Composite PEEK/Carbon fiber implants can increase the effectiveness of radiotherapy in the management of spine tumors
Introduction
Primary tumors of the spine are rare if compared to metastatic lesion which represents the 97% of the tumors of the spine (1). The indication of surgery and its timing in primary tumors are affected by many factors such as neurological status, histology, localization of the tumor, stability of the spine and general condition of the patients. Consequences of untreated spinal tumor include severe pain, fracture and spinal cord compression which represent a medical emergency (2).
En bloc resection is the treatment of choice of primary malignant or aggressive benign tumors (3). This is a very demanding and morbid surgical technique due to the surgical complexity, requiring double or triple approach and in any case the manipulation of more compartments (4,5). This technique frequently requires the sacrifice of functionally relevant structures like nerves, dura, vessels resulting in functional loss. Moreover, en bloc resection is not always feasible: a series of criteria of feasibility have been proposed in order to achieve a tumor-free margin specimen (6). Although technically feasible, sometimes this procedure is not accepted by the patient even if associated with a substantially reduced risk of local recurrence (LR) and with a better final outcome. Intentional transgression of oncological principles due to preserving function, incidental transgression of the margins or impossibility of achieving tumor-free margins due to lack of criteria of feasibility have increased the indication to combine gross total excision or en bloc resection with intralesional margins (separation surgery) followed by radiotherapy (7).
In the treatment of LR, en bloc resection is associated with lower effectiveness in local control (LC) therefore morbidity and functional loss are less acceptable by the patients. In these cases, intralesional excisions (from partial curettage to gross-total excision) can be combined with radiotherapy in order to achieve a better long term results (8,9).
Conventional radiotherapy has traditionally been used in the post-operative setting but, especially for some histotype of tumor such as chordoma, has not been proven to be affective treatment method (10,11).
Recently spine stereotactic body radiotherapy, carbon ion therapy and proton therapy have been proposed for the treatment of spine tumor with encouraging results (12). Data suggest that the safety and LC with these techniques are good, and a high degree of LC is seen even in patients who have spinal metastases from tumors classified as radioresistant (i.e., sarcoma) (13,14). As a result of these findings, the concept of radioresistance is being reassessed.
When the radiotherapy is performed after surgery, the presence of metal hardware can interfere due to the scattering effects of ionizing radiations or particles, leading artifacts during radiation imaging and therapy. The presence of a high-Z material in an irradiated patient results in a reducing radiation through the inhomogeneity as well as local perturbations known as interface effects. Thus, imaging results are affected by ferromagnetic artifacts and dose calculation is rendered inaccurate (15). The success or failure of radiation therapy treatments depends upon the accuracy in which target identification is correct and dose prescription is fulfilled. The presence of cold spot of the prescription dose could result in under-treating the disease with major risk of progression (16). Moreover, there will obviously be significant benefits also in defining the state of the disease detectable in TC and MRI imaging follow-up of treated patients.
The use of PEEK embedded Carbon fiber cages has been proposed in the spine surgery several years ago. This material has proven to be biocompatible and to promote bone fusion, thus resulting in excellent clinical outcome (17). Moreover, their lower modulus of elasticity better matches that of bone (18).
Recently a new fixation system (including rods and screw) fully made in PEEK embedded Carbon fiber (CFR-PEEK) has been proposed. The theoretical advantage of this system is the low artifact level at imaging, therefore it would be very useful to avoid any scattering effect during radiotherapy. As a consequence, it is conceivable that a higher dose can be forwarded to the tumor mass with lesser or no irradiation of neighboring structures.
Methods
An ambispective study was performed on the first 22 consecutive primary tumor patients, treated in a single institution from October 2014 to December 2016, who underwent spinal surgery including a composite CFR-PEEK fixation system (Carboclear™, produced by CarboFix Orthopedics® Ltd., Herziliya, IL, USA).
The inclusion criteria were patients with primary tumor in the thoracic and lumbar spine with skeletal-related events, including severe pain, pathologic fractures and epidural spinal cord compression. Patients with previously radiated spinal lesions were also included in this study.
This study was approved by the Institute’s Ethical Committee: the results of the prospective study on the first 15 patients were submitted to achieve the EC mark for the implanted device.
