Percutaneous screw placement in the lumbar spine with a modified guidance technique based on 3D CT navigation system
Introduction
The pedicle screw (PS) fixation technique is widely used for stabilization in spine surgery. PS placement techniques can be further divided into open, minimally-open, and percutaneous techniques according to the exposed surgical field and incision length (1-5). According to the literature, there is a slight preference for percutaneous PS techniques versus open and minimally-open techniques due to reduced operative time, blood loss, and incision length as well as the optimal positioning of the screws with this procedure (6). The percutaneous placement of PS in the lumbar spine for various conditions, such as pars interarticularis defects (7), traumatic or osteoporotic vertebral fractures (8-11), restoration and/or preservation of lumbar lordosis during correction procedures for severe kyphoscoliosis (12,13), spondylolysis (14-16), spondylolisthesis (17,18), and finally to provide supplemental stabilization for lumbar interbody fusion procedures (19-22). Another relatively new indication for percutaneous PS placement is in obese patients with spinal deformities and severe degenerative lumbar disease as it reduces the operative site exposure, surgical time, and hospitalization and decreases the postoperative infection rate (23-25).
New technologies witnessed over the last decade have allowed for the development of several methods for percutaneous screw placement in the lumbar spine with increased safety and accuracy. The implantation of percutaneous PS can be assisted by several navigational techniques, such as fluoroscopic imaging obtained from one or two C-arms or 3D isocentric C-arms (26-35), imaging obtained intraoperatively by computed tomography (CT) integrated with navigational systems (29,36-39), and robotic techniques (6,19,40-49). Patients that are operated on with minimally invasive techniques have less hospitalization rates, less use of opioids, and less reports of adverse events in comparison to open techniques (6,31). The goals of these techniques are reduction of operative time, radiation exposure, PS malpositioning, and procedure-related complications (such as injuries to the nerve root, spinal cord, blood vessels, and viscera) (50-54). The objective of this study is to present a modified navigational guidance technique for PS placement in the lumbar spine with the use of cone-beam CT (iCBCT) and image-guided navigation system (IGNS) (O-arm Surgical Imaging System, Medtronic, Minneapolis, MN, USA). This technique was aimed at reducing surgical time during MIS lumbar spine procedures.
Methods
Study design, data collection
The local institutional review board approved the protocol for this retrospective study. This approval included a HIPAA waiver of patient authorization owing to the retrospective nature and use of de-identified data in the study.
After receiving institutional approval, the authors reviewed the data for 23 patients who underwent percutaneous placement of PS using their modified technique from November 2015 to August 2016. In an effort to validate this technique, they collected the data for 24 other patients (control group) who were operated on with the Jamshidi needle (Becton, Dickenson and Company, Franklin Lakes, NJ, USA) technique during the same time period (30,55). This technique was performed only in lumbar MIS procedures. The two operative groups were matched for age and body mass index (BMI).
The data, extracted from surgery notes and patients’ charts, included indication for surgery; the patients’ sex, age, and BMI; intraoperative blood loss; intraoperative complications (including screw misplacement that resulted in repositioning of the screw); duration of the surgical procedure; and postoperative complications immediately after surgery and at the time intervals of 30 and 90 days after the procedure.
Technique description
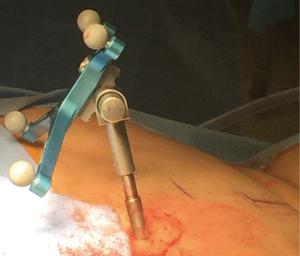
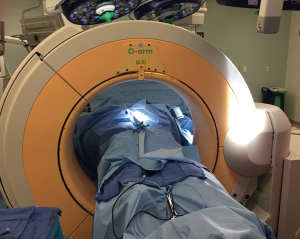
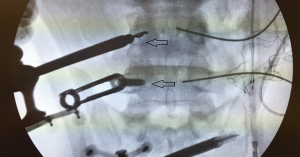
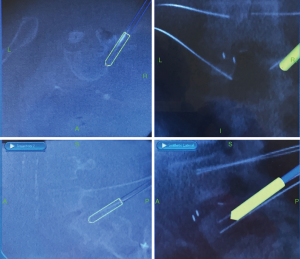
A cone-beam CT (iCBCT) and image-guided navigation system (IGNS) (O-arm Surgical Imaging System, Medtronic, Minneapolis, MN, USA) was used in all cases. After prone positioning of the patient on a Jackson table (Medtronic, Minneapolis, MN, USA), all the navigational instruments were registered, and a reference dynamic navigational frame was implanted percutaneously in the posterior superior iliac spine area (Figure 1). Then a CT scan of the lumbar spine was obtained for navigational purposes (Figure 2). Under the guidance of the navigational system (Stealth Station Surgical Navigation System, Medtronic, Minneapolis, MN, USA) (Figure 3), the optimal entry point and trajectory of the PS were determined, and the trajectory projection was marked on the skin. After a skin incision was made, a navigated drill guide was docked at the optimal entry point on the transverse process and facet junction (Figure 4). In the modified technique, the pedicle was cannulated with a handheld high torque drill (Triton, Medtronic) instead of the Jamshidi needles (Figures 5,6). A drill stop was used to preset the drill length to 25 mm. After the drill was fully inserted and placement of the tip of the drill lateral to the medial border of the pedicles was confirmed, the drill stop was reset to 35 mm and the drill was then advanced (Figures 7,8). Once the handheld drill had been removed, the guidewires were placed through the same drill guide and the screws were implanted over the guidewires. A final intraoperative CT was performed after the screw placement to ensure the optimal position, after which wound closure was completed.



