Primary leiomyosarcoma of the spine treated with total en bloc spondylectomy: the first case in Thailand—a case report and literature review
Introduction
Leiomyosarcoma is one of the most aggressive soft tissue sarcomas, accounting for approximately 7% of all soft tissue sarcomas (1,2). It originates from smooth muscle cells and typically arises in the uterus, abdominal viscera, retroperitoneal space, and soft tissue of the extremities (3). Primary osseous leiomyosarcoma is very rare and first published by Evans and Sanerkin in 1965 (4). The most common site of the osseous leiomyosarcoma is femur (5-8). Primary leiomyosarcoma of the spine is extremely rare due to the difficulty of the diagnosis. The diagnosis of primary leiomyosarcoma of spine have to exclude the possibility of the spinal metastasis from the other primary source. In general, the goals of surgery for the solitary spine tumors or localized spinal metastases are to correct and prevent any further deformity by stabilizing the spine, decompressing neural structures (spinal cord and nerves), obtaining a diagnosis if the primary is unknown, and preventing local recurrence (9). One of the surgical treatment options is total corpectomy or spondylectomy, a complete removal of vertebra. The first case of a total spondylectomy was published by Bertil Stener in 1971 in a case of chondrosarcoma of T6–T8 in a 49-year-old farmer (10). Later, larger series of this surgical procedure (20 cases of solitary spinal tumor or localized spinal metastasis) were published by Tomita et al. in 1994 with the newer technique, Tomita’s technique or total en bloc spondylectomy (TES), which have an advantage of minimize the local recurrence (11). This new surgical technique involves en bloc removal of the lesion, that is, removal of the whole vertebra, both body and lamina as one compartment (12). TES procedure was designed to achieve complete tumor resection en bloc, including main and satellite microlesions in a vertebral compartment to avoid local recurrence. The primary candidates for TES are primary malignant tumor (stage 1, 2); aggressive benign tumor (stage 3); and isolated metastasis in a patient with long life expectancy (13).
In Thailand, the first TES was published by Chanplakorn et al. in 2011 in a case of recurrent epithelioid sarcoma in the thoracic spine in a 14-year-old boy (14). In this report, we present the first diagnosed of primary leiomyosarcoma of the T12 vertebra in Thailand treated with TES.
Case presentation
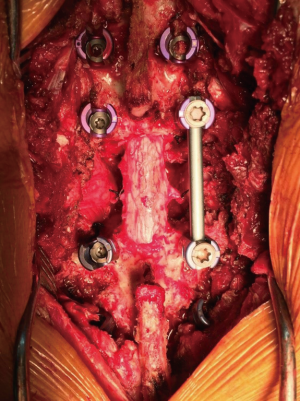
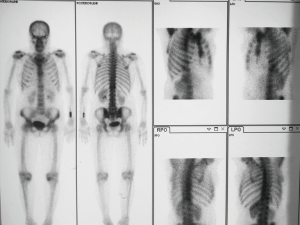
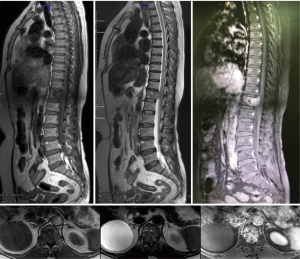
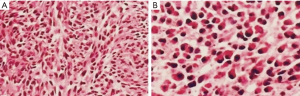
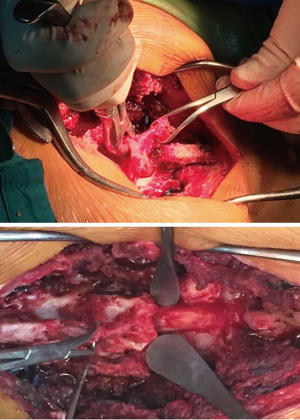
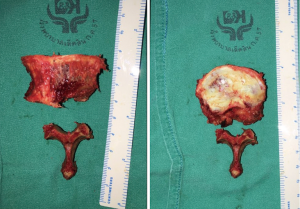
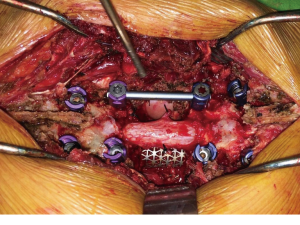
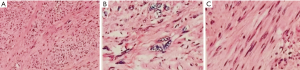
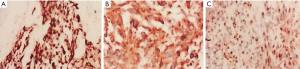
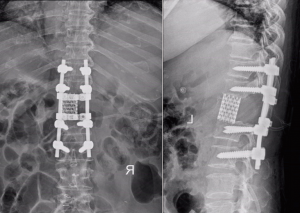
A 61-year-old Thai female was transferred and admitted to our institution in August 2016 with the chief complaint of severe backache for a few months and progressive hip flexors weakness for 1 week. At previous hospital, her chief complaint was back pain for 1 month without neurological deficit. Her symptoms were aggravated at night and could not be relieved by rest or oral analgesics. She had no symptoms of numbness, weakness, or abnormal sensation of the extremities. The radiographs of the thoracolumbar spine revealed osteolytic lesion at T12 vertebra and provisional diagnosis was tuberculosis of the spine. During this period, her clinical signs were not resolved. Furthermore, she had rapidly progressive weakness of both lower extremities, so she was subsequently referred to our institution. Physical examination revealed generalized bilateral lower extremities weakness, most marked in the hip flexors (grade II). Sensory examination showed hypoesthesia in the distribution of bilateral T12 dermatomes. Normoreflexia