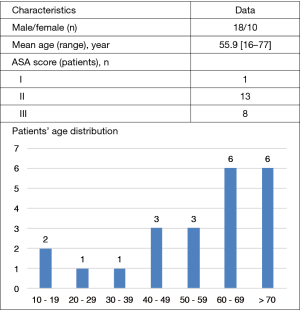
Patients characteristic are summarized in Figure 1. Twelve patients were older than 60. Fixation was associated to: (I) palliative surgery (decompression) in 3 cases; (II) tumor intralesional excision (Debulking/Curettage) in 15; (III) en bloc resection (extralesional removal of the whole tumor covered by a continuous shell of healthy tissue all around it) in 4. When reconstruction of the anterior column was needed (12 cases), composite CFR-PEEK cage was implanted in 4 cases, acrylic cement in 5 cases, titanium cage in 2 and massive allograft in 1.
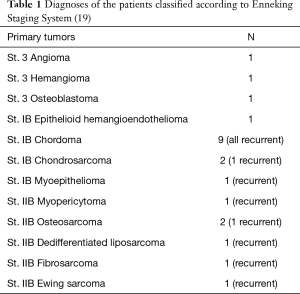
In all of the cases a histological diagnosis is available (Table 1): 16 of the 22 were recurrent. All cases were submitted to clinical and imaging studies including standard radiograms, CT scan and MRI and primary tumors were staged according to Enneking staging system (19).
Extension of fixation ranged from 3 levels (2 couple of screws, with or without anterior column reconstruction) to 9 levels. Total number of implanted screws was 167.
The construct involved the thoracic spine in 6, the lumbar spine in 1, the thoraco-lumbar junction in 8, the lumbo-sacral junction in 7.
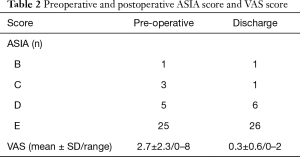
The incidence of complications (intra- and postoperative), LC and LR, and changes in neurological status were considered. The neurologic function was evaluated according to the ASIA score and the visual analogic scale (VAS) score for pain.
All the cases were submitted to post-op CT scan and standard radiograms before discharge. Periodical follow-up clinical and radiographic controls performed by the surgeons’ team were performed at 3, 6, 12 months and each year later to assess implant stability and possible tumor recurrence.
When suitable post-operative radiotherapy with photons, protons or carbon ion was performed, close contacts with the radiation oncologists were kept in order to record their opinion during treatment planning and execution.
Statistical analysis
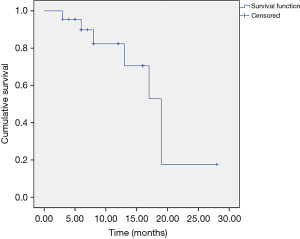
The LR of the patients was analyzed by Kaplan Meier method. Statistical analysis was performed using SPSS v.21.0 (IBM Corp., Armonk, NY, USA).
Results
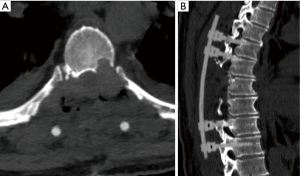
All the cases were followed 3 to 28 months (mean 10 months). Only one intraoperative complication occurred: a screw breakage during the third surgical procedure of the series. Weight-bearing was encouraged in the immediate post-operative course for all the patients without orthosis. Change in ASIA score and VAS score are summarized in Table 2. No rod breakage, neither any screw/rod disconnection was found during the considered follow-up (Figures 2,3). One cases of loosening of sacral screws were found at 12 months in one patient submitted to previous surgery and revised with CFR-PEEK screws. This was a multi recurrent malignant tumor and loosening was found at the time of the LR provoking instability of the construct.
Full table
Post-operative RT has been performed in 19 patients. In one case RT has been performed 2 times due to the progression of the tumor.
The overall number of progression of the tumour or LR was 7. In 6 of these cases the diagnosis was a recurrence, in 1 case there was an osteosarcoma without the feasibility criteria of en bloc resection therefore an intralesional excision followed by RT has been performed.
The actuarial rate of LR or progression of the tumour, calculated according to the Kaplan-Meier method, was 17.6% at 12 months (Figure 4).
