Impact of alcohol use on 30-day complication and readmission rates after elective spinal fusion (≥2 levels) for adult spine deformity: a single institutional study of 1,010 patients
Introduction
Alcohol consumption is a modifiable lifestyle risk factor which has the potential to negatively impact surgical outcomes. Increased surgical bleeding time, length of stay (LOS), transfer to the intensive care unit (ICU), postoperative infections, wound complications and cardiopulmonary insufficiency all have been demonstrated to be associated with increased alcohol use prior to surgery (1-6). Furthermore, increased alcohol use has been associated with inferior surgical outcomes in gastrointestinal surgery (7-9), colorectal surgery (4,10,11), obstetric surgery (12), transplant surgery (13), head and neck surgery (14-16), orthopedic surgery (17-19) and neurological surgery (20). A few studies even suggest a dose-dependent effect of alcohol use on postoperative complication rates (11).
Despite these studies, few have attempted to determine the impact of alcohol use in spine surgery. Some existing studies have demonstrated increased risk of postoperative spinal hematoma (21) and pneumonia (22) in patients with increased alcohol use undergoing elective spinal surgery. However, the effect of alcohol use on 30-day readmission rates and overall complications profiles in patients undergoing elective surgery for adult spinal deformity is still unknown.
The aim of the study is to determine the impact of alcohol use on 30-day readmission rates and complications profiles after elective spinal fusion (≥2 levels) in adults undergoing spinal deformity correction.
Methods
This was a retrospective study of 1,010 adult patients undergoing elective spinal fusion (≥2 levels) for spinal deformities at a major academic institution from 2005 to 2015. Institutional Review Board approval was obtained prior to the study’s initiation. Inclusion criteria included patients (I) with available demographics and treatment; (II) who underwent elective thoraco-lumbar spinal decompression with fusion ≥3 levels; and (III) an identified alcohol use status. The patients were divided into two cohorts by their alcohol use status with “Alcohol-Use” defined as any record of alcohol use and “No-Alcohol” defined as “no alcohol use” listed on their medical record. We identified 317 (31.4%) alcohol-use patients and 693 (68.6%) no-alcohol use patients (Alcohol Use: n=317; No-Alcohol: n=693). The primary outcome of this study was unplanned hospital readmissions within 30-days of hospital discharge and 30-day complication rates.
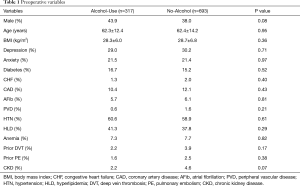
Demographic variables included sex and age. Comorbidities included body mass index (BMI), depression, anxiety, diabetes, congestive heart failure (CHF), coronary artery disease (CAD), atrial fibrillation (AFib), peripheral vascular disease (PVD), hypertension (HTN), hyperlipidemia (HLD), anemia and chronic kidney disease (CKD). We also identified any history of deep vein thrombosis (DVT) and pulmonary embolism (PE) in the patient medical records.
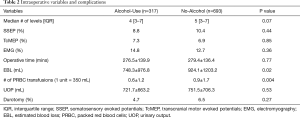
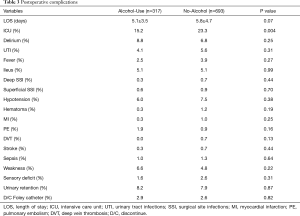
Surgical variables included operative time, median fusion levels, estimated blood loss (EBL) and number of packed red blood cell (PRBC) transfusions. Other operative variables assessed included use of somatosensory evoked potentials (SSEP), transcranial motor evoked potentials (TcMEP) and lectromyogram (EMG). Intraoperative complications included durotomy. Immediate postoperative complications included LOS, transfer to the ICU, delirium, urinary tract infections (UTI), fever, ileus, deep and superficial surgical site infections (SSI), hypotension, hematoma, myocardial infarction (MI), PE, DVT, stroke, sepsis, weakness, sensory deficits, urinary retention and discharge with a Foley catheter.
