National outcomes following single-level cervical disc arthroplasty versus anterior cervical discectomy and fusion
Introduction
Patients with herniated discs, mild spondylosis and degenerative disc disease resulting in radiculopathy and retro-discal myelopathy without facet arthrosis, instability, ossifying diseases or other contraindications can be treated surgically with either cervical disc arthroplasty (CDA) or the gold standard procedure of anterior cervical discectomy and fusion (ACDF). While there are a number of prospective, randomized multi-center studies that have compared the two procedures, all of these involved company-selected surgeons who likely were chosen because they were highly proficient at both procedures. It remains unclear whether procedure type impacts perioperative outcomes when the procedures are performed by “average” spine surgeons. Recent studies have suggested that CDA is a safe and effective alternative to the standard ACDF procedure for symptomatic cervical disease with respect to postoperative function, pain relief, global health status, and development of adjacent segment pathology (1-4). While these studies demonstrated slightly greater benefit in pain reduction after arthroplasty (5), we seek to investigate differences in perioperative outcomes including hospital readmission rate, length of stay, rate of return to the operating room, mortality, and other complications between CDA and ACDF.
Herein, we present a retrospective analysis of the American College of Surgeon’s National Surgical Quality Improvement Program (NSQIP) database to determine differences in 30-day postoperative outcomes between single-level CDA and ACDF. The NSQIP reports data from 517 hospitals and includes over 150 variables. NSQIP is the only database developed and validated by surgeons, and it includes preoperative demographics and comorbidities, intraoperative data points, and 30-day morbidity and mortality (6). In addition, the surgeons who performed the procedures were not a pre-selected group chosen by companies that market the devices. Therefore, it may be a more accurate reflection of outcomes following total disc arthroplasty in the general population than what was reported in FDA-IDE trials or by spine surgeons who publish their results, who may be more experienced than the typical spine surgeon. Unlike other datasets, outcome data is reported by site-specific surgical clinical reviewers instead of insurance claims, lending to its accuracy. Inter-observer disagreement of the dataset is less than 5% (6,7).
Methods
The ACS NSQIP is de-identified and was therefore deemed exempt by our institutional review board. We identified 3,975 patients who underwent either primary single-level ACDF or CDA from 2010–2014 through a retrospective analysis of the American College of Surgeons NSQIP database by utilizing unique Current Procedural Terminology (CPT) codes. The CPT code 22551 was used for ACDF procedures, and the CPT code 22856 was used for CDA procedures. Before the year 2011, ACDF procedures were identified by CPT codes 22554 and 63075. Given the strict indications for CDA, cases involving fractures, tumors, emergent cases, and patients with preoperative compromised wounds were excluded from the analysis, in order to create a more homogenous cohort. Similarly, concomitant posterior cervical, thoracic, or lumbar surgery cases were excluded to isolate single-level ACDF and CDA procedures.
Patient age, gender, postoperative diagnosis, American Society of Anesthesiology Physical Status Classification score (ASA), preoperative laboratory values, and preoperative comorbidities were obtained in addition to perioperative outcome data. The preoperative comorbidities included hypertension requiring medication, history of severe chronic obstructive pulmonary disease, diabetes requiring insulin or oral medication, congestive heart failure within 30 days prior to surgery, renal disease requiring dialysis, current smoking within 1 year of surgery, active corticosteroid use, and history of bleeding disorders. Preoperative lab abnormalities were utilized for analysis: hematocrit <33%, white blood cell count (WBC) >12,000 cells/mcL, creatinine (CR) >1.5 mg/dL, albumin (Alb) <3 g/dL, and platelets (Plt) <100,000/mcL.
Primary outcomes of interest included surgical and medical complications, length of hospital stay (LOS), unplanned readmission, return to operating room, and mortality all occurring within 30 days of the initial procedure. The surgical and medical complications were separated into major and minor complication groups. Major complications included pulmonary embolism, deep venous thrombosis, perioperative myocardial infarction, deep infection, sepsis, septic shock, cerebrovascular accident, acute renal failure, progressive renal insufficiency, and pulmonary events (pneumonia, ventilator use greater than 48 hours, and failure to wean or unplanned intubation). Minor complications included perioperative blood transfusion within 72 hours of surgery, superficial surgical incisional site infection, and urinary tract infection.
Statistical analysis
Propensity score-matching was utilized to create a more homogenous cohort by closely matching the two groups of patients in a paired 1:1 fashion, reducing both selection bias and pre-surgical differences in patient characteristics. Unadjusted univariate analysis was performed to determine whether patient characteristics or outcomes differed by case type; with Chi-squared or Fisher’s exact testing employed for categorical variables and independent sample t-test employed for continuous data. For characteristics and outcomes that demonstrated statistically significant associations (any P value <0.05), odds ratios (OR) in a multivariate model were utilized to control for covariates and determine risk-adjusted relationships between primary outcomes of interest and patient characteristics. Propensity score-matched and multivariate analyses allow for a more accurate evaluation of treatment effects by minimizing inherent patient differences. Findings were considered statistically significant when P<0.05. Analysis was conducted using IBM SPSS Statistics Version 24.
