Anterior lumbar interbody fusion (ALIF) as an option for recurrent disc herniations: a systematic review and meta-analysis
Introduction
Recurrent intervertebral disc herniation is a specific pathological entity which may occur in patients who have undergone a primary discectomy for lumbar intervertebral disc herniation (1-3). It occurs when there is a return of radicular pain symptoms after a pain-free interval following a disc herniation which has been surgically treated with a discectomy. To further define this phenomenon, Swartz et al. recommends that a clinically relevant definition does not restrict the pain-free period to a particular minimum postoperative time-frame (2). They further suggest that only ipsilateral disc herniation be included in the definition, hence excluding contralateral disc bulging with signs and symptomatology (2).
Risk factors for the development of recurrent disc herniation are generally classed into structural, patient or operative technique related. Patient factors include obesity, smoking, male gender, diabetes, weight lifting, young age, traumatic events and manual labour employment, which can all increase the likelihood of developing recurrent disc herniation (4-7). Structural factors largely involve the specific morphology of the annular tear or disc fragment. Annular prolapses without a sub-annular fragmentation are the most prone to recurrence when compared to a disc fragmentation and a small annular defect, a large disc fragmentation with a large posterior annular tear or fragment-contained discs with incomplete or no annular tears (8). Evidence from the literature also supports the impact of the invasiveness of discectomy on the rate of recurrence; with conservative discectomies such as a sequestrectomy (removal of extruded fragment only), prone to recurrent disc herniation when compared to an initially aggressive discectomy, with significant removal of disc nucleus (9).
Indications for an initial discectomy procedure include; persistent, recurrent or progressive radicular pain, which has failed to respond to conservative management and new or progressive neurological deficits observed clinically or with an electromyelogram. Additional indications include cauda equina syndrome, with bowel and bladder dysfunction (10). In contrast, indications for recurrent disc herniation discectomy surgeries are less well-defined. As revision surgery is more complicated, holding slightly worse patient outcomes and higher rates of complications including dural tears and nerve injury (11-13). Currently, an additional micro-discectomy procedure is the most common surgical intervention pursued for recurrent disc herniations, however primary fusion surgery has been practised with potential indications such as lumbar instability or severe axial lower back pain.
An anterior approach for discectomy and fusion may offer an alternative option for patients who suffer from recurrent lumbar disc herniation. As for anterior lumbar interbody fusion (ALIF) used in the context of degenerative disc disease (14-20), the anterior approach theoretically allows for a comprehensive discectomy, less paraspinal muscle trauma and less nerve trauma from spinal nerve retraction. Specifically for recurrent disc herniations, a repeat posterior approach may result in higher risks of dural tears, more posterior bone removal to access the disc space, and an access corridor that may be impeded by residual tissue or epidural fibrosis. These complications can potentially be avoided via an anterior approach. However, the ALIF approach is not without its own risks. These include vascular injury and retrograde ejaculation. In the current study, we assessed the available evidence of outcomes when pursuing ALIF for recurrent disc herniation through a systematic review and meta-analysis of the literature.
Methods
Purpose
To assess the viability of ALIF as a surgical treatment for recurrent disc herniations through the use of a systematic review and meta-analysis of the literature, following recommended guidelines (21,22).
Search strategy and study selection
Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club, and Database of Abstracts of Review of Effectiveness (DARE) from their dates of inception to May 2017. To achieve the maximum sensitivity of the search strategy, we combined the terms: “disc herniation”, “anterior lumbar interbody fusion”, “ALIF”, “anterior approach” as either key words or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies, assessed using the inclusion and exclusion criteria.
Eligible studies for the present systematic review and meta-analysis included those in which patient cohorts underwent an ALIF procedure using either integrated stand-alone cages or cages with supplemental posterior pedicle screw fixation. Studies that did not include complications as endpoints were excluded. When institutions published duplicate studies with accumulating numbers of patients or increased lengths of follow-up, only the most complete reports were included for quantitative assessment at each time interval. All publications were limited to those involving human subjects. Abstracts, case reports, conference presentations, editorials, reviews and expert opinions were excluded.
