
A Canadian perspective on anterior cervical discectomies: practice patterns and preferences
Introduction
Degenerative cervical spinal disease resulting in radiculopathy and myelopathy has long been treated by anterior cervical discectomy (ACD) (1). The Smith-Robinson (2) and Cloward (3) techniques were described in the literature and both were acceptable approaches to this procedure until the advent of instrumentation. The controversy amongst spinal surgeons regarding ACD versus discectomy with fusion (ACDF) and/or ACD with fusion and plating (ACDFP) has lessened over the last decade with the majority of surgeons choosing instrumentation for these cases. Available data seems to suggest that there is no difference in clinical outcome between methods except a propensity towards segmental kyphosis in the ACD group as well as lower fusion rates in this group compared to the ACDF and ACDFP groups (4,5). However, there is still considerable variation amongst spine surgeons with regards to the surgical procedure of choice (6). Similarly, there is no clear evidence supporting the routine use of external orthoses though there appears to be significant variation amongst surgeons in this regard (7). Cauthen et al. have shown that fusion was unrelated to graft source, cervical collar use or return to work but this was a retrospective, nonrandomized study (8). Intuitively, it would seem that surgeons using a plate would not immobilize their patients in cervical collars post-operatively as the plate would provide an internal brace, promoting graft subsidence and fusion (6). Despite that rationale, many spine surgeons continue to brace their patients in cervical spine collars, with or without instrumentation (9). Similarly, it would seem that intuitively, spinal surgeons would move away from autograft use to other fusion materials in order to avoid the donor site morbidity which inherently comes with its use. Again, this is not necessarily the case as there are many spinal surgeons who continue to use autografts with or without instrumentation and cervical collars. Although some centers find ACDF without plating or external orthoses to adequately treat degenerative spondylosis (10), other studies have found that plating is particularly useful for fusion rates in this group. The use of plating was looked at by Mobbs et al. (11) in a retrospective study comparing outcomes of fusion, kyphosis, graft extrusion and graft collapse with foraminal stenosis in ACDF versus ACDFP. They found superior fusion rates and a lower complication rate in the plating group. Despite this evidence, plating is not the gold standard.
The purpose of this study was to gain an understanding of the practices of Canadian spinal surgeons, specifically with regards to current preferences regarding method, fusion type, plating use, collar use, choice of collar and back to work times. This information would be helpful in designing a prospective, randomized trial addressing the significant variations in practice. A study of this kind looking at ACD method and collar use could lead to standardized practice, which in turn could lead to better outcomes for patients with less post-operative discomfort from wearing a collar and socioeconomic gains resulting from reduced hospital stay and sooner return to work.
Methods
The ACDFP survey was developed collaboratively by the authors with input from content experts.
The survey was one page in order to keep it user friendly and achieve the best possible response rate. It consisted of 13 questions which were sent to all members of the Canadian Neurosurgical Society via SurveyMonkey. Trainees, retired surgeons and surgeons who do not perform spine procedures were excluded. This resulted in responses from 120 neurosurgeons to use in our analysis. Two reminders were sent to optimize the response rate.
Results
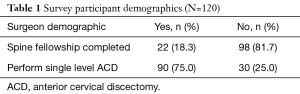
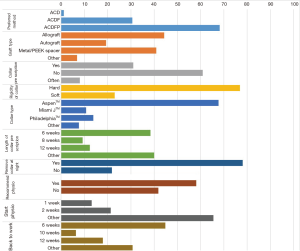
Surveys were sent to 162 surgeons and 120 responded, resulting in a response rate of 74% (95% CI: 51.5–65.7%) (Table 1). There were no differences in demographics between responders and non-responders. Of the responders, 90 (75.0%) said they performed single level ACD. All of the respondents were neurosurgeons (100%) and only some (18.3%) completed spine fellowships. The majority of the respondents performed ACD with fusion and plate (68.2%), followed by ACD with fusion alone (30.7%) while very few performed ACD alone (1.1%). The graft users were divided between allograft (44.3%), autograft (19.3%) and metal/Polyether-ether-ketone spacer (40.9%) with 6.8% using ‘other’ type of graft. The majority of responders (60.9%) did not routinely prescribe collars while 31.0% did. 8.0% of the respondents prescribed collars occasionally. Of the collar prescribers, the majority (76.9%) prescribed hard collars whereas 23.1% prescribed soft collars. Of the collar types, Aspen™ was the most popular (67.7%), followed by Philadelphia™ (13.8%), Miami J™ (10.8%) and other types of collars (7.7%). For length of time of collar use, the majority of responders chose the ‘other/variable’ option (40.0%), followed by 6 weeks (38.5%), 12 weeks (12.3%) and 8 weeks (9.2%). The vast majority of surgeons allowed their patients who wore collars to take them off at night (78.1%), while some required these patients to wear their collars 24 hours a day (21.9%). The majority of responders recommended physiotherapy for patients who underwent this procedure (58.1%), however a significant proportion (41.9%) did not. Time to begin physiotherapy post operatively was divided between 1 week (13.1%), 2 weeks (21.3%) and other (65.6%). The surgeons who chose other were given an option to comment on what length of time they routinely recommend - the most popular answer was 6–8 weeks (35.5%). The final question was regarding timing for return to work. The responses were divided amongst 6 weeks (44.9%), 10 weeks (6.4%), 12 weeks (17.9%) and other (30.8%). The vast majority of those who chose ‘other’ stated in their comments that it depended on the type of work the patient did (61.1%) (Figure 1).
