Obstructed spinopelvic fixation in the setting of a triangular titanium sacroiliac fusion implant: a case description
Introduction
The differential diagnosis of lower back pain includes lumbar spine, hip, groin, gluteal, and sacroiliac (SI) pathology. The diagnosis of the SI joint as the primary pain generator is often difficult, but some studies have shown that up to 22.5% of referred nonspecific back pain can be localized to this region (1). As a result of multiple pain generators, SI joint pain may explain “failed back syndrome” or the lack of improvement observed in a subset of patients after lumbar spinal fusion. Surgical arthrodesis of the SI joint is an option when non-operative management fails to prove any significant relief of symptoms. Due to recent advancements in minimally invasive surgical (MIS) approaches, the prevalence of SI fusion procedures is increasing. To our knowledge, herein we report the first case of revision thoracolumbar fusion to the ilium obstructed by a percutaneously instrumented SI joint requiring burring to allow for placement of an iliac screw.
Case presentation
A 71-year-old female presented with a longstanding history of spinal deformity after multiple spinal surgeries. On initial presentation, she complained of 40% back pain and 60% right thigh pain as well as a disabling, pitched-forward posture. The patient was previously instrumented and fused posteriorly from T11 to L5. Additionally, she had undergone lateral interbody fusions at four contiguous lumbar levels and a cephalad kyphoplasty to prevent proximal junctional kyphosis (PJK). Subsequently, she underwent a right SI joint fusion with the Zimmer TriCor SI Joint Fusion System, made of titanium alloy with an outer surface of pure titanium.
On physical examination, she stood with a forward bent posture and overall kyphotic alignment. She had weakness of right extensor hallucis longus (EHL) (4-/5), but no other neurologic abnormalities were detected.
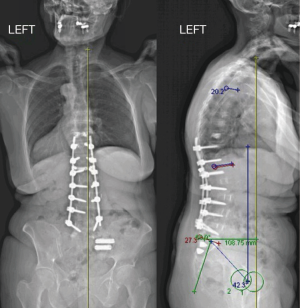
Diagnostic imaging revealed her prior thoracolumbar and SI joint instrumentation. Sagittal parameters measured: pelvic incidence (PI) of 61°, lumbar lordosis (LL) of 27°, thoracic kyphosis (TK) of 20°, and overall sagittal vertical axis (SVA) of +10.9 cm (Figure 1). She had significant segmental kyphosis about L5–S1, which was the focal aspect of her deformity. CT myelogram revealed a transitional lumbosacral vertebral body. Consistent with a Castellvi IIa pseudoarticulation, there was an anomalous pseudoarticulation of the right L5 transverse process with the sacrum leading to degenerative change and narrowing of the distal course of the L5 ventral nerve root.
After failing to improve with conservative treatment modalities, the patient was scheduled for a staged operative intervention. In the first stage, a 16 mm oblique lateral interbody fusion (OLIF) implant with 24° lordosis was placed at L5–S1. After optimal positioning was confirmed by fluoroscopy, a plate was placed over the ventral aspect of L5–S1 to prevent graft migration. The patient was then flipped prone and approached posteriorly. All instrumentation was removed and in order to regain segmental lordosis at L5–S1, a posterior column osteotomy was performed with removal of the posterior ligamentous complex, which included complete facetectomies. A laminectomy and right foraminotomy was performed at L5 to free the nerve root from the vertebrae’s pseudoarticular impingement. A third rod was placed across the osteotomy site for additional stability.
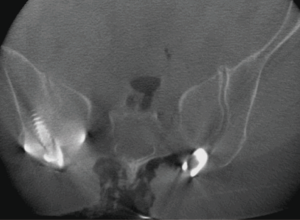
Attention was then turned to instrumentation of the sacrum and pelvis. Upon attempted placement of the right S2-alar-iliac (S2AI) screw, the gearshift was met with metallic resistance. Subsequently, a standard iliac screw was attempted. Fluoroscopy revealed obstruction of the path of the S2AI screw, as well as standard iliac screw, secondary to the SI joint implant. Circumventing the need from implant removal, a diamond burr was used to burr a hole through the metal SI joint “plug” to facilitate passage of the gear shift to probe the ilium (Figure 2). Concurrent irrigation and suctioning prevented excessive metal debris from contaminating the surrounding tissues.
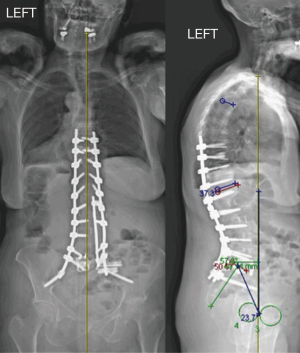
A 8.5 mm × 80 mm screw was then placed through the hole created through the SI joint plug into the ilium under direct visualization. The screw obtained good purchase and allowed for stable deformity correction. All remaining metal debris was thoroughly irrigated from the wound. Although there is concern for metal corrosion, the risk is minimized because both the pelvic screw and SI implant are of titanium alloy. Every level was subsequently instrumented up to T9, and fusion was performed. Postoperative imaging revealed markedly improved LL resulting in restoration of sagittal balance (Figure 3). The patient has had 2-year follow-up at this point, and is well-functioning without evidence of pseudoarthrosis or systemic metal ion toxicity.