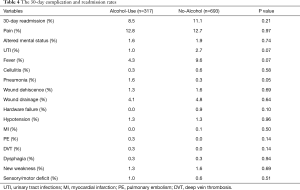
The 30-day readmission rates and complications were also recorded. Postoperative complications at 30-days included pain, altered mental status, UTI, fever, cellulitis, pneumonia, wound dehiscence, wound drainage, hypotension, MI, PE, DVT, dysphagia, new weakness and sensory/motor deficits.
Parametric data were expressed as mean ± standard deviation (SD) and compared via the Student’s t-test. Non-parametric data were expressed as median (interquartile range) and compared via the Mann-Whitney U-test. Nominal data were compared with Chi-square tests. All tests were two-sided and were significant if the P value was less than 0.05. Statistical analysis was performed using JMP®, Version 12. SAS Institute Inc., Cary, NC, 1989–2007.
Results
A total of 1,010 adult patients who underwent elective spinal fusion for correction of spinal deformity were included in the study (Alcohol-Use: n=317; No-Alcohol: n=693). There was no significant difference in age between both groups (Alcohol-Use: 62.3±12.4 years vs. No-Alcohol: 62.4±14.2 years; P=0.95) (Table 1). An approximately equal proportion of men and women were included in both groups (Alcohol-Use: 43.9% vs. No-Alcohol: 38.0%; P=0.08) (Table 1). BMI was similar in between cohorts (Alcohol-Use: 28.3±6.0 kg/m2vs. No-Alcohol: 28.7±6.8 kg/m2; P=0.36) (Table 1). There were no significant differences in the prevalence of other co-morbidities, such as depression, anxiety, diabetes, CHF, CAD, AFib, PVD, HTN, HLD, anemia and CKD (Table 1). History of prior DVT or prior PE were also similar between both cohorts ((respectively - Alcohol-Use: 2.2% vs. No-Alcohol: 3.9%; P=0.17 and Alcohol-Use: 1.6% vs. No-Alcohol: 2.5%; P=0.38) (Table 1).
Full table
The median [interquartile range] number of levels fused was similar between both cohorts {Alcohol-Use: 4 [3–7] vs. No-Alcohol: 5 [3–7]; P=0.07} (Table 2). Mean operative time between both cohorts was similar (Alcohol-Use: 276.5±139.9 minutes vs. No-Alcohol: 279.4±136.4 minutes; P=0.77) (Table 2). However, EBL and number of PRBC transfusions was significantly greater in the Alcohol-Use cohort (respectively - Alcohol-Use: 748.3±976.8 mL vs. No-Alcohol: 924.1±1,203.2 mL; P=0.02 and Alcohol-Use: 0.6±1.2 units vs. No-Alcohol: 0.9±1.7 units; P=0.004) (Table 2). UOP and incidence of durotomy were also similar between both cohorts (respectively - Alcohol-Use: 721.7±663.2 mL vs. No-Alcohol: 751.5±706.3 mL; P=0.53 and Alcohol-Use: 4.7% vs. No-Alcohol: 6.5%; P=0.27) (Table 2).