Full table
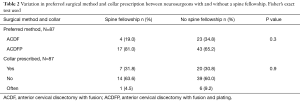
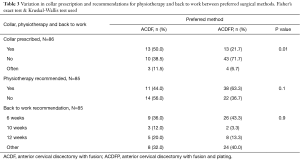
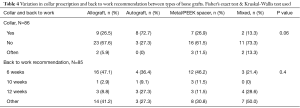
The results of our survey show that regardless of whether the surgeon has a spine fellowship or not, the preferred method of performing ACD was with graft and plate—81.0% (P=0.3) of surgeons with a spine fellowship said they performed ACDFP and 65.2% (P=0.3) of surgeons without a spine fellowship also said that ACDFP was their preferred technique (Table 2). The majority of surgeons (63.6%, P=0.9) with spine fellowships said that they did not use collars. A similar number of surgeons (60.0%, P=0.9) without spine fellowships did not use collars either (Table 2). Half the surgeons (50.0%, P=0.01) who performed anterior cervical discectomies with fusion alone prescribed collars whereas the majority of surgeons (71.7%, P=0.01) who performed anterior cervical discectomies with fusion and plate did not prescribe collars (Table 3). From our results, we can see that autograft users (72.7%, P=0.06) are more likely to prescribe collars whereas 61.5% (P=0.06) of metal/PEEK space users and 67.6% (P=0.06) of allograft users said that they did not prescribe collars for this procedure (Table 4). Physiotherapy was recommended for the majority of ACDFP users (63.3%, P=0.1) whereas the majority of ACDF users (56.0%, P=0.1) did not recommend physiotherapy for their patients (Table 3). Despite choice of method (ACDF =36.0%, ACDFP =43.3%, P=0.9) or graft type used (allograft =47.1%, autograft =36.4%, metal/PEEK spacer =46.2%, P=0.4), the majority of surgeons’ back to work recommendation was 6 weeks (Tables 3 and 4).
Full table
Full table
Full table
Discussion
Our survey seems to demonstrate significant variations in clinical practice amongst Canadian neurosurgeons performing anterior cervical discectomies. Despite the variations, there were certain trends which emerged from the data.
Our response rate of 74% was deemed acceptable according to the calculated confidence interval. Our survey comprised solely of neurosurgeons with only 18.3% of respondents having a spine fellowship. Despite the low number of neurosurgeons with spine fellowships, 75% of respondents said that they performed single level anterior cervical discectomies. This could be a reflection of the high volume of spine cases that most neurosurgery residents would be exposed to during their training, which in turn would lead to a greater comfort level in undertaking these cases without spine fellowship training as compared to their orthopedic colleagues. Unfortunately, we did not capture our orthopedic spinal colleagues in this survey and that data would have been useful for comparison in terms of preferences regarding collar use, instrumentation practices and proportion of orthopedic surgeons with spine fellowships. This is a limitation in our study as the additional data would have been useful for comparison however we were unable to reliably identify our orthopedic spine colleagues with the search method that we employed.
