Gibbus deformity after non-tuberculosis osteomyelitis
Introduction
Gibbus deformities are characterized by the collapse of the anterior portion of one or more vertebral bodies, resulting in kyphosis (1). “Gibbus” is derived from the Late Latin “gibbosus” meaning “humpbacked” (2). The term “gibbous” is most frequently used in contemporary English to describe the lunar phase between half and full when the moon is convex at both edges, exhibiting a “hump” (Figure 1). Gibbus deformities arise most commonly from tuberculosis infection of the spine in the thoracic region but may also result from congenital anomalies including horseshoe kidney (1,3). Compression fractures and metabolic diseases such as mucopolysaccharidoses or cretinism have been implicated in the development of Gibbus deformities (4).

Infection, congenital abnormalities, and metabolic disorders lead to bone weakness making vertebral bodies vulnerable to collapse (3,5). Preferential collapse of the anterior vertebral body leads to a wedge shape and progressive kyphosis characteristic of Gibbus deformities. Progressive kyphosis risks cord compression, myelopathy, and paraplegia if untreated (1). Treatment for Gibbus deformity, caused by infectious sources, requires both antibiotics to treat osteomyelitis as well as surgical correction which usually involve corpectomy, interbody cage placement, and posterior instrumentation and fusion (6). If treated promptly, patients typically improve following surgical correction, with one study demonstrating improvement in postoperative intervertebral height and kyphotic angulation correction from 2.1° to 27.1° (6). Despite a body of literature for Gibbus deformity for tuberculosis osteomyelitis, reports of Gibbus deformity from non-tuberculosis osteomyelitis are very rare. In this report, we present a unique case of Gibbus deformity from non-tuberculosis osteomyelitis and discuss its treatment.
Case presentation
A 39-year-old male was transferred to our institution with a one-month history of worsening back pain, bilateral lower extremity paraesthesias, subjective weakness, and intermittent urinary incontinence. One year prior the patient was diagnosed with non-tuberculosis osteomyelitis at the T11-T12 level and was treated with biopsy and six weeks of oxacillin. On presentation, the patient exhibited trace, pain-limited weakness of the left hip. Sensation remained intact, and no myelopathic signs were noted. Magnetic resonance imaging (MRI) on arrival revealed T11–T12 osteomyelitis and discitis with radiographic evidence of a Gibbus deformity. Marked central spinal stenosis, thoracolumbar spinal cord impingement, and 60° of kyphosis were measured and confirmed with subsequent computed tomography (CT) (Figure 2).

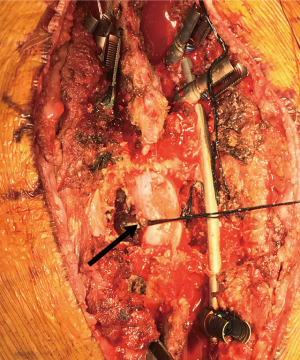
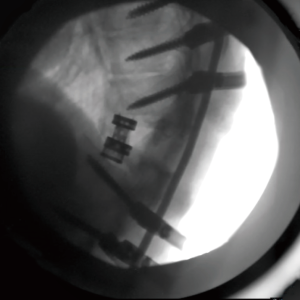
Blood cultures were negative, and the patient was discharged with clinic follow-up. When symptoms persisted 5 months later, the patient was admitted and underwent elective T11–12 corpectomy, placement of an expandable cage, and T8–L3 fusion (Figure 3) with kyphosis correction (Figure 4). The patient’s subsequent postoperative course was unremarkable and he was discharged with an intact neurologic examination. By follow-up at 3 months, the patient reported resolution of symptoms.