was observed. Laboratory findings were within normal limits and tumor markers including CA 125, CA 19-9, CA 15-3, carcinoembryonic antigen (CEA) and alpha-fetoprotein (AFP) were unremarkable. Plain radiographs of the spine revealed osteolytic lesion at T12 vertebral body (Figure 1). Bone scan (Tc-99m MDP) (29 July 2016) revealed increased tracer uptake at right side of T12 vertebra. The rest of skeletal uptake appeared unremarkable (Figure 2). Computerized Tomography scan of thorax from the previous hospital (13 July 2016) demonstrated normal of lung parenchyma without significant lung infiltration, lung mass or lung nodule. No mediastinal mass or lymph nodes enlargement were detected. Computerized tomography scan of whole abdomen from the previous hospital (13 July 2016) demonstrated no abnormal hepato-biliary system. Rectum, colon, small bowel, stomach, spleen, pancreas, adrenal glands, uterus and adnexae were unremarkable. There was 8.5 cm simple cyst at right upper pole of right kidney without solid mass. Normal renal excretion, ureters, bladder with no visible stone, mass or tract dilatation were demonstrated. Magnetic resonance image from the previous hospital (7 July 2016) revealed abnormal marrow signal intensity of T12 vertebral body. The images also showed heterogeneous T1 hypointense T2/STIR hyperintense and heterogeneous enhancement, associated with anterior epidural enhancing soft tissue along lower T11-upper L1 levels encroached bilateral T11/12 and T12/L1 neural foramina, with indentation to the conus medullaris without definite myelopathy. Bilateral psoas muscles appeared unremarkable. Magnetic resonance image was repeated (14 August 2016) and revealed abnormal intramedullary lesion at T12 vertebra involving from anterior to posterior column with posterior epidural extension into spinal canal causing anterior indentation on conus medullaris but still preserved normal signal intensity (Figure 3). Moreover, the MRI showed a 3.3 cm × 3.0 cm × 5.9 cm heterogeneously enhancing mass at right lower abdomen abutting anterior aspect of superficial fascia of right psoas muscle at the level between superior endplate of L4 vertebra and inferior endplate of L5 vertebra, also four enhancing nodules in hepatic segment IVa, VI, and VII with restricted diffusion, size up to 1.4 cm, probably liver metastasis. The percutaneous transpedicle biopsy of T12-vertebra was performed and histopathological studies showed short spindle-shaped cells infiltrates as fascicular pattern. These cells had round to oval nuclei, hyperchromasia, and eccentric nuclei. Large amount of eosinophilic cytoplasm was recognized. Mitoses were rarely seen (Figure 4). The patient was preliminarily diagnosed as Spindle-cell tumor at T12 vertebra. After preoperative preparation was done, TES of T12 vertebra was performed in one-stage posterior only approach (Tomita’s technique) (15) by Dr. Piyaskulkaew, Dr. Kunakornsawat and orthopaedics spine team. The upper resection margin was intervertebral disc T11–12 and the lower end resection margin was intervertebral disc T12–L1 where the tumor was not involved. A straight vertical midline incision was made over the spinous processes from T10 to L2. The paraspinal muscles were dissected from spinous processes and the laminae, and resected laterally. The biopsy tract was carefully resected in standard technique. After successful exposure, superior articular process of the T12, the spinous process and the inferior articular process of the T11 were osteotomized and removed with the attachment of soft tissue tumor mass infiltrated into the paraspinal muscles, including the ligamentum flavum (Figure 5). Then, T12 nerve roots and segmental arteries were identified bilaterally, ligated and cut (Figure 6). The blunt dissection was done on both sides through the plane between the pleura and the T12-vertebral body. Both of lateral sides of the T12-vertebral body were continually