Although it has been suggested in the literature that the only advantage in performing fusion with or without plating over discectomy alone is prevention of segmental kyphosis (4,5), the majority of our respondents stated that they perform ACDFP over ACDF. In fact, the number of surgeons who perform fusion with plating is more than twice the number that perform fusion alone suggesting that despite the literature, most of the spine surgeons in our survey believe that fusion with graft and plating is a better procedure for these patients. In the cross analysis between collar use and method, it became apparent that those surgeons who chose fusion alone were more likely to prescribe a collar (50.0%, P=0.01) versus those who performed fusion with plating. In the fusion and plating group, 71.7% (P=0.01) of respondents said that they did not prescribe a collar for this procedure. These results reach statistical significance and as such, reinforce the concept that the plate acts as an internal brace, obviating the need for collar to promote fusion.
In terms of graft choice, the group was almost evenly divided between metal/PEEK spacer and allograft users (40.9% versus 44.3%) with autograft use being far less popular (19.3%). This finding reflects the trends that we suspected were in place replacing autograft use with allograft, metal or PEEK spacers and cages to reduce donor site morbidity. Although autograft is the gold standard in terms of radiographic fusion rates, the clinical superiority of fusion with autograft remains undetermined (12). This finding coupled with donor site morbidity is likely the reason that autograft use has become less popular.
For collar use, the majority of surgeons did not prescribe collars but when they were used, hard collars were preferable to soft ones and the Aspen™ collar was the most popular choice. Most of the surgeons did prescribe physiotherapy and the majority of them felt that six weeks was the ideal time to undergo physiotherapy. The majority of surgeons recommended that patients return back to work at 6 weeks. A significant number chose ‘other’ for this question and the most common answer was that the type of work the patient did, i.e., heavy labor versus sedentary work, was the most important determinant of when they returned to work. This finding showed that most of the surgeons who participated in our survey were tailoring their recommendations for this patient population based upon the patient’s own individual needs and circumstances.
Our survey is the most up to date description of spine surgeon practice patterns in Canada amongst this patient population. In 2002, Drew et al. (13) reported on Canadian surgeon preferences amongst those performing anterior cervical discectomies. Their paper captured both neurosurgeons and orthopedic surgeons performing anterior cervical discectomies and they found that a greater number of orthopedic surgeons had undergone spine fellowship training versus their neurosurgeon colleagues (82.3% vs. 16.7%). Their finding that 16.7% of neurosurgeons performing anterior cervical discectomies had undergone spine fellowship training is comparable to our finding of 18.3% in our respondents. This comparison shows that the number of neurosurgeons undertaking formal spine fellowships and being able to perform this procedure hasn’t changed over the last decade. They found that 22% of the neurosurgeons surveyed augmented fusion with plating (ACDFP) compared with 68.2% of our respondents. This indicates a trend towards instrumentation in anterior cervical discectomies amongst neurosurgeons over the last 12 years. Drew et al. (13) reported that orthopedic surgeons were far more likely to instrument over their neurosurgeon colleagues. Drew et al. (13) also found that spine fellowship training was significantly associated with use of a plate for single level ACD and fusion. In contrast, our study found that there was no correlation between spine fellowship training amongst neurosurgeons and performing ACD with fusion and plate. Of the group of respondents that said they perform ACDFP, 81.0% (P=0.3) had spine fellowships and 65.2% (P=0.3) did not, indicating that whether or not the surgeon had fellowship training, ACDFP was the preferred technique for our respondents. A similar survey by Bible et al. (9) published in 2009, looked at bracing tendencies of fellowship versus non-fellowship trained surgeons. They found that fellowship trained surgeons were more likely to brace than non-fellowship trained surgeons (61% vs. 46%, P<0.0001). This is in contrast to our study where an almost equal amount of patients were being braced between the fellowship trained group versus the non-fellowship group (31.8% vs. 30.8%, P=0.9). This finding, although not reaching statistical significance is note-worthy because it may indicate a change in clinical practice. Drew et al. (13) reported a higher number of autograft users versus our survey (52.8% vs. 19.3%) and a lower number of allograft (38% vs. 44.3%) and synthetic graft users (19% vs. 40.9%) than our survey. This reflects a growing trend towards allograft and synthetic graft materials over autografts in order to minimize donor site morbidity, which we predicted would be the case (14). Their neurosurgeon respondents prescribed collars 72.2% of the time, which is in contrast to our respondents who only prescribed collars 31.0% of the time. This again is a reflection of the greater tendency to fuse and plate anterior cervical discectomies, obviating the need for external bracing.