Data extraction, critical appraisal and treatment effect
All data were extracted from article texts, tables and figures. Two investigators independently reviewed each retrieved article (K Phan, A Lackey). Discrepancies between the two reviewers were resolved by discussion and consensus. If the study provided medians and interquartile ranges instead of means and SDs, we imputed the means and SDs as described by Hozo et al. (23). Since quality scoring is controversial in meta-analyses of observational studies, two reviewers (K Phan, A Lackey) independently appraised each article included in our analysis according to a critical review checklist of the Dutch Cochrane Centre proposed by MOOSE (24). The key points of this checklist include: (I) clear definition of study population; (II) clear definition of outcomes and outcome assessment; (III) independent assessment of outcome parameters; (IV) sufficient duration of follow-up; (V) no selective loss during follow-up; and (VI) important confounders and prognostic factors identified.
Statistical analysis
A meta-analysis of proportions was conducted for the available main perioperative and postoperative variables. Firstly, to establish variance of raw proportions, a Freeman-Tukey transformation was applied (25). To incorporate heterogeneity (anticipated among the included studies), transformed proportions were combined using DerSimonian-Laird random effects models (26). Finally, the pooled estimates were back-transformed. Heterogeneity was evaluated using Cochran Q and I2 test. Weighted means were calculated by determining the total number of events divided by total sample size. Weighted Pearson’s coefficient (rs) was used to calculate correlation coefficients for meta-regression analysis of outcomes based on midpoint of study periods. All analyses were performed using the metafor package for R version 3.01. P<0.05 were considered statistically significant.
Results
Quality of studies
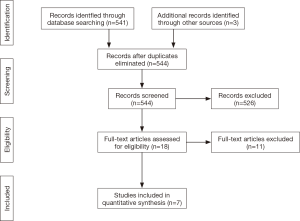
A total of 541 studies were identified through six electronic database searches and from other sources such as reference lists (Figure 1). After exclusion of duplicate or irrelevant references, 18 potentially relevant articles were retrieved. After detailed evaluation of these articles, 7 studies remained for assessment, including a total of 181 patients undergoing ALIF for treatment of recurrent disc herniations (27-33). All of the included 7 studies were observational and retrospective studies (Table 1). Only four studies reported mean follow-up equal of greater than 24 months (27-29,33). One study did not report follow-up duration (30). The mean time interval from previous surgery was only reported in three studies (27,29,32).

Full table
Patients’ characteristics
Overall, 40% of patients were male, with a weighted mean age of 52.7 (range, 29.5–59.5) years. All patients had been diagnosed with recurrent lumbar disc herniations. Baselines characteristics such as height, weight, smoker status and any additional co-morbidities were not reported.
Perioperative outcomes
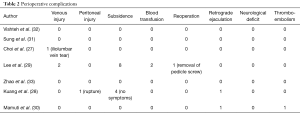
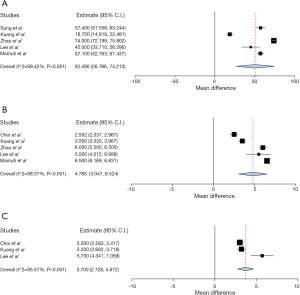
Perioperative outcomes from the seven studies the overall range of perioperative complications was 0.079% (95% CI, 0.021–0.137%; I2=62.58%; P=0.014) (Figure 2A). Three studies reported no perioperative complications (31-33), two studies reported only one or two (27,30), while six or more complications were reported in the other two studies (28,29). Subsidence was the most frequently reported complication. These complications are summarised in Table 2. Average total blood loss was 122 mL (95% CI, 88.7–155.2 mL; I2=95.14%; P<0.001) (Figure 2B). Average operative duration was 89 minutes (95% CI, 64.8–113.1 minutes; I2=97.85%; P<0.001) (Figure 2C). Average hospital stays were 5.3 days (95% CI, 4.0–6.5 days; I2=93.04%, P<0.001) (Figure 2D).

Full table
Clinical outcomes
From the 7 studies, the average improvement in Oswestry Disability Index (ODI) scores was 50.5 (95% CI, 26.8–74.2; I2=99.42%, P<0.001) (Figure 3A). Average improvement in Visual Analogue Scale (VAS) back pain scores was 4.8 (95% CI, 3.05–6.5; I2=98.37%; P<0.001) (Figure 3B). Average improvement in VAS leg pain scores was 3.7 (95% CI, 2.7–4.6; I2=85.57%; P<0.001) (Figure 3C).