Full table
Immediate postoperative complications profile
LOS was similar in the No-Alcohol cohort compared to the Alcohol-Use cohort (Alcohol-Use: 5.1±3.5 days vs. No-Alcohol: 5.8±4.7 days; P=0.07) (Table 3). However, a greater percentage of the No-Alcohol cohort were transferred to the ICU than the Alcohol-Use cohort (Alcohol-Use: 15.2% vs. No-Alcohol: 23.3%; P=0.004) (Table 3). There was no significant difference in the incidence of other immediate postoperative complications: delirium (Alcohol-Use: 8.8% vs. No-Alcohol: 6.8%; P=0.25), UTI (Alcohol-Use: 4.1% vs. No-Alcohol: 5.6%; P=0.31), fever (Alcohol-Use: 2.5% vs. No-Alcohol: 3.9%; P=0.27), ileus (Alcohol-Use: 5.1% vs. No-Alcohol: 5.1%; P=0.99), deep SSI (Alcohol-Use: 0.3% vs. No-Alcohol: 0.7%; P=0.44), superficial SSI (Alcohol-Use: 0.6% vs. No-Alcohol: 0.9%; P=0.70), hypotension (Alcohol-Use: 6.0% vs. No-Alcohol: 7.5%; P=0.38), hematomas (Alcohol-Use: 0.3% vs. No-Alcohol: 1.2%; P=0.19), MI (Alcohol-Use: 0.3% vs. No-Alcohol: 1.0%; P=0.25), PE (Alcohol-Use: 1.9% vs. No-Alcohol: 0.9%; P=0.16), DVT (Alcohol-Use: 0.0% vs. No-Alcohol: 0.7%; P=0.13), stroke (Alcohol-Use: 0.3% vs. No-Alcohol: 0.7%; P=0.44), sepsis (Alcohol-Use: 1.0% vs. No-Alcohol: 1.3%; p=0.64), weakness (Alcohol-Use: 6.6% vs. No-Alcohol: 4.8%; P=0.22), sensory deficits (Alcohol-Use: 1.6% vs. No-Alcohol: 2.6%; P=0.31) and urinary retention (Alcohol-Use: 8.2% vs. No-Alcohol: 7.9%; P=0.87) (Table 3). Discharge with a Foley Catheter was similar between the two cohorts (Alcohol-Use: 2.9% vs. No-Alcohol: 2.6%; P=0.82) (Table 3).
Full table
The 30-day readmission rates and postoperative complications profile
There was no significant difference in 30-day unplanned readmission rates between both cohorts (Alcohol-Use: 8.5% vs. No-Alcohol: 11.1%; P=0.21). Incidence of postoperative pneumonia trended to be greater in the Alcohol-Use cohort compared with the No-Alcohol cohort (P=0.05) (Table 4). There was no significant difference in the incidence of other 30-day postoperative complications: pain (Alcohol-Use: 12.8% vs. No-Alcohol: 12.7%; P=0.97), altered mental status (Alcohol-Use: 1.6% vs. No-Alcohol: 1.9%; P=0.74), UTI (Alcohol-Use: 1.0% vs. No-Alcohol: 2.7%; P=0.07), fever (Alcohol-Use: 4.3% vs. No-Alcohol: 9.6%; P=0.07), cellulitis (Alcohol-Use: 0.3% vs. No-Alcohol: 0.6%; P=0.58), wound dehiscence (Alcohol-Use: 1.3% vs. No-Alcohol: 1.6%; P=0.69), wound drainage (Alcohol-Use: 4.1% vs. No-Alcohol: 4.8%; P=0.64), hardware failure (Alcohol-Use: 0.0 vs. No-Alcohol: 0.9%; P=0.10), hypotension (Alcohol-Use: 1.3% vs. No-Alcohol: 1.3%; P=0.96), MI (Alcohol-Use: 0.0% vs. No-Alcohol: 0.1%; P=0.50), PE (Alcohol-Use: 0.3% vs. No-Alcohol: 0.0%; P=0.14), DVT (Alcohol-Use: 0.3% vs. No-Alcohol: 0.0%; P=0.14), dysphagia (Alcohol-Use: 0.3% vs. No-Alcohol: 0.3%; P=0.94), new weakness (Alcohol-Use: 1.3% vs. No-Alcohol: 1.6%; P=0.69) and sensory/motor deficits (Alcohol-Use: 1.0% vs. No-Alcohol: 0.6%; P=0.51) (Table 4).
Full table
Discussion
In this retrospective cohort study assessing outcomes after spinal fusion for correction of adult spinal deformity, we demonstrated a similar incidence of postoperative complications and 30-day readmission rates between patients with and without alcohol use.