Similarly in 2004, Pickett et al. (15) reported on practice patterns of Canadian spinal surgeons performing anterior cervical discectomies and fusion. Their study, like ours, looked solely at single level procedures whereas Drew et al. (13) looked at both single and multi level cervical discectomies. Pickett et al. (15) had both neurosurgeon and orthopedic respondents however they looked at some different parameters than we did such as years in practice of the surgeon, technique used and plate type used. There were some similar questions to our study and those parameters allow for useful comparison. Again, autograft use was higher in their study (76%) as compared to ours confirming a trend away from autograft use. Again, this survey found that orthopedic spine surgeons were more likely to have a formal spine fellowship and also were more likely to use instrumentation. Like our study, they found that recommended length of external bracing was between 1 to 12 weeks, with six weeks being the most commonly reported length of time recommended. Interestingly, this study found that surgeons who have been in practice for less than 5 years were more likely to use anterior cervical plates following ACDF and that surgeons who had been in practice for greater than 10 years were more likely to use bovine grafts. Pickett et al.’s (15) study was published ten years prior to our study and our findings reflect a trend that was identified in their study: more surgeons will use plating to augment fusion for anterior cervical discectomies and fewer surgeons will be using autografts when allografts and metal/PEEK spacers are available.
Conclusions
Our study adds valuable information to a growing body of literature on the subject of anterior cervical discectomies for the treatment of cervical degenerative disease. The trends that we have identified, which include greater use of fusion and plating with discectomy, greater use of synthetic materials and allograft over autograft, decreased collar use especially when plating is used, as well as a consistent back to work recommendation and proportion of surgeons with spine fellowships are reflective of trends which were identified over a decade ago and provide a background for further studies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Hamilton Integrated Research Ethics Board (project number 12-231). Informed consent was not obtained because completing and submitting the questionnaire implied informed consent.
References
- Watters WC 3rd, Levinthal R. Anterior cervical discectomy with and without fusion. Results, complications, and long-term follow-up. Spine (Phila Pa 1976) 1994;19:2343-7. [Crossref] [PubMed]
- Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607-24. [Crossref] [PubMed]
- Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg 1958;15:602-17. [Crossref] [PubMed]
- Konduru S, Findlay G. Anterior cervical discectomy: to graft or not to graft? Br J Neurosurg 2009;23:99-103. [Crossref] [PubMed]
- Xie JC, Hurlbert RJ. Discectomy versus discectomy with fusion versus discectomy with fusion and instrumentation: a prospective randomized study. Neurosurgery 2007;61:107-16; discussion 116-7. [Crossref] [PubMed]
- Irwin ZN, Hilibrand A, Gustavel M, et al. Variation in surgical decision making for degenerative spinal disorders. Part II: cervical spine. Spine (Phila Pa 1976) 2005;30:2214-9. [Crossref] [PubMed]
- Campbell MJ, Carreon LY, Traynelis V, et al. Use of cervical collar after single-level anterior cervical fusion with plate: is it necessary? Spine (Phila Pa 1976) 2009;34:43-8. [Crossref] [PubMed]
- Cauthen JC, Kinard RE, Vogler JB, et al. Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine (Phila Pa 1976) 1998;23:188-92. [Crossref] [PubMed]
- Bible JE, Biswas D, Whang PG, et al. Postoperative bracing after spine surgery for degenerative conditions: a questionnaire study. Spine J 2009;9:309-16. [Crossref] [PubMed]
- Jagannathan J, Shaffrey CI, Oskouian RJ, et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine 2008;8:420-8. [Crossref] [PubMed]
- Mobbs RJ, Rao P, Chandran NK. Anterior cervical discectomy and fusion: analysis of surgical outcome with and without plating. J Clin Neurosci 2007;14:639-42. [Crossref] [PubMed]
- Floyd T, Ohnmeiss D. A meta-analysis of autograft versus allograft in anterior cervical fusion. Eur Spine J 2000;9:398-403. [Crossref] [PubMed]
- Drew B, Bhandari M, Orr D, et al. Surgical preference in anterior cervical discectomy: a national survey of Canadian spine surgeons. J Spinal Disord Tech 2002;15:454-7. [Crossref] [PubMed]
- Robinson RA, Walker AE, Ferlic DC, et al. The Results of Anterior Interbody Fusion of the Cervical Spine. J Bone Joint Surg Am 1962;44:1569-87. [Crossref]
- Pickett GE, Van Soelen J, Duggal N. Controversies in cervical discectomy and fusion: practice patterns among Canadian surgeons. Can J Neurol Sci 2004;31:478-83. [Crossref] [PubMed]