Discussion
The treatment of primary spine tumors is challenging and when an en bloc resection is not feasible post-operative RT is often mandatory in order to achieve a better LC. Radiotherapy with particles (protons and ions) have gained popularity due to its selectivity allowing delivery of a high dose to the tumour (or tumour bed) sparing surrounding healthy tissues. However, RT after a spine stabilization has always been limited due to the metallic hardware used for fixation or reconstruction.
The metallic hardware affects both the contouring precision and the precise range calculation of delivered particles, thus introducing a high degree of uncertainties in calculating dose distributions. This represents a main issue for the proximity of the spinal cord, leading to a further decrease of the maximum deliverable dose of RT. Moreover metallic implants significantly differ from normal tissues in terms of density and composition producing substantial perturbation effects. As a matter of fact, any metallic artifacts following stabilization of the spine are a real challenge for the correct planning and delivery of RT with the photons and it prevents the use of RT with particles. In some series the presence of metallic hardware was the strongest predictive factor for LRs in spinal tumors treated with particle therapy (20).
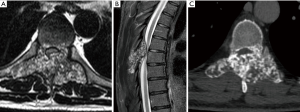
The main advantage of the composite CFR-PEEK spine stabilization systems is its radiolucency that should produce low artifact level at the imaging. If compared to metal hardware, CFR-PEEK allows one to analyze a large body segment and even to use particles for postoperative radiotherapy without any perturbation of the images and interference of the beams with metallic material. The carbonaceous orthopedic implants, thanks to their low atomic number, have radiation properties similar to those of biological tissues and, therefore, they are more suitable to patient candidates for RT. Moreover experimental data by Monte Carlo simulations and TLD measurements show that carbon plates will neither increase the incident surface dose, nor lead to the decrease of exit surface dose (the effect of a second build-up) by using six MV photons (21).
The use of CFR-PEEK allowing a better postoperative RT should lead to better results. In our series there were 7 LR with a rate of LR of 17.6% at 12 months, however, it should be pointed that in all these cases an intralesional excision or a palliative decompression has been performed without curative intent. No LR has been observed in patients in whom an en-block resection has been performed.
Radiolucency is helpful also during follow-up studies: if compared to metallic hardware the CFR-PEEK allows an optimal visualization of the bone and soft tissue structures also in the close proximity thus helping to identify any early tumor regrowth.
However CFR-PEEK also has some disadvantages: the radiolucency can make more difficult the positioning of the screws that cannot be verified using standard intraoperative radiograms, while intraoperative CT scan allows for this. Moreover, the rod contour cannot be modelled to fit the screws on the operative field and a dedicated device is required to connect a small component fixed on the rod into the screw collar. All these issues make the surgical technique not user-friendly. To overcome the intraoperative radiolucency, the producer can provide both screws covered by a thin layer of titanium or with a small reference point at the tip.
In our series, we report a screw breakage occurred while replacing a thinner titanium screw without reaming the pedicle with the diameter of the composite screw. It seems that the resistance of the screws in CFR-PEEK to rotational forces is lower than those in titanium therefore a proper tapping is mandatory. However the mechanical properties of the screws/rods construct of CFR-PEEK seems to have at least the same mechanical performances of titanium: the mechanical adverse events of this cohort of patients are not superior to those commonly observed with titanium implants.
Conclusions
Data from this preliminary report show that CFR-PEEK fixation system is comparable to standard titanium system in term of intraoperative complications, stability at weight bearing and at functional recovery.
Thanks to radiolucency, CFR-PEEK stabilization devices are more suitable in patients eligible for RT: the absence of image artifacts together with significantly less dose perturbation improve the treatment accuracy. Moreover the radiolucency is useful in the follow-up of patients thus allowing early detection of LR.
The advantage of using CFR-PEEK composite implants in terms of overall results and patients’ outcome needs to be prospectively defined with larger patient series and longer follow-up. In this perspective, even the final prognosis could be positively affected by combination of less aggressive surgery and appropriate courses of radiotherapy.
Acknowledgements
The authors are indebted with Carlo Piovani for his activity as archivist and for image processing.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study obtained the approval of the Institute’s Ethical Committee (the ethical approval ID: PROT. GEN 0033745 date 09/10/2014). An informed consent has been obtained for the use of the images.