Results
A total of 3,975 patients were identified in the ACS NSQIP search from 2010–2014. Of the 3,975 patients, 3,322 (83.6%) underwent single-level ACDF and 653 (16.4%) underwent single level CDA. A propensity score-matched analysis produced a paired cohort of 1,305 patients with 652 (50.0%) in the ACDF group and 653 (50.0%) in the CDA group. The average age for patients in the CDA and ACDF groups were 44.6±9.7 and 46.9±11.3 years, P<0.001. There was no significant difference in the number of female patients in the ACDF group compared to the CDA group (44.6% vs. 46.1%, P=0.596). There were a larger number of current smokers in the ACDF group (33.0% vs. 22.4%, P<0.001) and patients with elevated white blood cell counts (6.2% vs. 2.7%, P=0.005) when compared to the CDA group. All other preoperative patient characteristics were similar between the groups (Table 1).
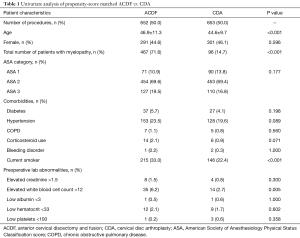
Full table
ACDF procedures were performed more often for patients with myelopathy (71.6% vs. 14.7%, P<0.001). Displacement of cervical intervertebral disc without myelopathy and degeneration of cervical intervertebral disc were the most common postoperative diagnoses for which CDA procedures were performed. Contrastingly, cervical spondylosis with myelopathy and intervertebral disc disorder with myelopathy accounted for the majority of ACDF procedures (Table 2). Other less common diagnoses included cervical spinal stenosis and cervical spondylosis without myelopathy, and brachial neuritis/radiculitis.
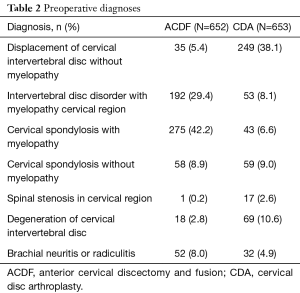
Full table
Major and minor complications were similar between the groups (Table 3). However, ACDF procedures were associated with a significantly longer LOS (14.8±2.3 vs. 1.1±1.0 days, P=0.034) and a higher rate of unplanned readmissions (1.8% vs. 0.2%, P=0.002) when compared to CDA procedures.
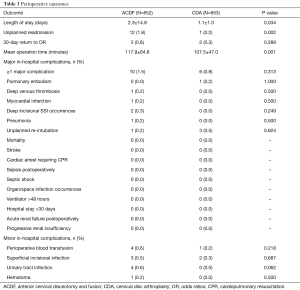
Full table
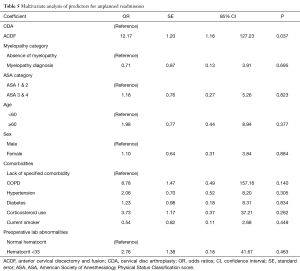
The multivariate analysis noted several associations between outcomes of interest and patient characteristics (Tables 4,5). Increased LOS after ACDF cases persisted in the multivariate model [OR, 4.21; 95% confidence interval (CI), 1.29–13.73, P=0.017]. Furthermore, elevated ASA scores (OR, 2.85; 95% CI, 1.28–6.37; P=0.011), preoperative anemia (OR, 6.82; 95% CI, 1.49–31.30; P=0.013), and elevated white blood cell count (OR, 4.34; 95% CI 1.49–12.62; P=0.007) were also associated with increased length of stay. Additionally, unplanned readmission was found to be significantly associated with the ACDF cohort in the multivariate analysis (OR, 12.17; 95% CI, 1.16–127.23; P=0.037). No other preoperative patient characteristics were significantly associated with an increase in 30-day unplanned readmission.
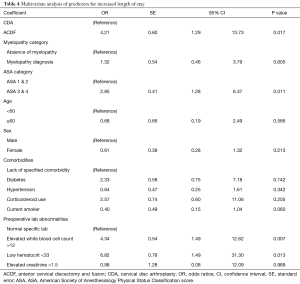
Full table
Full table
Discussion
Select patients with mild spondylosis, stenosis, or intervertebral disc disorders stand to benefit from surgical intervention with ACDF or CDA. In ACDF, neural decompression and spinal stabilization is achieved with disc removal and fusion of the two vertebrate (8). The elimination of motion through fusion is thought to increase stress across adjacent disc spaces, contributing to pathology at adjacent segments (9,10). CDA was developed to preserve natural segmental motion and spinal biomechanics in the hope of avoiding the complications of nonunion and adjacent segment disease associated with ACDF. Despite many articles comparing ACDF and CDA, the risk of perioperative complications, adjacent segment pathology, and reoperation at the index level is still widely debated. Additionally, while there are several prospective, randomized multi-center studies that have compared ACDF and CDA, all of these have involved company-selected surgeons who were likely chosen because they were highly proficient at both types of procedures. By utilizing prospectively acquired national outcome data, our study sought to investigate the demographic profiles and perioperative outcome differences between ACDF and CDA procedures performed by “average” spine surgeons.
