar screws reduces to 2.60%. Further if we excluded laterally screws, which are generally considered safe, then the accuracy improves to 99.51% (3/614). The small number of misplaced screws did not allow for a number of associations tested for, such as right or left sided screw misplacement.
This study used a blinded independent single observer to review the CT scans generating single observer bias. This bias could be minimised by the use of additional observers also blinded to the clinical outcomes optimising reliability, however the absolute values of pedicular breach was carefully assessed in all 3 dimensional planes using high quality CT.
A further potential bias related to the assessment of clinical outcome performed by the single surgeon. It would have been better validated had a blinded independent post-operative neurological assessment be performed to minimise confounders.
Radiation exposure
One must consider the radiation exposure of utilising 2D fluoroscopy for the placement of pedicle screws. When utilising minimally invasive surgical techniques there is an increase reliance on fluoroscopy to aid screw placement, with an increase in screening time (29,30). Much work has been performed assessing patient, surgeon and operating personnel, aiming to minimise exposure and possible long-term effects of ionising radiation. On average, we calculated 28 and 36 fluoroscopic images were required for a single- and two-level fusion respectively equating to a median 2 minutes and 12 seconds of screening time and median exposure of 49.35 mGray and 1.22 mGray﹒cm2 dose exposure. This is comparable to studies which have shown screening time of 2 minutes and 25 seconds for a percutaneous lumbar fusion (30), and another study utilising an ultra-low radiation imaging technique with 35.02 mGray (29). However, the significance of this remains unknown as there are different levels of exposure based on scatter and staff positioning. It is difficult to extrapolate this data with other studies, as measurements can vary significantly with techniques and subsequent dosimetry. Different imaging and navigation techniques will produce different amounts of radiation which can be a trade off with image quality. Studies have shown the use of an O-arm system, which utilises an initial 3D spin and will usually be followed by a post-operative acquisition, can produce up to 40% larger radiation dose to the patient, and compared to low dose fluoroscopy with post processing software which can reduce exposure by up to 83.5% (29,31-33). Staff are able to leave the operating theatre during certain image acquisitions meaning the dose is directed to the patient, whereas 2D fluoroscopy will generate exposure to operating staff and surgeons as well as the patient. The aim of any surgical technique is to maintain accuracy, and above all safety to the patient and staff alike. As such radiation exposure should be reduced as much as possible to prevent adverse long-term effects to both patients and staff. This can be achieved by careful positioning of the surgeon, staff and imaging equipment, tailoring the exposure parameters to each patient, and also reducing the number of images acquired during the operation. All staff wear lead lined gowns and lead lined eye glasses for protection
Recommendations
This study confirms that pedicle screws can be safely inserted percutaneously using 2D fluoroscopy with minimal complication rates. The rates of misplacement in the lumbar region were 2.6% but higher in the thoracic region (14.7%) leading to an overall rate of misplacement of 4.07%. Based on our data a learning curve is apparent, with 80% misplaced screws occurring in the first 12 months. A statistically significant difference was seen between lumbar and thoracic pedicle screw placement. It would seem reasonable to recommend that lumbar pedicle screws can be safely and reliably percutaneously placed using 2D fluoroscopy. This is supported by a large patient sample, low misplacement rate, extremely low medial misplacement rate (0.49%) and small size of screw breach. We would recommend caution with obese patients due to suboptimal image acquisition. However, in the thoracic region, despite the absence of neurological complications, the 14.7% rate of misplacement may be improved by the use of computer assisted navigation using multiplanar trajectories.
Conclusions
In this study of 108 patients involving placement of 614 percutaneous pedicle screws by a single surgeon, the misplacement rate was found to be 4.07%. Lumbar spine region screws had a misplacement rate of 2.60%. This low misplacement rate, which was also associated with an extremely low incidence of complications, confirms that minimally invasive insertion of pedicle screws utilising 2D fluoroscopy is a safe, reliable and reproducible technique. The low misplacement rate is equivalent, if not lower, than reported rates for open spinal and computer navigated forms of pedicle screw placement. Statistically significant differences were seen between rates of misplacement for lumbar and thoracic screws and as with any technique a learning curve was apparent. This study adds to the emerging spinal surgical data by contributing a large patient cohort using minimally invasive percutaneously inserted thoracic and lumbar pedicle screws.
Acknowledgements
None.
Footnote
Conflicts of Interest: MJ Winder is a Consultant and Educator for Nuvasive Pty Ltd.
Ethical Statement: The study was approved by St Vincent’s Hospital Ethics Committee (HREC).