In the control group of patients, the process of registration of the instruments was the same, with the use of the cone-beam CT (iCBCT) and image-guided navigation system (IGNS) After docking of the Jamshidi needle at the optimal entry point for the insertion of the PS, the Jamshidi needles were advanced in order to cannulate the pedicle and vertebral bodies under navigational control.
Results
Descriptive data
A total of 11 men and 12 women with a median age of 57.64 years and a median BMI of 37.65 were operated on according to the modified technique. The matched control group consisted of 10 men and 14 women with a median age of 57.18 years and a median BMI of 37.14. The procedures performed for the modified technique group were: 9 lateral interbody fusions (LIFs), 10 anterior lumbar interbody fusions (ALIFs), and 4 transforaminal lumbar interbody fusions (TLIFs). For the control group, there were 11 LIFs, 11 ALIFs, and 2 TLIFs. A total number of 100 screws were implanted with the modified technique and 104 screws were implanted with the Jamshidi needle technique. Percutaneous screw placement was performed for supplementary stabilization in MIS lumbar spine procedures for both groups of patients.
Outcome data
There were no intraoperative complications associated with the modified or the standard technique. In both operative groups, PS placement was correct, without any breach noted at the pedicles in any case. The average time for PS placement was 6.9 minutes for the new technique. The average time for the standard technique used with the control group was 9.2 minutes. An average blood loss of 54 mL (range, 0–100 mL) was noted in the control group versus an average of 57 mL of blood loss within the same range (0–100 mL) in the new technique group. The average follow-up was 6.2 months in the control group of patients (range, 3–10 months) and 6.5 months in the group of patients with the new technique (range, 2.5–9 months). There were no infections noted in any of the patients at their latest follow-up.
Discussion
Neuronavigation technologies have evolved significantly in spine surgery during the last decades and have provided significant advantages as an adjunct to minimally invasive surgical techniques (56). The reported accuracy in PS placement when fluoroscopic guidance is used ranges between 79.8% and 96.9% (26,28,30,34-36,46,54,57-59) while the intraoperative CT-based navigation technique is between 95.3% and 100% (60-63), and the robotic guidance technique between 83.6% and 100% (46,49,64-66).
Several reports of navigated percutaneous PS placement in the lumbar spine with the use of CT have been published. Jamshidi navigated needles are widely used for the placement of guidewires into the pedicles and vertebral bodies in this procedure as well as in vertebroplasty (30,67). According to our technique, cannulation of the pedicles for the placement of the guidewires is performed through a navigated drill guide. Our technique minimizes the micro-displacement that is noted with Jamshidi needle technique at the entry point to the pedicles and also potential errors in navigation (38). There is minimal displacement of the drill tip even in difficult cases with hypertrophic facets in comparison to Jamshidi needles which enter the pedicle with the use of a mallet. Thus, complications associated with the Jamshidi technique, such as fragmentation of the needles in the presence of sclerotic pedicles or difficult introduction of the needles in small diameter pedicles, are obviated (1,68).
With the modified, new technique, there is minimal need for repositioning or redirection of the drill. If redirection is required, it can be done easily with slight withdrawal of the drill tip and redirection of the drill guides. In addition, there is real-time feedback from the drill-tip as it passes with less resistance through the cancellous bone at the center of the pedicle utilizing the drill and tap technique.