References
- Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am 2000;31:515-28. vii. [Crossref] [PubMed]
- Expert Panel on Radiation Oncology-Bone Metastases, Lo SS, Ryu S, et al. ACR Appropriateness Criteria® Metastatic Epidural Spinal Cord Compression and Recurrent Spinal Metastasis. J Palliat Med 2015;18:573-84. [Crossref] [PubMed]
- Fisher CG, Andersson GB, Weinstein JN. Spine focus issue. Summary of management recommendations in spine oncology. Spine (Phila Pa 1976) 2009;34:S2-6. [Crossref] [PubMed]
- Kato S, Murakami H, Demura S, et al. Patient and family satisfaction with en bloc total resection as a treatment for solitary spinal metastasis. Orthopedics 2013;36:e1424-30. [Crossref] [PubMed]
- Boriani S, Bandiera S, Donthineni R, et al. Morbidity of en bloc resections in the spine. Eur Spine J 2010;19:231-41. [Crossref] [PubMed]
- Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine. Terminology and surgical staging. Spine (Phila Pa 1976) 1997;22:1036-44. [Crossref] [PubMed]
- Liu JK, Laufer I, Bilsky MH. Update on management of vertebral column tumors. CNS Oncol 2014;3:137-47. [Crossref] [PubMed]
- Stacchiotti S, Sommer J. Chordoma Global Consensus Group. Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol 2015;16:e71-83. [Crossref] [PubMed]
- Germscheid NM, Fisher CG. Focus Issue II in Spine Oncology: Compendium of Spine Oncology Recommendations. Spine (Phila Pa 1976) 2016;41 Suppl 20:S163-S70. [Crossref] [PubMed]
- Walcott BP, Nahed BV, Mohyeldin A, et al. Chordoma: current concepts, management, and future directions. Lancet Oncol 2012;13:e69-76. [Crossref] [PubMed]
- Boriani S, Chevalley F, Weinstein JN, et al. Chordoma of the spine above the sacrum. Treatment and outcome in 21 cases. Spine (Phila Pa 1976) 1996;21:1569-77. [Crossref] [PubMed]
- Zhang W, Tanaka M, Sugimoto Y, et al. Carbon-ion radiotherapy of spinal osteosarcoma with long-term follow. Eur Spine J 2016;25 Suppl 1:113-7. [Crossref] [PubMed]
- Thibault I, Chang EL, Sheehan J, et al. Response assessment after stereotactic body radiotherapy for spinal metastasis: a report from the SPIne response assessment in Neuro-Oncology (SPINO) group. Lancet Oncol 2015;16:e595-603. [Crossref] [PubMed]
- Folkert MR, Bilsky MH, Tom AK, et al. Outcomes and toxicity for hypofractionated and single-fraction image-guided stereotactic radiosurgery for sarcomas metastasizing to the spine. Int J Radiat Oncol Biol Phys 2014;88:1085-91. [Crossref] [PubMed]
- Zimel MN, Hwang S, Riedel ER, et al. Carbon fiber intramedullary nails reduce artifact in postoperative advanced imaging. Skeletal Radiol 2015;44:1317-25. [Crossref] [PubMed]
- Zoccali C, Soriani A, Rossi B, et al. The Carbofix™ “Piccolo Proximal femur nail”: A new perspective for treating proximal femur lesion. A technique report. J Orthop 2016;13:343-6. [Crossref] [PubMed]
- Kersten RF, van Gaalen SM, de Gast A, et al. Polyetheretherketone (PEEK) cages in cervical applications: a systematic review. Spine J 2015;15:1446-60. [Crossref] [PubMed]
- Hak DJ, Mauffrey C, Seligson D, et al. Use of carbon-fiber-reinforced composite implants in orthopedic surgery. Orthopedics 2014;37:825-30. [Crossref] [PubMed]
- Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res 1980.106-20. [PubMed]
- Rutz HP, Weber DC, Sugahara S, et al. Extracranial chordoma: Outcome in patients treated with function-preserving surgery followed by spot-scanning proton beam irradiation. Int J Radiat Oncol Biol Phys 2007;67:512-20. [Crossref] [PubMed]
- Xin-ye N, Xiao-bin T, Chang-ran G, et al. The prospect of carbon fiber implants in radiotherapy. J Appl Clin Med Phys 2012;13:3821. [Crossref] [PubMed]