Discussion
There is currently no gold standard treatment for operative management of recurrent lumbar disc herniations (4,5,34-37). Generally the first-line treatment is an additional discectomy surgery without fusion. There is however growing evidence that fusion is efficacious in reducing dysfunction and pain in severe axial back pain, specifically when sacral tilt, and lumbar lordosis, is restored (29), although the approach remains a topic of ongoing debate. In a large scale survey across 2,560 American spinal surgeons, there was a general trend for more experienced surgeons, defined as performing greater than 200 cases a year, to include a fusion as opposed to a standalone repeat discectomy procedure in comparison to those performing <100 cases (38).
In a review by Drazin et al., transforaminal lumbar interbody fusion (TLIF) was suggested to be the most efficacious fusion option when compared to posterolateral fusion (PLF) and posterior lumbar interbody fusion (PLIF), finding a mean VAS pain improvement of 54–86.5% (4). However, Drazin et al. (5) did not asses ALIF as a fusion option (4). Additionally Dower et al.’s review reported that following treatment of recurrent disc herniation by discectomy and fusion, VAS leg pain score improved by 44.9, VAS back pain scores improved by 47.1 and ODI scores improved by 41.2 (in 100 point scores).
To our knowledge, the present study is the first meta-analysis of pooled outcomes using an ALIF approach for recurrent disc herniations. In terms of surgical parameters, an acceptable total blood loss rate of 122 mL, average operative duration of 89 min and hospital stay of 5 days was achieved. Similarly to Dower et al. (5), We demonstrated significant improvements in VAS leg pain score, back pain score and ODI scores with an ALIF approach for recurrent disc herniations.
ALIF has several theoretical and observable advantages to other fusion approaches. This includes less injury to paraspinal muscle which results in less postoperative pain and blood loss during surgery. An anterior approach would avoid the need to dissect scar tissue produced as a result of the primary discectomy surgery and also concurrently reduce epidural bleeding. A repeat posterior microdiscectomy approach may require increased posterior bony resection or dissection around scar tissue in order to safely access the herniated discs. Further advantages come from ALIF reducing the need for nerve root retraction, hence limiting nerve irritation, and its ability to allow for a more complete discectomy with greater exposure of the disc space, reducing recurrent disc rates. Moreover, anterior access to the lumbar spine allows for larger cages to be inserted with wider contact areas, allowing for correction of the lordotic curvature of the lumbar spine and the pursuit of an increased sacral tilt. This is significant as Lee et al. found it to be significantly associated with outcomes postoperatively (29).
There are however some associated complications and disadvantages. The most commonly reported is injury to the associated vasculature, with other complications including, ureteral avulsion, retrograde ejaculation resulting from hypogastric plexus injury, and dural leaks which are more challenging to repair in an anterior approach. Additionally reported are retroperitoneal haematoma (39), ileus, sympathetic dysfunction, pancreatitis, bowel injury (40), lateral femoral cutaneous nerve injury (41). and retroperitoneal fibrosis (42). In some instances, the herniated disc fragment may migrate beyond the disc space, and the anterior approach may be inadequate in visualization and retrieval of the disc fragment. Furthermore, an anterior approach necessitates a fusion procedure and thus longer follow-up to assess fusion status and risks of adjacent segment disease, whereas posterior approaches can be performed without requiring fusion.
ALIF procedures should be approached with caution for patients with significant vessel calcification, abnormal aortic or vena cava anatomy, prior abdominal surgery or any potential adhesions or osteophytes in contact between the venous vascular structures and anterior spine. In these settings, mobilization of the major abdominal vessels is more difficult and can potentially be hazardous. Although compared with no access surgeon, the use of an access surgeon was associated with similar intraoperative complication rates, support from an access surgeon is recommended in cases wherein exposure may be difficult (17).