Furthermore, the modification is an efficient method, proven by the comparison of our measurements with those of other studies that used other percutaneous navigated PS insertion techniques (average of 10.35 minutes per screw placement in those studies vs. 6.9 minutes in ours) (58). In addition, our time per screw placement was similar to that reported in a recent study of the K-wireless technique for percutaneous PS placement (average of 6.92 minutes in that study vs. 6.9 minutes in ours) (69). Finally, the modified technique is very favorable in obese patients where the introduction of the guidewires proved to be a more simplified procedure than the more common technique. In both groups of patients studied, the average BMI was more than the normal ratio. The intraoperative CT scans performed after screw insertion did not show any screw malpositioning for either group.
Limitations
Drawbacks for this study are the retrospective design and small number of patients. A large prospective study is warranted to further evaluate the effectiveness of the modified technique.
Conclusions
This modified technique for percutaneous placement of lumbar PS is characterized by minimal blood loss, and decreased operative time in comparison to the commonly used method.
Acknowledgements
The authors thank Paul H. Dressel BFA for preparation of the illustrations and Carrie A. Owens MSILS and Debra J. Zimmer for editorial assistance.
Footnote
Conflicts of Interest: Dr. J Pollina is involved with surgical training for Stryker/NuVasive. The other authors have no conflicts of interest to declare.
References
- Mobbs RJ, Sivabalan P, Li J. Technique, challenges and indications for percutaneous pedicle screw fixation. J Clin Neurosci 2011;18:741-9. [Crossref] [PubMed]
- Jones-Quaidoo SM, Djurasovic M, Owens RK 2nd, et al. Superior articulating facet violation: percutaneous versus open techniques. J Neurosurg Spine 2013;18:593-7. [Crossref] [PubMed]
- Regev GJ, Lee YP, Taylor WR, et al. Nerve injury to the posterior rami medial branch during the insertion of pedicle screws: comparison of mini-open versus percutaneous pedicle screw insertion techniques. Spine (Phila Pa 1976) 2009;34:1239-42. [Crossref] [PubMed]
- Chin KR, Seale J, Cumming V. Mini-open or percutaneous bilateral lumbar transfacet pedicle screw fixation: a technical note. J Spinal Disord Tech 2015;28:61-5. [Crossref] [PubMed]
- Phan K, Rao PJ, Mobbs RJ. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: Systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg 2015;135:85-92. [Crossref] [PubMed]
- Kantelhardt SR, Martinez R, Baerwinkel S, et al. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J 2011;20:860-8. [Crossref] [PubMed]
- Sairyo K, Sakai T, Yasui N. Minimally invasive technique for direct repair of pars interarticularis defects in adults using a percutaneous pedicle screw and hook-rod system. J Neurosurg Spine 2009;10:492-5. [Crossref] [PubMed]
- Wang HW, Li CQ, Zhou Y, et al. Percutaneous pedicle screw fixation through the pedicle of fractured vertebra in the treatment of type A thoracolumbar fractures using Sextant system: an analysis of 38 cases. Chin J Traumatol 2010;13:137-45. [PubMed]
- Gu YT, Zhu DH, Liu HF, et al. Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty for preventing secondary fracture after vertebroplasty. J Orthop Surg Res 2015;10:31. [Crossref] [PubMed]
- Liu D, Zhang B, Xie QY, et al. Biomechanical comparison of pedicle screw augmented with different volumes of polymethylmethacrylate in osteoporotic and severely osteoporotic cadaveric lumbar vertebrae: an experimental study. Spine J 2016;16:1124-32. [Crossref] [PubMed]
- Schizas C, Kosmopoulos V. Percutaneous surgical treatment of chance fractures using cannulated pedicle screws. Report of two cases. J Neurosurg Spine 2007;7:71-4. [Crossref] [PubMed]
- Hardin CA, Nimjee SM, Karikari IO, et al. Percutaneous pedicle screw placement in the thoracic spine: A cadaveric study. Asian J Neurosurg 2013;8:153-6. [Crossref] [PubMed]
- Kuo CC, Martin A, Telles C, et al. Biomechanical demands on posterior fusion instrumentation during lordosis restoration procedures. J Neurosurg Spine 2016;25:345-51. [Crossref] [PubMed]
- Chen XS, Zhou SY, Jia LS, et al. A universal pedicle screw and V-rod system for lumbar isthmic spondylolysis: a retrospective analysis of 21 cases. PLoS One 2013;8:e63713. [Crossref] [PubMed]
