Use of 3D printer model to study vertebral artery anatomy and variations in developmental craniovertebral junction anomalies and as a preoperative tool—an institutional experience
Introduction
The craniovertebral complex comprises of two sets of joints-occipitoatlantal and atlantoaxial joints. Occipitoatlantal joint is more stable but less mobile while atlantoaxial joint offers more mobility. Due to more mobility, there are more chances of injury and dislocation (1). The surgical management of atlantoaxial dislocation (AAD) mostly consists of posterior approaches. Spinal instrumentation using rods and screws have become procedure of choice for posterior fixation. There is 4.1% risk of vertebral artery injury during craniovertebral junction (CVJ) surgery (2,3). Vertebral artery anatomy is highly variable in this region posing challenges during surgery. There have been a few cadaveric studies on vertebral artery anatomy in this region (4,5). Our study used a 3D printer model to understand the anatomy and variations in vertebral artery in live patients thereby providing an accurate idea about vertebral artery injury risk in these patients preoperatively and to rehearse the whole procedure.
Methods
Ten patients of developmental CVJ anomalies who were planned for operative intervention in the Department of Neurosurgery at SMS Hospital from February 2016 to December 2016 were analysed using a 3D printer model. An ethical clearance was obtained for the study by local ethical committee of the institute.
Inclusion criteria
Patients with developmental CVJ anomalies undergoing surgical intervention.
Exclusion criteria
Patients having CVJ deformity due to causes other than developmental like traumatic, infections.
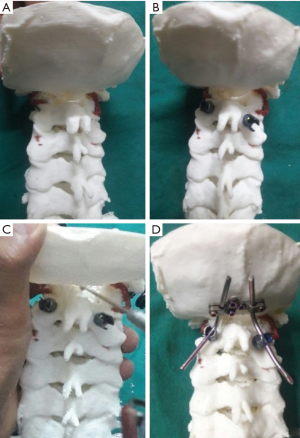
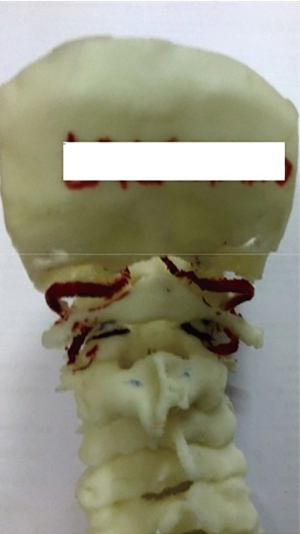
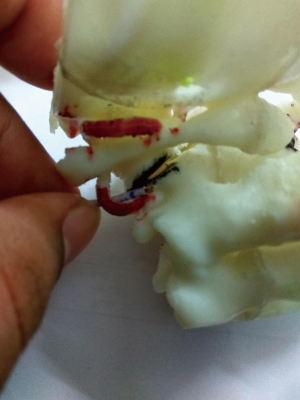
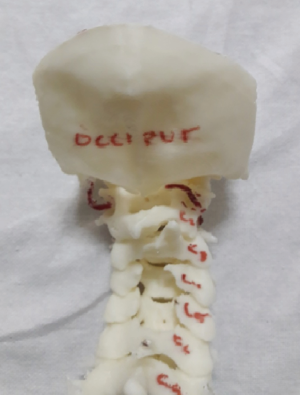
All these patients underwent non-contrast 3 Tesla MRI CVJ and cervical spine. If clinical features and MRI were indicative of any bony CVJ anomaly, then CT scan CVJ with flexion, extension and neutral view was done using Philips 128 slice CT scan. Accordingly a diagnosis of AAD with or without BI (basilar invagination) was made. All patients underwent 3 dimensional CT angiography head and neck by injecting contrast at the rate of 4.5 mL/sec. CT Angiography of these patients was used to extract the three dimensional file in STL (surface tessellation language) format. This STL file was sent to 3 D printer station for printing of 3D model. The models were made using acrylonitrile butadiene styrene (ABS) polymer by a fused dependent modelling (FDM) printer (Figure 1). This printer uses beads of heated plastic which are released from the print head as it moves forming the tissue replica in thin layers. We made 3D printer models of all ten patients and studied vertebral artery anatomy and its relation to C1–C2 facets and joints. The course of vertebral artery after its exit from C2 transverse foramina to its entry in cranium was studied. Any gross asymmetry in two vertebral arteries with presence of hypoplasia or aplasia was noted. Also, various bony abnormalities like occipitalisation of C1, C2–C3 fusion were noted. We studied the morphology of atlantoaxial joints and marked the length of atlantoaxial joint dorsally and the distances of medial most part of vertebral artery with lateral most part of joint. The posterior part of atlantoaxial joint was marked with a black marker and vertebral artery was marked with red marker. A malleable wire with markings in mms was used to measure the distance of vertebral artery from the joint (Figure 2). According to the course of vertebral artery in relation to the joint, the vertebral artery course was classified as being outside, in lateral third, middle third or medial third of the joint. These printer models were able to give an in vivo picture of vertebral arteries in patients and morphology of facetal joints. Accordingly appropriate fixation procedure was planned and preoperative rehearsal of procedure was done.
Results