dissected, the aorta was carefully dissected posteriorly from the anterior aspect of the vertebral body with a spatula. After all of the structures in all planes were identified, the discectomy of T11–12 and T12–L1 were performed. The anterior and posterior longitudinal ligaments were also removed. The mobility of the T12-vertebral body was checked to ensure a complete corpectomy and then rotated around the spinal cord and removed carefully to avoid injury to the spinal cord (Figure 7). The Titanium mesh cage filled inside with autologous iliac bone graft was applied for the anterior supporting structure and pedicular screws, rods and cross-linked bars were applied from T10 to L2 as posterior structural support (Figure 8). The operative time was 7 hours and intraoperative blood loss was 1,100 mL. The surgically resected tissue was sent to the department of pathology for histopathological examination. The section showed encapsulated mass with diffuse fascicle of neoplastic cells infiltrates. The cells have spindle-shaped and large atypical cells, oval nuclei, vesicular chromatin, fine chromatin, and eosinophilic cytoplasm. Resection margins were free of tumor (Figure 9). The specific immunohistochemistry studies showed positive for desmin, smooth muscle actin, muscle specific actin, cytokeratin (AE1/AE3), h-caldesmon (Figure 10). The final diagnosis was leiomyosarcoma. The postoperative X-ray was shown in (Figure 11). A few days later, the patient underwent explore laparotomy with tumor resection at right psoas muscle with retroperitoneal lymph nodes resection. The surgically resected tissue was also sent for histopathological examination and the report were similarly. Finally, the patient was diagnosed as primary leiomyosarcoma of twelfth thoracic vertebra with liver metastasis. After surgery, the overall symptoms were relieved gradually and the motor power of hip flexors were improved bilaterally from grade II to grade IV. After discharge, the patient was continually treated with chemotherapy. Six months of follow-up, no clinical symptoms or signs of local recurrence were detected.
Discussion
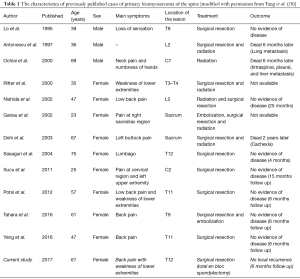
Leiomyosarcoma is one of the most aggressive soft tissue sarcomas, which originates from mesenchymal cells. These cells tend to differentiate into smooth muscle cells (16), frequently occur in uterus, abdominal viscera, retroperitoneal space, and soft tissue of the extremities. Primary leiomyosarcoma of spine is an extremely rare condition. The diagnosis are made by excluded the possibility of the spinal metastasis from the other primary source. Immunohistochemistry studies are the important investigation to confirm the diagnosis of leiomyosarcoma, especially in differentially diagnoses from other type of carcinomas. From the previous studies, primary leiomyosarcoma of the spine have been reported only 12 cases (17-28). This case was the 13th case, which summarized in the Table 1. The first case report was published by Lo et al. in 1995 with the eighth thoracic vertebral lesion, causing compression of the spinal cord. The most common site of the spine was thoracic spine in 7 cases, followed by cervical spine 2 cases, lumbar spine 2 cases, and sacrum 2 cases. The female:male ratio was 10:3 and the average age of the patients at the time of the diagnosis were 49.38 years old (23–75 years old). The treatment of primary leiomyosarcoma of the spine remains controversial depends on the patient’s age, location of the tumor, size of the tumor, and staging of the tumor. According to the studies, 5 cases were treated with surgical resection alone, 4 cases were treated with surgical resection combined with radiation, 1 case was treated with surgical resection combined with radiation and embolization, 1 case was treated with surgical resection and chemotherapy, 1 case was treated with surgical resection and embolization, and 1 case was treated with radiation alone. The