Recent studies have demonstrated no clinically significant impact of alcohol use on surgical outcomes. In a retrospective study of 3,041 patients undergoing fast-track hip and knee arthroplasty, Jorgensen et al. determined that alcohol use was not associated with a prolonged LOS >4 days or an increased risk of readmissions at 30- or 90-day follow-up. Furthermore, the authors found that there was no increased risk of specific readmissions for complications typically related to alcohol at 90-days (23). In another retrospective cohort study of 13,065 patients undergoing elective coronary artery bypass graft surgery, Maheshwari et al. found that alcohol consumption was not associated with the risk of postoperative complications (24). Moreover, in a systematic review and meta-analysis of fifteen observational studies assessing postoperative complications among alcohol users and two randomized controlled trials assessing perioperative alcohol interventions, Shabanzadeh and Sørensen determined that alcohol use was not an independent risk factor for SSI and that interventions aimed at alcohol cessation did not have a clinical effect on the risk for SSI (25). Analogous to these studies, our study showed that alcohol consumption was not significantly associated with either increased postoperative complications or 30-day readmission rates in patients undergoing elective spine surgery.
In contrast, some studies have even suggested a protective effect of alcohol consumption. In a retrospective study of 148 patients undergoing elective spine surgery for a lumbar disc herniation, Rasmussen found that alcohol consumption, in particular wine intake, was associated with a favorable prognosis after first-time lumbar disc surgery (26). In a retrospective study of 20,124 patients undergoing hip and knee arthroplasties, Maradit Kremers et al. also determined that alcohol use was associated with a lower risk of re-operations and revisions surgeries (27).
Studies have demonstrated an increased impact of alcohol use on postoperative complications in patients undergoing spinal surgeries (1-6). In a prospective cohort study of 154 patients undergoing posterior instrumented adult spinal surgery, Boetto et al. found that alcohol consumption was associated with increased incidence of postoperative SSI (28). Similarly, a retrospective study of 1,095 patients undergoing spinal procedures by Fang et al. determined that alcohol abuse was a significant preoperative risk factor for postoperative infections (29). In a retrospective study of 220,522 patients undergoing anterior, posterior and anterior/posterior approaches for lumbar fusions from the Nationwide Inpatient Sample database, Fineberg et al. demonstrated that alcohol abuse was an independent predictor of postoperative ileus (30). In another retrospective study of 292,177 patients undergoing lumbar decompression and 286,280 patients undergoing lumbar fusion, Fineberg et al. demonstrated that alcohol abuse was an independent predictor of delirium (31).
The impact of alcohol on postoperative complication profiles is still being debated and may vary according to surgical subspecialty. However, current recommendations regarding preoperative alcohol consumption trend towards overall alcohol cessation, regardless of the procedure. In a systematic review of the contemporary alcohol guidelines, Tønnesen et al. recommends alcoholic abstinence starting 3–8 weeks prior to surgery in order to reduce the incidence of several postoperative complications, including infections, wound complications and cardiopulmonary complications (32). Additionally, perioperative alcohol cessation interventions have been suggested and two randomized clinical trials have found that intensive alcohol cessation interventions are effective in reducing postoperative complication rates (2,33).
Reductions in postoperative complications and 30-day readmission rates are associated with decreased utilization and costs of care and improved long-term patient outcomes (34,35). In addition, it has been reported that the prevalence of alcohol use within surgical populations is as great as 49% (36). If alcohol use is indeed associated with a decrease in postoperative complications and readmission rates, the current recommendations for intensive alcohol cessation programs may prove fruitful in decreasing costs of care due to complications and unplanned readmissions. However, with recent studies pointing to the reduced impact of perioperative alcohol use on the incidence of postoperative complications and 30-day hospital readmission rates, the true effect of alcohol use on patient outcomes is unclear. Our study demonstrated that there was no significant clinical effect of alcohol use on postoperative complications and 30-day readmission rates, further suggesting that alcohol use may not be a significant factor in determining postoperative patient outcomes.