In our study, we found that ACDF procedures were associated with a significantly longer hospital LOS and an increased rate of unplanned readmission after controlling for preoperative patient differences via propensity score-matching and multivariate analyses. Additionally, elevated ASA classification, preoperative anemia, and elevated WBC were similarly associated with an increase in LOS. No other patient characteristics showed a significant impact on unplanned readmission.
Due to increased length of stay and resultant readmission, complications after spine surgery can be both devastating and costly. Previous studies have suggested that insulin dependence, chronic steroid use, obesity, and operative time were independent risk factors for spinal surgical complications (11,12). Furthermore, increased age, more extensive operations, medical deconditioning, increased body mass index (BMI), bleeding disorders, and non-independent mobilization were independently associated with a length of stay of greater than 3 days after spine surgery (13). Time in the operating room and duration of hospital admission are directly related to health care costs and risk of surgical morbidity. In a randomized controlled trial of the BRYAN cervical disc replacement and ACDF, Zhang et al. reported that the CDA group had a significantly longer operation time, but equivalent length of stay (14). Similarly, Phillips et al. showed a significantly longer operation time, but decreased length of stay (15). In a recent meta-analysis of thirteen randomized controlled trials, the CDA group had longer operative times, but similar length of stay in the hospital (16). The longer operative times are likely due to the increased complexity of the arthroplasty procedure, as well as the surgeon learning curve for a relatively new operation. More recent data suggest that both ACDF and CDA can be safely and effectively performed in an outpatient setting without any increased untoward complications (17). Our data found a clinically insignificant difference in operative times between the groups, but corroborates the prior reports suggesting that CDA limits LOS. Moreover, increased ASA grade, anemia, and leukocytosis were each associated with increased length of stay.
Unplanned readmission to the hospital is related to a complex interaction between many critical aspects of patient care, including prevention of complications, coordinated disposition plans, and care transition. Prior studies have shown a direct correlation of hospital readmission rate and the quality of health care delivered (18). The effect of preoperative comorbidities and risk of complications in spinal surgery is well-documented throughout the literature, especially in cases involving degenerative spondylolisthesis and adult deformity (19,20). In our analysis, single-level ACDF procedures were associated with a significantly greater number of unplanned hospital readmission, even after controlling for preoperative patient characteristic differences. Careful analysis of comorbidities is essential in the preoperative surgical discussion of potential complications in patients undergoing either ACDF or CDA.
A recent Cochrane Review found that, while small in magnitude, results are statistically in favor of arthroplasty for single-level disease with regards to arm pain, neck pain, neck-related function, and global health status (21). However, while there is data supporting a trend towards better functional outcomes in CDA procedures, revision procedures of CDA show greater incidence of perioperative wound infection, higher cost, and greater LOS compared with revision ACDF by virtue of the increased invasiveness of the revision CDA procedure (22). Therefore, surgeon skill and familiarity with the procedure must be considered when choosing CDA. Similar to other studies, we report that the risk of major and minor complications with primary, single-level ACDF and CDA are comparable when preoperative characteristics are controlled and surgeons are not pre-selected by companies that market the devices (14-16,23).
Many of the limitations of this study are due to the intrinsic limitations of large patient databases. The NSQIP database restricts information to outcomes and complications that occur within 30 days of surgery, limiting the scope of complications that could be measured. Inherent to a large study, the surgeries were performed by a large variety of surgeons, allowing for differences in surgical technique and potential indication bias.
Throughout the literature, inconsistent reporting on complications and a lack of standardized outcome measures prevent a perfect comparison of CDA and ACDF. The use of a nationally recognized database mitigates the variability in outcome measures. The strength of this study is due to the size, scope, and accuracy of the NSQIP database, in which dedicated clinical reviewers at hundreds of institutions report data directly from patient charts. Since the database collects data at a national level, this analysis is applicable to the population as a whole. In addition, our study provides a more accurate reflection of perioperative outcomes following CDA in the typical surgeon population than has been previously reported in FDA-IDE trials or by more experienced spine surgeons that publish their results, because it did not involve a pre-selected group of surgeons chosen by companies that market the devices.