- Drazin D, Shirzadi A, Jeswani S, et al. Direct surgical repair of spondylolysis in athletes: indications, techniques, and outcomes. Neurosurg Focus 2011;31:E9. [Crossref] [PubMed]
- Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine (Phila Pa 1976) 1999;24:1252-6. [Crossref] [PubMed]
- Lee SH, Kang BU, Jeon SH, et al. Revision surgery of the lumbar spine: anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation. J Neurosurg Spine 2006;5:228-33. [Crossref] [PubMed]
- Miyashita T, Ataka H, Kato K, et al. Good clinical outcomes and fusion rate of facet fusion with a percutaneous pedicle screw system for degenerative lumbar spondylolisthesis: minimally invasive evolution of posterolateral fusion. Spine (Phila Pa 1976) 2015;40:E552-557. [Crossref] [PubMed]
- Raftopoulos C, Waterkeyn F, Fomekong E, et al. Percutaneous pedicle screw implantation for refractory low back pain: from manual 2D to fully robotic intraoperative 2D/3D fluoroscopy. Adv Tech Stand Neurosurg 2012;38:75-93. [Crossref] [PubMed]
- Niesche M, Juratli TA, Sitoci KH, et al. Percutaneous pedicle screw and rod fixation with TLIF in a series of 14 patients with recurrent lumbar disc herniation. Clin Neurol Neurosurg 2014;124:25-31. [Crossref] [PubMed]
- Jang JS, Lee SH. Clinical analysis of percutaneous facet screw fixation after anterior lumbar interbody fusion. J Neurosurg Spine 2005;3:40-6. [Crossref] [PubMed]
- Pakzaban P. Modified Mini-Open Transforaminal Lumbar Interbody Fusion (MOTLIF): Description of Surgical Technique and Assessment of Free-Hand Pedicle Screw Insertion. Spine (Phila Pa 1976) 2016;41:E1124-30. [Crossref] [PubMed]
- Senker W, Meznik C, Avian A, et al. Perioperative morbidity and complications in minimal access surgery techniques in obese patients with degenerative lumbar disease. Eur Spine J 2011;20:1182-7. [Crossref] [PubMed]
- Park P, Wang MY, Nguyen S, et al. Comparison of Complications and Clinical and Radiographic Outcomes Between Nonobese and Obese Patients with Adult Spinal Deformity Undergoing Minimally Invasive Surgery. World Neurosurg 2016;87:55-60. [Crossref] [PubMed]
- Park P, Upadhyaya C, Garton HJ, et al. The impact of minimally invasive spine surgery on perioperative complications in overweight or obese patients. Neurosurgery 2008;62:693-9; discussion 693-9. [Crossref] [PubMed]
- Nakahara M, Yasuhara T, Inoue T, et al. Accuracy of Percutaneous Pedicle Screw Insertion Technique with Conventional Dual Fluoroscopy Units and a Retrospective Comparative Study Based on Surgeon Experience. Global Spine J 2016;6:322-8. [Crossref] [PubMed]
- Nimjee SM, Karikari IO, Carolyn A, Hardin AB, et al. Safe and accurate placement of thoracic and thoracolumbar percutaneous pedicle screws without image-navigation. Asian J Neurosurg 2015;10:272-5. [Crossref] [PubMed]
- Ahmad FU, Wang MY. Use of anteroposterior view fluoroscopy for targeting percutaneous pedicle screws in cases of spinal deformity with axial rotation. J Neurosurg Spine 2014;21:826-32. [Crossref] [PubMed]
- Ravi B, Zahrai A, Rampersaud R. Clinical accuracy of computer-assisted two-dimensional fluoroscopy for the percutaneous placement of lumbosacral pedicle screws. Spine (Phila Pa 1976) 2011;36:84-91. [Crossref] [PubMed]
- Park DK, Thomas AO, St Clair S, et al. Percutaneous lumbar and thoracic pedicle screws: a trauma experience. J Spinal Disord Tech 2014;27:154-61. [Crossref] [PubMed]
- Mohi Eldin MM, Hassan AS. Percutaneous Transpedicular Fixation: Technical tips and Pitfalls of Sextant and Pathfinder Systems. Asian Spine J 2016;10:111-22. [Crossref] [PubMed]
- Gazzeri R. Percutaneous Pedicle Screw Fixation Technique in the Thoracic and Lumbar Spine-Tips and Tricks. Surg Technol Int 2016;28:303-10. [PubMed]
- Acosta FL Jr, Thompson TL, Campbell S, et al. Use of intraoperative isocentric C-arm 3D fluoroscopy for sextant percutaneous pedicle screw placement: case report and review of the literature. Spine J 2005;5:339-43. [Crossref] [PubMed]
- Holly LT, Foley KT. Three-dimensional fluoroscopy-guided percutaneous thoracolumbar pedicle screw placement. Technical note. J Neurosurg 2003;99:324-9. [PubMed]
- Beckman JM, Murray G, Bach K, et al. Percutaneous Minimally Invasive (MIS) Guide Wire-less Self-Tapping Pedicle Screw Placement in the Thoracic and Lumbar Spine: Safety and Initial Clinical Experience: Technical Note. Neurosurgery 2015;11:530-6.