We studied 10 patients (9 male and 1 female patient) of developmental CVJ anomaly with their age ranging from 13 to 55 years (Table 1). Eight out of ten patients in the series were having AAD with BI while two patients were having AAD only. Nine out of ten patients were having occipitalised atlas, one having C2–C3 fusion and four of them having scoliosis or tilt of cervical spine. Out of twenty vertebral arteries studied in ten patients, two were hypoplastic and out of these one couldn’t be appreciated on 3D printer model. Out of remaining nineteen, thirteen arteries were found to lie outside the joint, three were in lateral third, one traversed the middle third of joint and one lied in medial third. In one patient, due to severe scoliosis, the vertebral artery was stretched and it traversed horizontally over the joint. Also the course of vertebral arteries along with its entry into cranium was studied. Out of nineteen arteries studied, six arteries formed an abnormal medial stretching or loop posing an increased risk of vertebral artery injury during fixation (Figure 3). Out of ten patients studied, nine were having occipitalised atlas and so entry of these vertebral arteries into cranium were classified as given by Wang et al. (6) into four types. Seven of these patients were having entry through separate osseous foramina (type 3) while in one patient vertebral artery was below the occipitalised C1 lateral mass and enters the foramen magnum (type 1). In the patient with non occipitalised atlas, both vertebral arteries entry into cranium was normal through foramen magnum while in one patient vertebral artery was not appreciated on one side.

Full table
Discussion
CVJ anatomy is complex and consists of various osseous, ligamentous, neural and vascular structures compatible for life. Therefore, surgery in this region demands extra precautions and expertise. Now days, the surgical approaches for CVJ anomalies have changed from sublaminar wiring to posterior spinal instrumentation using screws and rods. These methods achieve greater stability and better fusion but involve greater risk of injuring vertebral arteries. Preoperative knowledge of patient’s individualised anatomy, therefore, helps in planning of suitable operative procedure and minimizing these injuries.
Printer model on the basis of 3D CT Angiography replicates the real anatomy of the patient and thus is of immense help in preoperative planning and rehearsal. Our study is the first study of its type in an institutional set up in our knowledge using 3D printer model to study various osseous and vertebral artery anomalies in these preoperative patients and using it in preoperative rehearsal of screw placement in these models mimicking the actual patients in operation theatre. Preparation of three dimensional printer models involve three steps-Image acquisition, Image post-processing and 3D printing (7). Imaging data acquisition can be done by any of imaging modalities including USG, CT scan and MRI but irrespective of imaging modality, images are stored in DICOM (Digital Imaging and Communications in Medicine) format. These DICOM images are then converted into STL (Surface Tessellation Language) file format using computer aided design (CAD) software and various post processing tools. Now this STL file is used by the 3D printer station for 3D printing. 3D printing may be rapid prototyping, solid free form or layered manufacturing on the basis of production method used. The principle of rapid prototyping is to use 3D computer models for the reconstruction of a 3D physical model by the addition of material layers (7). There are a number of rapid prototyping techniques which include stereolithography, selective laser sintering (SLS), Fused Deposition Modelling (FDM), Laminated Object Manufacturing (LOM), Inkjet printing techniques. In Fused Deposition Modelling technique, which was used by us, small beads of heated thermoplastic material which immediately attaches to layer below to form a three dimensional model. It is cost effective but has low speed. Various coloured materials can also be used mimicking various structures such as red for arteries and blue for veins.