This study has limitations, ensuing implications for its interpretation. First, the data was acquired via chart reviews and are subject to the weaknesses of a retrospective analysis. Secondly, determination of alcohol use was recorded based on self-reported data from the patients and may be subject to underreporting by the patient. Additionally, because the data was obtained via chart reviews, we are limited to the classification of alcohol use based on what was listed in the respective patient medical records. Fourth, the amount of alcohol use could not be stratified and was not accounted for in the analysis. Therefore, any underlying effect of alcohol use on complication and readmission rates could have been masked. Despite these limitations, the study demonstrates that both alcohol use and no alcohol use have similar incidence of postoperative complications and readmission rates at 30-days following spinal fusion.
Conclusions
Current data on the impact of alcohol use on surgical outcomes is controversial. Our study suggests that there is a reduced impact of alcohol use on 30-day complication and readmission rates among adult patients undergoing elective spinal fusion for the correction of spinal deformities.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board approval was obtained prior to the study’s initiation.
References
- Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg 1999;86:869-74. [Crossref] [PubMed]
- Oppedal K, Møller AM, Pedersen B, et al. Preoperative alcohol cessation prior to elective surgery. Cochrane Database Syst Rev 2012.CD008343. [PubMed]
- Rantala A, Lehtonen OP, Niinikoski J. Alcohol abuse: a risk factor for surgical wound infections? Am J Infect Control 1997;25:381-6. [Crossref] [PubMed]
- Tønnesen H, Petersen KR, Højgaard L, et al. Postoperative morbidity among symptom-free alcohol misusers. Lancet 1992;340:334-7. [Crossref] [PubMed]
- Shabanzadeh DM, Sørensen LT. Alcohol Consumption Increases Post-Operative Infection but Not Mortality: A Systematic Review and Meta-Analysis. Surg Infect (Larchmt) 2015;16:657-68. [Crossref] [PubMed]
- Eliasen M, Grønkjær M, Skov-Ettrup LS, et al. Preoperative alcohol consumption and postoperative complications: a systematic review and meta-analysis. Ann Surg 2013;258:930-42. [Crossref] [PubMed]
- Mantziari S, Hübner M, Demartines N, et al. Impact of preoperative risk factors on morbidity after esophagectomy: is there room for improvement? World J Surg 2014;38:2882-90. [Crossref] [PubMed]
- Nath B, Li Y, Carroll JE, et al. Alcohol exposure as a risk factor for adverse outcomes in elective surgery. J Gastrointest Surg 2010;14:1732-41. [Crossref] [PubMed]
- Spies CD, Nordmann A, Brummer G, et al. Intensive care unit stay is prolonged in chronic alcoholic men following tumor resection of the upper digestive tract. Acta Anaesthesiol Scand 1996;40:649-56. [Crossref] [PubMed]
- Nickelsen TN, Jørgensen T, Kronborg O. Lifestyle and 30-day complications to surgery for colorectal cancer. Acta Oncol 2005;44:218-23. [Crossref] [PubMed]
- Sørensen LT, Jørgensen T, Kirkeby LT, et al. Smoking and alcohol abuse are major risk factors for anastomotic leakage in colorectal surgery. Br J Surg 1999;86:927-31. [Crossref] [PubMed]
- Felding C, Jensen LM, Tønnesen H. Influence of alcohol intake on postoperative morbidity after hysterectomy. Am J Obstet Gynecol 1992;166:667-70. [Crossref] [PubMed]
- Lowery EM, Kuhlmann EA, Mahoney EL, et al. Heavy alcohol use in lung donors increases the risk for primary graft dysfunction. Alcohol Clin Exp Res 2014;38:2853-61. [Crossref] [PubMed]
- Hirakawa H, Hasegawa Y, Hanai N, et al. Surgical site infection in clean-contaminated head and neck cancer surgery: risk factors and prognosis. Eur Arch Otorhinolaryngol 2013;270:1115-23. [Crossref] [PubMed]