Discussion
This report represents a unique case of Gibbus deformity secondary to non-tuberculosis osteomyelitis infection. Vertebral osteomyelitis is an infection of the vertebral body with an incidence of 2.2/100,000 annually (7,8). Infection typically arises by spread from the bloodstream, infected soft tissue, or inoculation from trauma (9). The most common presentation of vertebral osteomyelitis is back pain and pain-limited mobility, although in severe cases of vertebral body destruction and collapse, patients may present with weakness, sensory loss, incontinence, and myelopathic signs (10). Gibbus deformity, named for the Latin word “gibbus” meaning hump, most commonly occurs in the thoracic spine and is characterized by kyphosis from vertebral body collapse. The most common cause of Gibbus deformity is tuberculosis osteomyelitis (1), although it may also result from metabolic disorders or congenital syndromes such as achondroplasia or cretinism and therefore is more common in children than adults. If left untreated, patients with Gibbus deformities are vulnerable to progressive kyphosis, myelopathy, and paraplegia.
Gibbus deformities are rarely reported in the literature and typically involve congenital disorders including horseshoe kidney, myelomeningocele, and myelodysplasia (3,11,12) Among the two cases reported in adults, both Gibbus deformities arose secondary to tuberculosis infection (1,13). Treatment options differ between children and adults. Adults are commonly treated with posterior fusion with or without corpectomy and interbody cage placement, while surgery in children usually involves vertebral column resection and cage insertion with placement of bilateral vertical expandable prosthetic titanium ribs or rods (11,13,14).
Conclusions
This case presents a rare example of Gibbus deformity in an adult patient with non-tuberculosis osteomyelitis. Although Gibbus deformities have become rare as rates of tuberculosis have declined, it remains an important surgical entity that should be recognized by the spine surgeon.
Acknowledgements
The authors would like to thank Ms. Tamara Nuñez, a second-year medical student at the University of Illinois at Chicago, for the gibbous moon photograph.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ghandi M, Aycock RD, Berwald N, et al. Gibbus Deformity. J Emerg Med 2015;49:340-1. [Crossref] [PubMed]
- Merriam-Webster 2017. gibbous. Available online: https://www.merriam-webster.com/dictionary/gibbous
- Bozdogan E, Demir M, Konukoglu O, et al. Reverse U-shaped horseshoe kidney accompanied by gibbus deformity and spina bifida. Jpn J Radiol 2016;34:448-50. [Crossref] [PubMed]
- Palmucci S, Attina G, Lanza ML, et al. Imaging findings of mucopolysaccharidoses: a pictorial review. Insights Imaging 2013;4:443-59. [Crossref] [PubMed]
- Weaver P, Lifeso RM. The radiological diagnosis of tuberculosis of the adult spine. Skeletal Radiol 1984;12:178-86. [Crossref] [PubMed]
- Tosun B, Erdemir C, Yonga O, et al. Surgical treatment of thoracolumbar tuberculosis: a retrospective analysis of autogenous grafting versus expandable cages. Eur Spine J 2014;23:2299-306. [Crossref] [PubMed]
- Digby JM, Kersley JB. Pyogenic non-tuberculous spinal infection: an analysis of thirty cases. J Bone Joint Surg Br 1979;61:47-55. [PubMed]
- Beronius M, Bergman B, Andersson R. Vertebral osteomyelitis in Goteborg, Sweden: a retrospective study of patients during 1990-95. Scand J Infect Dis 2001;33:527-32. [PubMed]
- Berbari EF, Kanj SS, Kowalski TJ, et al. 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin Infect Dis 2015;61:e26-46. [Crossref] [PubMed]
- McHenry MC, Easley KA, Locker GA. Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin Infect Dis 2002;34:1342-50. [Crossref] [PubMed]
- Smith JT, Novais E. Treatment of Gibbus deformity associated with myelomeningocele in the young child with use of the vertical expandable prosthetic titanium rib (VEPTR): a case report. J Bone Joint Surg Am 2010;92:2211-5. [Crossref] [PubMed]
- Smith JT. Bilateral Rib-Based Distraction to the Pelvis for the Management of Congenital Gibbus Deformity in the Growing Child With Myelodysplasia. Spine Deform 2016;4:70-7. [Crossref] [PubMed]
- Chen YH, Lin CB, Wu SW, et al. Surgical treatment of noncontiguous spinal tuberculosis with gibbus deformity: A case report. Ci Ji Yi Xue Za Zhi 2013;25:246-8.
- Şenköylü A, Çetinkaya M. Gibbus deformity. Spine J 2016;16:e237-e8. [Crossref] [PubMed]