In our study of ten patients, nine were having an occipitalised atlas (90%). In normal population, occipitalisation of atlas was seen in 0.1–0.8% of population (8) while it is significantly higher in patients with AAD (9-11). In study conducted by Sardhara et al. (12), occipitalisation of atlas was found in 72% of patients which was 90% in our study. Occipitalisation of atlas and C2–C3 fusion is often associated with lateral joint asymmetry due to their common embryological development (12). This leads to facetal instability and consequent AAD (13).
There have been previous studies on vertebral artery anomalies in this subset of patients on the basis of CT angiography and in normal patients on cadaver but most of these have not described the distance of vertebral artery from C1–C2 joint which is one of the most important parameter in screw placement. Also CT angiography gives an idea about the anatomy but 3D printer model is like providing actual anatomy in hand for practice. The use of 3D-printer models for surgical training is also better than training on cadavers, which are less available and costly. Cadavers also don’t have predefined pathology and are better for anatomical training rather than surgical training. Out of nineteen arteries, we were able to study, thirteen arteries were found to lie outside the joint, three were in lateral third, one in the middle third of joint and one lied in medial third. In one patient, due to severe scoliosis, the vertebral artery was stretched and it traversed horizontally all over the joint. Six out of nineteen arteries formed an abnormal medial stretching or loop. Those arteries crossing the articular surfaces especially in lateral and medial thirds have to be dissected carefully and gently retracted superiorly or inferiorly making place for screw insertion. Also monopolar cautery should be cautiously used in these patients in this region and better not to use. Two out of twenty arteries (10%) in our series were found to be hypoplastic and these deserve a special mention as the side of hypoplastic artery has to be dissected first and its joint should be opened first as it helps in opening the joint on the opposite side and makes dissection on opposite side easier and thus decrease the chances of dominant vertebral artery injury.
Regarding entry of vertebral artery into cranial cavity, Wang et al. (6) classified it into four types. Type I is below the occipitalised C1 lateral mass (8.3%), in Type II, it travels on the posterior surface or makes a curve on it (25%); in Type III (the most common variety; 61.1%), it enters an osseous foramen created between the fused atlas and occipital bone; and in type IV, there is absence of vertebral artery. In our series, one patient was having non occipitalised atlas and normal entry through foramen magnum. In remaining nine patients, seven patients were having type III entry (77.7%), one patient was having type I entry (11.11%) and remaining one patient was having type IV entry (11.11%).
By our study, 3D printer model was extremely helpful in terms of analyzing joints and vertebral artery preoperatively and making the surgeon acquainted about the placement and trajectory of the screws in particular patient by practising it on printer model preoperatively (Figure 4), thus minimizing the chances of vertebral artery injury. It gives a clear idea about size, course, dominance and anomalies of vertebral artery along with bony abnormalities in this region. These models were also useful in preoperative selection of screws, their sizes and trajectory. These models were also helpful in studying joint morphology and facetal alignment and any tilt or rotation which helps in deciding accessibility of joints. This along with the dominance of vertebral artery in turn decides the side to be dissected first. Preferably the joint with easy accessibility and non-dominant vertebral artery should be dissected first and opened .Also, position of vertebral artery in relation to the joint gives an idea about the manoeuvre required to access the joint. Further size of pedicles, lateral masses and lamina can be preoperatively assessed and appropriate type of fixation procedure can be planned. Although CT Angiography also delivers similar piece of knowledge but it doesn’t give that graspable three dimensional objects for hands on.