References
- Onibokun A, Holly LT. Minimally invasive pedicle screw fixation. Operative Techniques in Neurosurgery 2004;7:72-8. [Crossref]
- Castro WH, Halm H, Jerosch J, et al. Accuracy of pedicle screw placement in lumbar vertebrae. Spine (Phila Pa 1976) 1996;21:1320-4. [Crossref] [PubMed]
- Amato V, Giannachi L, Irace C, et al. Accuracy of pedicle screw placement in the lumbosacral spine using conventional technique: computed tomography postoperative assessment in 102 consecutive patients. J Neurosurg Spine 2010;12:306-13. [Crossref] [PubMed]
- Gelalis ID, Paschos NK, Pakos EE, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 2012;21:247-55. [Crossref] [PubMed]
- Laine T, Lund T, Ylikoski M, et al. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J 2000;9:235-40. [Crossref] [PubMed]
- Shin BJ, James AR, Njoku IU, et al. Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine 2012;17:113-22. [Crossref] [PubMed]
- Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003;28:S26-35. [Crossref] [PubMed]
- Harris EB, Massey P, Lawrence J, et al. Percutaneous techniques for minimally invasive posterior lumbar fusion. Neurosurg Focus 2008;25:E12. [Crossref] [PubMed]
- Raley DA, Mobbs RJ. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine: accuracy and complication rates. Spine (Phila Pa 1976) 2012;37:1092-100. [Crossref] [PubMed]
- Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15:11-4. [Crossref] [PubMed]
- Manbachi A, Cobbold RS, Ginsberg HJ. Guided pedicle screw insertion: techniques and training. Spine J 2014;14:165-79. [Crossref] [PubMed]
- Weinstein JN, Rydevik BL, Rauschning W. Anatomic and technical considerations of pedicle screw fixation. Clin Orthop Relat Res 1992.34-46. [PubMed]
- Fisher CG, Sahajpal V, Keynan O, et al. Accuracy and safety of pedicle screw fixation in thoracic spine trauma. J Neurosurg Spine 2006;5:520-6. [Crossref] [PubMed]
- Tang J, Zhu Z, Sui T, et al. Position and complications of pedicle screw insertion with or without image-navigation techniques in the thoracolumbar spine: a meta-analysis of comparative studies. J Biomed Res 2014;28:228-39. [PubMed]
- Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 2007;32:E111-20. [Crossref] [PubMed]
- Tian NF, Xu HZ. Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop 2009;33:895-903. [Crossref] [PubMed]
- Weinstein JN, Spratt KF, Spengler D, et al. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 1988;13:1012-8. [Crossref] [PubMed]
- Wiesner L, Kothe R, Schulitz KP, et al. Clinical evaluation and computed tomography scan analysis of screw tracts after percutaneous insertion of pedicle screws in the lumbar spine. Spine (Phila Pa 1976) 2000;25:615-21. [Crossref] [PubMed]
- Oh HS, Kim JS, Lee SH, et al. Comparison between the accuracy of percutaneous and open pedicle screw fixations in lumbosacral fusion. Spine J 2013;13:1751-7. [Crossref] [PubMed]
- Stauff MP. Pedicle screw accuracy and the ramifications of imperfect screw placement. Spine J 2013;13:1758-9. [Crossref] [PubMed]
- Patel N, Bagan B, Vadera S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine 2007;6:291-7. [Crossref] [PubMed]
- Telfeian AE, Reiter GT, Durham SR, et al. Spine surgery in morbidly obese patients. J Neurosurg 2002;97:20-4. [PubMed]
- Park Y, Ha JW, Lee YT, et al. Percutaneous placement of pedicle screws in overweight and obese patients. Spine J 2011;11:919-24. [Crossref] [PubMed]
- Ahn J, Iqbal A, Manning BT, et al. Minimally invasive lumbar decompression-the surgical learning curve. Spine J 2016;16:909-16. [PubMed]
- Lee KH, Yeo W, Soeharno H, et al. Learning curve of a complex surgical technique: minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). J Spinal Disord Tech 2014;27:E234-40. [Crossref] [PubMed]
- Silva PS, Pereira P, Monteiro P, et al. Learning curve and complications of minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus 2013;35:E7. [Crossref] [PubMed]
- Wood MJ, McMillen J. The surgical learning curve and accuracy of minimally invasive lumbar pedicle screw placement using CT based computer-assisted navigation plus continuous electromyography monitoring - a retrospective review of 627 screws in 150 patients. Int J Spine Surg 2014.8. [PubMed]
- Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res 2014;472:1711-7. [Crossref] [PubMed]
- Wang TY, Farber SH, Perkins SS, et al. An Internally Randomized Control Trial of Radiation Exposure Using Ultra-Low Radiation Imaging (ULRI) Versus Traditional C-arm Fluoroscopy for Patients Undergoing Single-level Minimally Invasive Transforaminal Lumbar Interbody Fusion (TLIF). Spine (Phila Pa 1976) 2016;31:31. [PubMed]
- Fransen P. Fluoroscopic exposure in modern spinal surgery. Acta Orthop Belg 2011;77:386-9. [PubMed]
- Nakagawa H, Kamimura M, Uchiyama S, et al. The accuracy and safety of image-guidance system using intraoperative fluoroscopic images: an in vitro feasibility study. J Clin Neurosci 2003;10:226-30. [Crossref] [PubMed]
- Nelson EM, Monazzam SM, Kim KD, et al. Intraoperative fluoroscopy, portable X-ray, and CT: patient and operating room personnel radiation exposure in spinal surgery. Spine J 2014;14:2985-91. [Crossref] [PubMed]
- Tabaraee E, Gibson AG, Karahalios DG, et al. Intraoperative cone beam-computed tomography with navigation (O-ARM) versus conventional fluoroscopy (C-ARM): a cadaveric study comparing accuracy, efficiency, and safety for spinal instrumentation. Spine (Phila Pa 1976) 2013;38:1953-8. [Crossref] [PubMed]