overall prognosis was poor. After the diagnosis was made. two cases had died 6 months later due to metastasis, 1 case had died 2 years after due to cachexia, 2 cases were loss follow up, and 8 cases are still follow up (6 months to 2 years follow-up). According to Gladdy et al. reported in 2013 (29), the predictor of the survival and recurrence of primary leiomyosarcoma, only high grade and size were significant independent predictors of disease-specific survival. Significant independent predictors for local recurrence were size and margin, whereas predictors for distant recurrence were size and grade. Site was not an independent predictor of recurrence; however, late recurrence (>5 years) occurred in 9% of abdominal/retroperitoneal and 4% of extremity lesions but the recurrence rate of primary leiomyosarcoma of the spine still not known, In our patient, the diagnosis was made from the clinical presentation, physical examination, laboratory findings, images studies from the previous hospital and confirmation by tissue biopsy before planning the definite treatment. At that time, the diagnosis was primary leiomyosarcoma of the twelfth vertebra. Unfortunately, the disease was progress rapidly with tumor extension to psoas muscle and liver metastasis. The patient was continually treated with chemotherapy. During 6 months of follow-up, no clinical symptoms and signs of local recurrence or contiguous spreading were detected.
Full table
In conclusion, primary leiomyosarcoma of the spine is an extremely rare and difficult to diagnosis. Immunohistochemistry studies are very important for confirmation of the diagnosis. Standard treatment remains controversial. However, surgical resection is still treatment of choice. One of the most effective surgical options is TES, which give the better outcome and minimize local recurrence, if indicate.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Nanassis K, Alexiadou-Rudolf C, Tsitsopoulos P. Spinal manifestation of metastasizing leiomayosarcoma. Spine 1999;24:987-9. [Crossref] [PubMed]
- Russell WO, Cohen J, Enzinger F, et al. A clinical and pathological staging system for soft tissue sarcomas. Cancer 1977;40:1562-70. [Crossref] [PubMed]
- Ziewacz JE, Lau D, Marca FL, et al. Outcomes after surgery for spinal metastatic leiomyosarcoma. J Neurosurg Spine 2012;17:432-7. [Crossref] [PubMed]
- Evans DM, Sanerkin NG. Primary leiomyosarcoma of bone. J Pathol Bacteriol 1965;90:348-50. [Crossref] [PubMed]
- Kameda N, Kagesawa M, Hiruta N, et al. Primary leiomyosarcoma of bone. A case report and review of the literature. Acta Pathol Jpn 1987;37:291-303. [PubMed]
- Hannachi Sassi S, Khattech R, Dhouib R, et al. Primary bone leiomyosarcoma. Anatomo-clinical, immunohistochemical, and ultrastructural study. Rev Chir Orthop Reparatrice Appar Mot 1999;85:865-70. [PubMed]
- Bouaziz MC, Chaabane S, Mrad K, et al. Primary leiomyosarcoma of bone: report of 4 cases. J Comput Assist Tomogr 2005;29:254-9. [Crossref] [PubMed]
- Miura K. Primary leiomyosarcoma with the invasion into intertrabecular space of bone: a case report. Clin Imaging 2001;25:209-14. [Crossref] [PubMed]
- Klimo P Jr, Schmidt MH. Surgical Management of Spinal Metases. The Oncologist 2004;9:188-96. [Crossref] [PubMed]
- Stener B. Total spondylectomy in chondrosarcoma arising from the seventh thoracic vertebra. J Bone Joint Surg Br 1971;53:288-95. [PubMed]
- Tomita K, Kawahara N, Baba H, et al. Total en bloc spondylectomy for solitary spinal metastases. Int Orthop 1994;18:291-8. [Crossref] [PubMed]
- Tomita K, Kawahara N, Murakami H, et al. Total En Bloc Spondylectomy for Spinal Tumors: Improvement of the Technique and Its Associated Basic Background. J Orthop Sci 2006;11:3-12. [Crossref] [PubMed]
- Tomita K, Kawahara N, Murakami H. Primary and Metastatic Tumors of the Spine: Total En Bloc Spondylectomy. Operative Techniques in Orthopaedic Surgical Oncology. Second edition. Springer, 2016:1-9.