- Yang BP, Wahl MM, Idler CS. Percutaneous lumbar pedicle screw placement aided by computer-assisted fluoroscopy-based navigation: perioperative results of a prospective, comparative, multicenter study. Spine (Phila Pa 1976) 2012;37:2055-60. [Crossref] [PubMed]
- Houten JK, Nasser R, Baxi N. Clinical assessment of percutaneous lumbar pedicle screw placement using theO-arm multidimensional surgical imaging system. Neurosurgery 2012;70:990-5. [Crossref] [PubMed]
- Eck JC, Lange J, Street J, et al. Accuracy of intraoperative computed tomography-based navigation for placement of percutaneous pedicle screws. Global Spine J 2013;3:103-8. [Crossref] [PubMed]
- Gianaris TJ, Helbig GM, Horn EM. Percutaneous pedicle screw placement with computer-navigated mapping in place of Kirschner wires: clinical article. J Neurosurg Spine 2013;19:608-13. [Crossref] [PubMed]
- Pechlivanis I, Kiriyanthan G, Engelhardt M, et al. Percutaneous placement of pedicle screws in the lumbar spine using a bone mounted miniature robotic system: first experiences and accuracy of screw placement. Spine (Phila Pa 1976) 2009;34:392-8. [Crossref] [PubMed]
- Devito DP, Kaplan L, Dietl R, et al. Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine (Phila Pa 1976) 2010;35:2109-15. [Crossref] [PubMed]
- Kim S, Chung J, Yi BJ, et al. An assistive image-guided surgical robot system using O-arm fluoroscopy for pedicle screw insertion: preliminary and cadaveric study. Neurosurgery 2010;67:1757-67; discussion 1767.
- Lefranc M, Peltier J. Accuracy of thoracolumbar transpedicular and vertebral body percutaneous screw placement: coupling the Rosa(R) Spine robot with intraoperative flat-panel CT guidance--a cadaver study. J Robot Surg 2015;9:331-8. [Crossref] [PubMed]
- Lieberman IH, Hardenbrook MA, Wang JC, et al. Assessment of pedicle screw placement accuracy, procedure time, and radiation exposure using a miniature robotic guidance system. J Spinal Disord Tech 2012;25:241-8. [Crossref] [PubMed]
- Lieberman IH, Togawa D, Kayanja MM, et al. Bone-mounted miniature robotic guidance for pedicle screw and translaminar facet screw placement: Part I--Technical development and a test case result. Neurosurgery 2006;59:641-50; discussion 641-50. [Crossref] [PubMed]
- Schatlo B, Molliqaj G, Cuvinciuc V, et al. Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine 2014;20:636-43. [Crossref] [PubMed]
- Sukovich W, Brink-Danan S, Hardenbrook M. Miniature robotic guidance for pedicle screw placement in posterior spinal fusion: early clinical experience with the SpineAssist. Int J Med Robot 2006;2:114-22. [Crossref] [PubMed]
- Togawa D, Kayanja MM, Reinhardt MK, et al. Bone-mounted miniature robotic guidance for pedicle screw and translaminar facet screw placement: part 2--Evaluation of system accuracy. Neurosurgery 2007;60:ONS129-39; discussion ONS139.
- Wang H, Zhou Y, Liu J, et al. Robot assisted navigated drilling for percutaneous pedicle screw placement: A preliminary animal study. Indian J Orthop 2015;49:452-7. [Crossref] [PubMed]
- Ahn Y, Lee SH. Iatrogenic sacroiliac joint syndrome after percutaneous pedicle screw fixation at the L5-S1 level: case report. Neurosurgery 2010;67:E865-866; discussion E866.