In the seven included studies, there are no direct comparisons made between discectomy and fusion and just discectomy for treatment of recurrent disc herniation. This demonstrated that we are still in the early stages of understanding the utility of fusion in recurrent disc herniation. It is therefore important that further prospective and retrospective studies directly compare fusion for recurrent disc herniation to repeat discectomy and to conservative management, so as to clarify whether symptoms such as severe axial discogenic back pain truly stand up as an indication for fusion surgery. It is interesting to note that two of the included studies (Kuang et al. and Lee et al.) were also observational studies that looked at ALIF but not specifically in recurrent disc herniation, but in revision lumbar surgery. This heterogeneity not only exists in the sample populations being analysed in this paper but also exists within the ALIF intervention itself which can be undertaken in a variety of ways, with or without the use of self-anchoring cages (28), percutaneous pedicle screw fixation (29) and the utilisation of the mini-open approach (28,30,33). Another limitation is that the correct diagnosis of recurrent disc herniation as well as the appropriate surgical treatment option is an ongoing challenge for surgeons and clinicians. There remains limited comparative data amongst surgical techniques for recurrent disc herniations.
Conclusions
Through a meta-analysis of the current literature, this study found ALIF to be a safe and feasible approach for the treatment of recurrent disc herniations. This was demonstrated through significant improvements in preoperative ODI and VAS back and leg pain scores, with minimal complications. The anterior approach may be appealing in particular scenarios where there is extensive scar tissue from the initial procedure requiring extensive bony resection or cases of lumbar instability.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Parker SL, Mendenhall SK, Godil SS, et al. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res 2015;473:1988-99. [Crossref] [PubMed]
- Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus 2003;15:E10. [Crossref] [PubMed]
- Lebow R, Adogwa O, Parker S, et al. Asymptomatic same-site recurrent disc herniation after lumbar discectomy: results of a prospective longitudinal study with 2-year serial imaging. Spine (Phila Pa 1976) 2011;36:2147-51. [Crossref] [PubMed]
- Drazin D, Ugiliweneza B, Al-Khouja L, et al. Treatment of recurrent disc herniation: a systematic review. Cureus 2016;8:e622. [PubMed]
- Dower A, Chatterji R, Swart A, et al. Surgical management of recurrent lumbar disc herniation and the role of fusion. J Clin Neurosci 2016;23:44-50. [Crossref] [PubMed]
- Simpson JM, Silveri CP, Balderston RA, et al. The results of operations on the lumbar spine in patients who have diabetes mellitus. J Bone Joint Surg Am 1993;75:1823-9. [Crossref] [PubMed]
- Suk KS, Lee HM, Moon SH, et al. Recurrent lumbar disc herniation: results of operative management. Spine (Phila Pa 1976) 2001;26:672-6. [Crossref] [PubMed]
- Carragee EJ, Han MY, Suen PW, et al. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am 2003;85-A:102-8. [Crossref] [PubMed]
- Watters WC 3rd, McGirt MJ. An evidence-based review of the literature on the consequences of conservative versus aggressive discectomy for the treatment of primary disc herniation with radiculopathy. Spine J 2009;9:240-57. [Crossref] [PubMed]
- Spengler DM, Freeman CW. Patient selection for lumbar discectomy. An objective approach. Spine (Phila Pa 1976) 1979;4:129-34. [Crossref] [PubMed]
- Burton CV, Kirkaldy-Willis WH, Yong-Hing K, et al. Causes of failure of surgery on the lumbar spine. Clin Orthop Relat Res 1981.191-9. [PubMed]
- Palma L, Carangelo B, Muzii VF, et al. Microsurgery for recurrent lumbar disk herniation at the same level and side: do patients fare worse? Experience with 95 consecutive cases. Surg Neurol 2008;70:619-21; discussion 621. [Crossref] [PubMed]
- Fager CA, Freidberg SR. Analysis of failures and poor results of lumbar spine surgery. Spine (Phila Pa 1976) 1980;5:87-94. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Thayaparan GK, et al. Anterior lumbar interbody fusion as a salvage technique for pseudarthrosis following posterior lumbar fusion surgery. Global Spine J 2016;6:14-20. [Crossref] [PubMed]