- Chanplakorn P, Chanplakorn N, et al. Recurrent epithelioid sarcoma in the thoracic spine successfully treated with multilevel total en bloc spondylectomy. Eur Spine J 2011;20:S302-S308. [Crossref] [PubMed]
- Tomita K, Kawahara N, Baba H, et al. Total en bloc spondylectomy. A new surgical technique for malignant vertebral tumors. Spine (Phila Pa 1976) 1997;22:324-33. [Crossref] [PubMed]
- Gardner LU. A Case of Metastatic Leiomyosarcoma Primary in the Uterus. J Med Res 1917;36:19-30. [PubMed]
- Lo TH, van Rooij WJ, Teepen JL, et al. Primary leiomyosarcoma of the spine. Neuroradiology 1995;37:465-7. [Crossref] [PubMed]
- Antonescu CR, Erlandson RA, Huvos AG. Primary leiomyosarcoma of bone: a clinicopathologic, immunohistochemical, and ultrastructural study of 33 patients and a literature review. Am J Surg Pathol 1997;21:1281-94. [Crossref] [PubMed]
- Ochiai H, Yamakawa Y, Fukushima T, et al. Primary leiomyosarcoma of the cervical spine causing spontaneous compression fracture: report of an autopsy case. Neuropathology 2000;20:60-4. [Crossref] [PubMed]
- Ritter AM, Amaker BH, Graham RS, et al. Central nervous system leiomyosarcoma in patients with acquired immunodeficiency syndrome. Report of two cases. J Neurosurg 2000;92:688-92. [Crossref] [PubMed]
- Nishida J, Kato S, Shiraishi H, et al. Leiomyosarcoma of the lumbar spine: case report. Spine 2002;27:E42-6. [Crossref] [PubMed]
- Sasaguri T, Tanimoto A, Kimura S, et al. Primary leiomyosarcoma of the vertebra: case report and review of the literature. Pathol Int 2004;54:73-6. [Crossref] [PubMed]
- Dohi O, Hatori M, Ohtani H, et al. Leiomyosarcoma of the sacral bone in a patient with a past history of resection of uterine leiomyoma. Ups J Med Sci 2003;108:213-20. [Crossref] [PubMed]
- Ganau S, Tomas X, Mallofre C, et al. Leiomyosarcoma of sacrum: imaging and histopathologic findings. Eur Radiol 2002;12:S35-9. [PubMed]
- Potsi M, Stavrinou P, Patsinakidis N, et al. Primary osseous leiomyosarcoma of the spine: a rare entity—case report and review of the literature. J Neurol Surg A Cent Eur Neurosurg 2012;73:238-42. [Crossref] [PubMed]
- Sucu HK, Bezircioglu H, Rezanko T. Partial spondylectomy for primary leiomyosarcoma of C2 vertebra. Spine 2011;36:E1422-6. [Crossref] [PubMed]
- Tahara K, Yamashita K, Hiwatashi A, et al. MR imaging findings of a leiomyosarcoma of the thoracic spine: a case report. Clin Neuroradiol 2016;26:229-33. [Crossref] [PubMed]
- Yang Y, Ma L, Li L, et al. Primary leiomyosarcoma of the spine. A case report and literature review. Medicine (Baltimore) 2017;96:e6227. [Crossref] [PubMed]
- Gladdy RA, Qin LX, Moraco N, et al. Predictors of survival and recurrence in primary leiomyosarcoma. Ann Surg Oncol 2013;20:1851-7. [Crossref] [PubMed]