Discussion and conclusions
Spinopelvic fixation plays a critical role in the success of lumbosacral fusion and spinal deformity surgery. Achieving fusion at the lumbosacral junction is challenging for a variety of reasons, including high biomechanical forces and poor sacral bone quality. Studies have demonstrated high pseudoarthrosis rates for long fusions to S1 (2). Extension of a thoracolumbar fusion to the pelvis in adult deformity patients results in greater multi-planar correction, more stability of the construct, and better overall success of lumbosacral fusion (3).
Multiple instrumentation techniques have been developed for spinopelvic fixation, including the Galveston technique, iliac screws, and most recently, S2AI screws (4). The S2AI screw is appealing for several reasons. It has decreased implant prominence, as the screws start 15 mm deeper than traditional iliac screws (5). In addition, the S2AI trajectory allows the screw head to sit in line with the S1 screws, decreasing the need for additional connectors, thereby decreasing surgical complexity. S2AI screws have been shown to be equally biomechanically stable as iliac screws in all loading modes (6). It is the preference of the senior author to use S2AI screws for lumbopelvic fixation, when feasible. However, placement of iliac screws or S2AI screws can be challenging in the setting of SI arthrodesis implants.
Open arthrodesis of the SI joint was the gold standard of surgical management for SI joint pain throughout the 20th century. However, open arthrodesis was wrought with complications and required extensive soft tissue dissection. MIS SI fusion has been shown to successfully improve pain, function and satisfaction, while maintaining a low perioperative complication rate. In a recent meta-analysis of open and MIS techniques, the surgical revision rate for SI joint arthrodesis was reported at only 2.1% (7). As the prevalence of MIS SI fusion increases, the spinal deformity surgeon will likely be faced with addressing a SI fusion bolt obstructing the path of an iliac or S2AI screw.
Although the indication for the original MIS SI fusion in our case was unknown, we can speculate that the patient’s sagittal imbalance and deformity was inadvertently overlooked. Prior to indicating implantation for SI fusion, it is imperative for all surgeons to understand and recognize the implications of sagittal imbalance, especially in the patient with failed back syndrome. Unfortunately, there is little discussion in the literature regarding obstructed lumbopelvic fixation in the setting of such implants.
Our patient presented with positive sagittal decompensation after thoracolumbar fusion as a result of distal junctional kyphosis at L5–S1. Our choice of a staged reconstruction involving direct lateral and traditional posterior approaches was based on the need to regain significant, segmental lordosis at L5–S1. In the first stage alone, 24° of segmental lordosis was regained through the interbody spacer. Subsequently, a posterior column osteotomy allowed for further sagittal correction. Given the extensive proximal fusion mass acting as a fulcrum at L5–S1, fixation was extended to the pelvis. Previous studies have shown that the incidence of pseudoarthrosis at L5–S1 level increases with the number of proximal fusion levels and positive sagittal balance (2,8). In these settings, fixation to the ilium is a viable option for augmenting biomechanical fixation and decreasing stress across lumbosacral instrumentation.
Upon instrumentation of the right S2AI screw, we encountered obstruction with the previously placed SI joint implant. At this point in the case, there were a few options, including unilateral S2AI fixation, unilateral iliac wing fixation, redirecting the gear shift to a native pathway, or placing a short screw that ended at the SI implant. In order to obtain optimal, bilateral pelvic fixation, there were only two options: (I) a separate procedure for removal of the SI implants; or (II) burr a pathway through the SI implant. Because removal of the SI implants would subject the patient to a second incision, dissection, and associated complications, the decision was made to use a high-speed diamond burr to create a pathway through the SI implant and allow passage of the S2AI screw.
There are a few potential concerns with our technique. The practice of using a diamond burr for cannulation of a screw path through an SI implant may vary depending on the SI implant itself. In our case, the SI implant had a relatively trabecular outer surface that permitted high-speed burring with relative ease. It is possible that other SI fusion systems with denser implants may preclude such ease of this technique. Secondly, because the metal of the S2AI screw and the SI joint fusion instrumentation may be dissimilar, there is potential to create a “battery effect” or corrosive environment. Although not as profound as the effects in lower extremity arthroplasty, there have been reports of corrosion and wear in thoracolumbar posterior internal fixation retrieval studies that must be taken into account (9).
Herein, we report the first case of lumbopelvic fixation obstructed by a percutaneously instrumented SI joint. As the number of MIS SI fusion procedures increase, adult deformity cases requiring pelvic fixation in the setting of these implants will be more frequently encountered. We describe a technique using the high-speed diamond burr that allows for stable spinopelvic fixation in the setting of SI joint implants and obviates the morbidity associated with their removal.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 2008;21:579-84. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976) 2006;31:2329-36. [Crossref] [PubMed]
- Edwards CC 2nd, Bridwell KH, Patel A, et al. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976) 2004;29:1996-2005. [Crossref] [PubMed]
- Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976) 2010;35:2245-51. [Crossref] [PubMed]
- Chang TL, Sponseller PD, Kebaish KM, et al. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976) 2009;34:436-40. [Crossref] [PubMed]
- O'Brien JR, Yu W, Kaufman BE, et al. Biomechanical evaluation of S2 alar-iliac screws: effect of length and quad-cortical purchase as compared with iliac fixation. Spine (Phila Pa 1976) 2013;38:E1250-5. [Crossref] [PubMed]
- Heiney J, Capobianco R, Cher D. A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique. Int J Spine Surg 2015;9:40. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am 2006;88:721-8. [PubMed]
- Villarraga ML, Cripton PA, Teti SD, et al. Wear and corrosion in retrieved thoracolumbar posterior internal fixation. Spine (Phila Pa 1976) 2006;31:2454-62. [Crossref] [PubMed]