Conclusions
In this analysis of the NSQIP database, the ACDF cohort demonstrated greater LOS and a higher rate of unplanned readmission compared to the CDA cohort, which may have significant impact on patient cost and outcomes. In addition, elevated ASA grade, preoperative anemia, and elevated white blood cell count were associated with greater LOS. Although both ACDF and CDA are performed for similar disease processes, CDA may be performed safely and effectively with comparable perioperative risk of major complications while diminishing LOS and readmission. More long-term prospective studies are necessary to further elucidate the differences in outcomes between CDA and ACDF procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study is exempt from ethics approval by Institutional Review Board at Columbia University. The National Surgical Quality Improvement Program (NSQIP) database contains all de-identified patient information and data, which is exempt from ethics review at Columbia University.
References
- Coric D, Nunley PD, Guyer RD, et al. Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 2011;15:348-58. [Crossref] [PubMed]
- Jawahar A, Cavanaugh DA, Kerr EJ 3rd, et al. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine J 2010;10:1043-8. [Crossref] [PubMed]
- Mummaneni PV, Amin BY, Wu JC, et al. Cervical artificial disc replacement versus fusion in the cervical spine: a systematic review comparing long-term follow-up results from two FDA trials. Evid Based Spine Care J 2012;3:59-66. [Crossref] [PubMed]
- Sasso RC, Anderson PA, Riew KD, et al. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am 2011;93:1684-92. [Crossref] [PubMed]
- Staub LP, Ryser C, Röder C, et al. Total disc arthroplasty versus anterior cervical interbody fusion: use of the Spine Tango registry to supplement the evidence from randomized control trials. Spine J 2016;16:136-45. [Crossref] [PubMed]
- Patel AA, Singh K, Nunley RM, et al. Administrative Databases in Orthopaedic Research: Pearls and Pitfalls of Big Data. J Am Acad Orthop Surg 2016;24:172-9. [Crossref] [PubMed]
- Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6-16. [Crossref] [PubMed]
- Kaiser MG, Haid RW Jr, Subach BR, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002;50:229-36; discussion 236-8. [PubMed]
- Matsunaga S, Kabayama S, Yamamoto T, et al. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 1999;24:670-5. [Crossref] [PubMed]
- Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine 2005;3:417-23. [Crossref] [PubMed]
- Qin C, Kim JY, Hsu WK. Impact of Insulin Dependence on Lumbar Surgery Outcomes: An NSQIP Analysis of 51,277 Patients. Spine (Phila Pa 1976) 2016;41:E687-93. [Crossref] [PubMed]
- Sebastian A, Huddleston P 3rd, Kakar S, et al. Risk factors for surgical site infection after posterior cervical spine surgery: an analysis of 5,441 patients from the ACS NSQIP 2005-2012. Spine J 2016;16:504-9. [Crossref] [PubMed]
- Bekelis K, Desai A, Bakhoum SF, et al. A predictive model of complications after spine surgery: the National Surgical Quality Improvement Program (NSQIP) 2005-2010. Spine J 2014;14:1247-55. [Crossref] [PubMed]
- Zhang X, Zhang X, Chen C, et al. Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China. Spine (Phila Pa 1976) 2012;37:433-8. [Crossref] [PubMed]
- Phillips FM, Lee JY, Geisler FH, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. 2-year results from the US FDA IDE clinical trial. Spine (Phila Pa 1976) 2013;38:E907-18. [Crossref] [PubMed]
- Luo J, Huang S, Gong M, et al. Comparison of artificial cervical arthroplasty versus anterior cervical discectomy and fusion for one-level cervical degenerative disc disease: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 2015;25 Suppl 1:S115-25. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Seale JA, et al. Clinical Outcomes of Outpatient Cervical Total Disc Replacement Compared With Outpatient Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:E567-E74. [Crossref] [PubMed]
- Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med 2000;160:1074-81. [Crossref] [PubMed]
- Kalanithi PS, Patil CG, Boakye M. National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976) 2009;34:1963-9. [Crossref] [PubMed]
- Cho SK, Bridwell KH, Lenke LG, et al. Major complications in revision adult deformity surgery: risk factors and clinical outcomes with 2- to 7-year follow-up. Spine (Phila Pa 1976) 2012;37:489-500. [Crossref] [PubMed]
- Boselie TF, Willems PC, van Mameren H, et al. Arthroplasty versus fusion in single-level cervical degenerative disc disease: a Cochrane review. Spine (Phila Pa 1976) 2013;38:E1096-107. [Crossref] [PubMed]
- Nandyala SV, Marquez-Lara A, Fineberg SJ, et al. Comparison of revision surgeries for one- to two-level cervical TDR and ACDF from 2002 to 2011. Spine J 2014;14:2841-6. [Crossref] [PubMed]
- Zou S, Gao J, Xu B, et al. Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: a meta-analysis of randomized controlled trials. Eur Spine J 2017;26:985-97. [Crossref] [PubMed]