Our study has few limitations. Being in a government set up catering a large number of poor patients, cost remains a major factor although we used cheaper fused dependent modelling technique. But this technique limits clarity as compared to SLS which is must costlier and involves colour imparting to various structures like red for arteries and blue for veins. Secondly, these models are fragile and utmost care is to be taken to handle them. Also small vessels are sometimes not formed in this technique as it involves deposition of small beads one upon another in three dimensional space and it is difficult for these tiny particles to stack one upon another against gravity. Hypoplastic vessels are sometimes not seen as in our case. But these problems can also be addressed by other advanced techniques. Venous and nervous anatomy is not visualised in our models. Also the stretchability and suppleness of joints cannot be assessed and amount of distraction required cannot be judged preoperatively.
Conclusions
3D printer model is an invaluable tool for complex CVJ surgeries which provides an excellent opportunity to study vertebral artery relationship to C1–C2 joint, facetal morphology and joint structure and utilizes this study to practice the actual procedure preoperatively with appropriate screws thereby reducing the chances of vertebral artery injury. Also it can be a perfect teaching and learning material for training surgeons. In our opinion, these models should be included as a basic investigation tool in this subset of patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: An ethical clearance was obtained for the study by local ethical committee of the institute (Office of the ethics committee SMS Medical College and attached hospitals Jaipur vide letter no. – 2693/MCEC/2016).
References
- White AA 3rd, Panjabi MM. The clinical biomechanics of the occipitoatlantoaxial complex. Orthop Clin North Am 1978;9:867-78. [PubMed]
- Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg 1998;88:634-40. [Crossref] [PubMed]
- Yamazaki M, Okawa A, Furuya T, et al. Anomalous vertebral arteries in the extra- and intraosseous regions of the craniovertebral junction visualized by 3-dimensional computed tomographic angiography: analysis of 100 consecutive surgical cases and review of the literature. Spine (Phila Pa 1976) 2012;37:E1389-97. [Crossref] [PubMed]
- Cacciola F, Phalke U, Goel A. Vertebral artery in relationship to C1-C2 vertebrae: an anatomical study. Neurol India 2004;52:178-84. [PubMed]
- Muralimohan S, Pande A, Vasudevan MC, et al. Suboccipital segment of the vertebral artery: a cadaveric study. Neurol India 2009;57:447-52. [Crossref] [PubMed]
- Wang S, Wang C, Liu Y, et al. Anomalous vertebral artery in craniovertebral junction with occipitalization of the atlas. Spine (Phila Pa 1976) 2009;34:2838-42. [Crossref] [PubMed]
- Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 2010;5:335-41. [Crossref] [PubMed]
- Lang J. Craniocervical region, osteology and articulations. Neurol Orthop 1986;1:67-92.
- Jain VK, Behari S. Management of congenital atlanto-axial dislocation: somelessons learnt. Neurol India 2002;50:386-97. [PubMed]
- Jain VK, Behari S, Banerji D, et al. Transoral decompression for craniovertebral osseous anomalies: perioperative management dilemmas. Neurol India. 1999;47:188-95. [PubMed]
- Behari S, Kiran Kumar MV, Banerji D, et al. Atlantoaxial dislocation associated with the maldevelopment of the posterior neural arch of axis causing compressive myelopathy. Neurol India 2004;52:489-91. [PubMed]
- Sardhara J, Behari S, Mohan BM, et al. Risk stratification of vertebral artery vulnerability during surgery for congenital atlanto-axial dislocation with or without an occipitalized atlas. Neurol India 2015;63:382-91. [Crossref] [PubMed]
- Goel A. Goel's classification of atlantoaxial "facetal" dislocation. J Craniovertebr Junction Spine 2014;5:3-8. [Crossref] [PubMed]