- Babu R, Park JG, Mehta AI, et al. Comparison of superior-level facet joint violations during open and percutaneous pedicle screw placement. Neurosurgery 2012;71:962-70. [Crossref] [PubMed]
- Du JY, Wu JS, Wen ZQ, et al. Treatment strategies for early neurological deficits related to malpositioned pedicle screws in the lumbosacral canal: A pilot study. Bone Joint Res 2016;5:46-51. [Crossref] [PubMed]
- Patel RD, Graziano GP, Vanderhave KL, et al. Facet violation with the placement of percutaneous pedicle screws. Spine (Phila Pa 1976) 2011;36:E1749-1752. [Crossref] [PubMed]
- Smith ZA, Sugimoto K, Lawton CD, et al. Incidence of lumbar spine pedicle breach after percutaneous screw fixation: a radiographic evaluation of 601 screws in 151 patients. J Spinal Disord Tech 2014;27:358-63. [Crossref] [PubMed]
- Beringer W, Potts E, Khairi S, et al. Percutaneous pedicle screw instrumentation for temporary internal bracing of nondisplaced bony Chance fractures. J Spinal Disord Tech 2007;20:242-7. [Crossref] [PubMed]
- Moses ZB, Mayer RR, Strickland BA, et al. Neuronavigation in minimally invasive spine surgery. Neurosurg Focus 2013;35:E12. [Crossref] [PubMed]
- Chiu CK, Kwan MK, Chan CY, et al. The accuracy and safety of fluoroscopically guided percutaneous pedicle screws in the lumbosacral junction and the lumbar spine: a review of 880 screws. Bone Joint J 2015;97-B:1111-7. [Crossref] [PubMed]
- Gu G, Zhang H, He S, et al. Percutaneous Pedicle Screw Placement in the Lumbar Spine: A Comparison Study Between the Novel Guidance System and the Conventional Fluoroscopy Method. J Spinal Disord Tech 2015;28:E522-527. [Crossref] [PubMed]
- Hansen-Algenstaedt N, Chiu CK, Chan CY, et al. Accuracy and safety of fluoroscopic guided percutaneous pedicle screws in thoracic and lumbosacral spine: a review of 2000 screws. Spine (Phila Pa 1976) 2015;40:E954-963. [Crossref] [PubMed]
- Kang HY, Lee SH, Jeon SH, et al. Computed tomography-guided percutaneous facet screw fixation in the lumbar spine. Technical note. J Neurosurg Spine 2007;7:95-8. [Crossref] [PubMed]
- Verma SK, Singh PK, Agrawal D, et al. O-arm with navigation versus C-arm: a review of screw placement over 3 years at a major trauma center. Br J Neurosurg 2016;30:658-61. [Crossref] [PubMed]
- Hsieh JC, Drazin D, Firempong AO, et al. Accuracy of intraoperative computed tomography image-guided surgery in placing pedicle and pelvic screws for primary versus revision spine surgery. Neurosurg Focus 2014;36:E2. [Crossref] [PubMed]
- Ling JM, Dinesh SK, Pang BC, et al. Routine spinal navigation for thoraco-lumbar pedicle screw insertion using the O-arm three-dimensional imaging system improves placement accuracy. J Clin Neurosci 2014;21:493-8. [Crossref] [PubMed]
- Macke JJ, Woo R, Varich L. Accuracy of robot-assisted pedicle screw placement for adolescent idiopathic scoliosis in the pediatric population. J Robot Surg 2016;10:145-50. [Crossref] [PubMed]
- van Dijk JD, van den Ende RP, Stramigioli S, et al. Clinical pedicle screw accuracy and deviation from planning in robot-guided spine surgery: robot-guided pedicle screw accuracy. Spine (Phila Pa 1976) 2015;40:E986-991. [Crossref] [PubMed]
- Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res 2014;472:1839-44. [Crossref] [PubMed]
- Jeon SI, Choe IS, Kwon YS, et al. Comparative clinical results of vertebroplasty using jamshidi(R) needle and bone void filler for acute vertebral compression fractures. Korean J Spine 2012;9:239-43. [Crossref] [PubMed]
- Wang MY, Block S. Retrieval of retained Jamshidi needle fragments during minimally invasive surgery. Journal of neurosurgery. Spine 2011;14:681-4. [Crossref] [PubMed]
- Spitz SM, Sandhu FA, Voyadzis JM. Percutaneous "K-wireless" pedicle screw fixation technique: an evaluation of the initial experience of 100 screws with assessment of accuracy, radiation exposure, and procedure time. J Neurosurg Spine 2015;22:422-31. [Crossref] [PubMed]