- Assem Y, Pelletier MH, Mobbs RJ, et al. Anterior lumbar interbody fusion integrated screw cages: intrinsic load generation, subsidence, and torsional stability. Orthop Surg 2017;9:191-7. [Crossref] [PubMed]
- Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion--systematic review and meta-analysis. Br J Neurosurg 2015;29:705-11. [Crossref] [PubMed]
- Phan K, Xu J, Scherman DB, et al. Anterior lumbar interbody fusion with and without an "access surgeon": a systematic review and meta-analysis. Spine (Phila Pa 1976) 2017;42:E592-E601. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Daly D, et al. Approach-related complications of anterior lumbar interbody fusion: results of a combined spine and vascular surgical team. Global Spine J 2016;6:147-54. [Crossref] [PubMed]
- Phan K, Davies S, Rao PJ, et al. Worker's compensation status and outcomes following anterior lumbar interbody fusion (ALIF): prospective observational study. World Neurosurg 2017;103:680-5. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [PubMed]
- Phan K, Mobbs RJ. Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg 2015;1:19-27. [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [Crossref] [PubMed]
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13. [Crossref] [PubMed]
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 2000;283:2008-12. [Crossref] [PubMed]
- Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Statist 1950.607-11. [Crossref]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [Crossref] [PubMed]
- Choi JY, Choi YW, Sung KH. Anterior lumbar interbody fusion in patients with a previous discectomy: minimum 2-year follow-up. J Spinal Disord Tech 2005;18:347-52. [Crossref] [PubMed]
- Kuang L, Chen Y, Li L, et al. Applying the Mini-open anterolateral lumbar interbody fusion with self-anchored stand-alone polyetheretherketone cage in lumbar revision surgery. Biomed Res Int 2016;2016:1758352. [PubMed]
- Lee SH, Kang BU, Jeon SH, et al. Revision surgery of the lumbar spine: anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation. J Neurosurg Spine 2006;5:228-33. [Crossref] [PubMed]
- Mamuti M, Fan S, Liu J, et al. Mini-open anterior lumbar interbody fusion for recurrent lumbar disc herniation following posterior instrumentation. Spine (Phila Pa 1976) 2016;41:E1104-14. [Crossref] [PubMed]
- sung KHC, Jeong JY, Hyun HT, et al. Anterior lumbar interbody fusion for recurrent disc herniation. Korean J Spine 2004:237-42.
- Vishteh AG, Dickman CA. Anterior lumbar microdiscectomy and interbody fusion for the treatment of recurrent disc herniation. Neurosurgery 2001;48:334-7; discussion 338. [PubMed]
- Zhao F, Suyou L, Ni D, et al. Mini-open ALIF in the treatment of patients with recurrent lumbar disc herniation. Chin J Orthop 2014.34.
- Cinotti G, Roysam GS, Eisenstein SM, et al. Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br 1998;80:825-32. [Crossref] [PubMed]
- Ebeling U, Kalbarcyk H, Reulen HJ. Microsurgical reoperation following lumbar disc surgery. Timing, surgical findings, and outcome in 92 patients. J Neurosurg 1989;70:397-404. [Crossref] [PubMed]
- Eie N. Comparison of the results in patients operated upon for ruptured lumbar discs with and without spinal fusion. Acta Neurochir (Wien) 1978;41:107-13. [Crossref] [PubMed]
- Herron L. Recurrent lumbar disc herniation: results of repeat laminectomy and discectomy. J Spinal Disord 1994;7:161-6. [Crossref] [PubMed]
- Mroz TE, Lubelski D, Williams SK, et al. Differences in the surgical treatment of recurrent lumbar disc herniation among spine surgeons in the United States. Spine J 2014;14:2334-43. [Crossref] [PubMed]
- Sasso RC, Best NM, Mummaneni PV, et al. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976) 2005;30:670-4. [Crossref] [PubMed]
- Rajaraman V, Vingan R, Roth P, et al. Visceral and vascular complications resulting from anterior lumbar interbody fusion. J Neurosurg 1999;91:60-4. [PubMed]
- Saraph V, Lerch C, Walochnik N, et al. Comparison of conventional versus minimally invasive extraperitoneal approach for anterior lumbar interbody fusion. Eur Spine J 2004;13:425-31. [Crossref] [PubMed]
- Chan FL, Chow SP. Retroperitoneal fibrosis after anterior spinal fusion. Clin Radiol 1983;34:331-5. [Crossref] [PubMed]