- Patel RS, McCluskey SA, Goldstein DP, et al. Clinicopathologic and therapeutic risk factors for perioperative complications and prolonged hospital stay in free flap reconstruction of the head and neck. Head Neck 2010;32:1345-53. [Crossref] [PubMed]
- Furr AM, Schweinfurth JM, May WL. Factors associated with long-term complications after repair of mandibular fractures. Laryngoscope 2006;116:427-30. [Crossref] [PubMed]
- Williams G, Daly M, Proude EM, et al. The influence of alcohol and tobacco use in orthopaedic inpatients on complications of surgery. Drug Alcohol Rev 2008;27:55-64. [Crossref] [PubMed]
- Williams-Russo P, Urquhart BL, Sharrock NE, et al. Post-operative delirium: predictors and prognosis in elderly orthopedic patients. J Am Geriatr Soc 1992;40:759-67. [Crossref] [PubMed]
- Tønnesen H, Pedersen A, Jensen MR, et al. Ankle fractures and alcoholism. The influence of alcoholism on morbidity after malleolar fractures. J Bone Joint Surg Br 1991;73:511-3. [PubMed]
- Cote DJ, Karhade AV, Burke WT, et al. Risk factors for post-operative respiratory failure among 94,621 neurosurgical patients from 2006 to 2013: a NSQIP analysis. Acta Neurochir (Wien) 2016;158:1639-45. [Crossref] [PubMed]
- Amiri AR, Fouyas IP, Cro S, et al. Postoperative spinal epidural hematoma (SEH): incidence, risk factors, onset, and management. Spine J 2013;13:134-40. [Crossref] [PubMed]
- Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001;135:847-57. [Crossref] [PubMed]
- Jørgensen CC, Kehlet H. Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative Group. Outcomes in smokers and alcohol users after fast-track hip and knee arthroplasty. Acta Anaesthesiol Scand 2013;57:631-8. [Crossref] [PubMed]
- Maheshwari A, Dalton JE, Yared JP, et al. The association between alcohol consumption and morbidity and mortality in patients undergoing coronary artery bypass surgery. J Cardiothorac Vasc Anesth 2010;24:580-5. [Crossref] [PubMed]
- Shabanzadeh DM, Sørensen LT. Alcohol drinking does not affect postoperative surgical site infection or anastomotic leakage: a systematic review and meta-analysis. J Gastrointest Surg 2014;18:414-25. [Crossref] [PubMed]
- Rasmussen C. Lumbar disc herniation: favourable outcome associated with intake of wine. Eur Spine J 1998;7:24-8. [Crossref] [PubMed]
- Maradit Kremers H, Kremers WK, et al. Social and Behavioral Factors in Total Knee and Hip Arthroplasty. J Arthroplasty 2015;30:1852-4. [Crossref] [PubMed]
- Boetto J, Chan-Seng E, Lonjon G, et al. Is hospital information system relevant to detect surgical site infection? Findings from a prospective surveillance study in posterior instrumented spinal surgery. Orthop Traumatol Surg Res 2015;101:845-9. [Crossref] [PubMed]
- Fang A, Hu SS, Endres N, et al. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 2005;30:1460-5. [Crossref] [PubMed]
- Fineberg SJ, Nandyala SV, Kurd MF, et al. Incidence and risk factors for postoperative ileus following anterior, posterior, and circumferential lumbar fusion. Spine J 2014;14:1680-5. [Crossref] [PubMed]
- Fineberg SJ, Nandyala SV, Marquez-Lara A, et al. Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine (Phila Pa 1976) 2013;38:1790-6. [Crossref] [PubMed]
- Tønnesen H, Nielsen PR, Lauritzen JB, et al. Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth 2009;102:297-306. [Crossref] [PubMed]
- Tonnesen H, Rosenberg J, Nielsen HJ, et al. Effect of preoperative abstinence on poor postoperative outcome in alcohol misusers: randomised controlled trial. BMJ 1999;318:1311-6. [Crossref] [PubMed]
- Boozary AS, Manchin J, Wicker RF. The Medicare Hospital Readmissions Reduction Program: Time for Reform. JAMA 2015;314:347-8. [Crossref] [PubMed]
- Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 2011;254:907-13. [Crossref] [PubMed]
- Tønnesen H. Alcohol abuse and postoperative morbidity. Dan Med Bull 2003;50:139-60. [PubMed]


