The effectiveness of non-surgical treatments, re-discectomy and minimally invasive transforaminal lumbar interbody fusion in post-discectomy pain syndrome
Introduction
Discectomy is the accepted treatment option for intervertebral disc herniation in patients who have had unsuccessful conservative treatment. However, the overall rate of unsatisfactory results after discectomy is reported between 5% and 37% (1-6).
There have been many studies that reported various treatment options about recurrent disc herniation, recurrent sciatica, and low back pain following discectomy. Most of these studies evaluated and reported mixed patient populations including patients with spinal-foraminal stenosis, recurrent disc herniation, perineural fibrosis, instability, and degenerative spinal conditions (1,2,7-14). However, due to these mixed and complex underlying conditions, evaluation and treatment algorithm of post-discectomy pain syndrome (PDPS) could not be standardized. The purpose of this study was to report the results of non-surgical treatments and re-discectomy for PDPS and present our clinical results of minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) procedures for patients who unsuccessfully underwent non-surgical treatments and re-discectomy.
Methods
After institutional review board (IRB) approval we retrospectively evaluated 75 patients with PDPS between 2009 and 2014. Fifty-three of these patients had their index surgery at different institutions whereas 22 had at our institution. The mean duration between the index surgery and the diagnosis of PDPS was 6 (range, 4–20) months. During this period, these patients were treated with oral or intramuscular pain medication only. Patients were diagnosed as PDPS at the time of their admittance to our institution. First, we applied 12 weeks of conservative treatment to all patients. These conservative treatments included activity modulation and pain treatment and/or comprehensive physical therapy programs. The pain medications that were given to the patients were analgesics, nonsteroidal anti-inflammatory agents (NSAIDs), muscle relaxants, narcotic medications, and neuro-modulating medications. The 21 patients have responded positively to the 12-week of conservative treatments. We routinely obtained magnetic resonance imaging (MRI) with gadolinium enhancement, 3-dimensional computerized tomography (3D-CT) scan, lumbar dynamic radiographs, and electromyography (EMG) for patients who did not respond to conservative treatments after the 12 weeks. These evaluation methods were used at the time of diagnosis only. After these diagnostic studies, the diagnoses of the patients were classified as epidural fibrosis, recurrent disc herniation, facet joint arthrosis, spondylodiscitis, erosive osteochondrosis, instability, and polyneuropathy. Since evaluation of the outcomes would be debatable, the patients who were diagnosed with polyneuropathy (with or without the diagnoses mentioned above) by using EMG were excluded from this study. After these evaluations, 54 patients who did not respond to the 12 weeks of conservative treatments were included in our study. The distribution of the underlying diagnoses and applied treatments are summarized in Figure 1. The mean age of the patients was 44.3 (range, 28–55) years. Thirty-four of the patients were female and 20 were male.
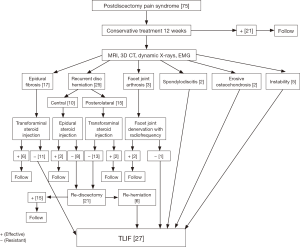
The patients with facet joint arthrosis that were confirmed with 3D-CT had a facet joint denervation with radiofrequency (RF). Instability was defined based on the measurements on three lateral radiographs at neutral, extension, and flexion positions. Measurement of slip was performed using the method basically described by White and Panjabi (15). A slip of ≥3 mm in the neutral position, ≥3 mm translation, or ≥10 degrees angulation was defined as instable. The diagnosis of the patients who were included in the study were epidural fibrosis in 17 patients, recurrent disc herniation in 25 patients, facet joint arthrosis in three patients, spondylodiscitis in two patients, erosive osteochondrosis in two patients, and segmental instability in five patients. The patients with the diagnosis including epidural fibrosis, recurrent disc herniation and facet joint arthrosis were treated conservatively in the first manner. The patients with the other diagnoses were treated with MIS-TLIF. One of the three patients who were included to the group of facet joint arthrosis also had an epidural fibrosis and one also had a recurrent disc herniation. These patients were treated both with steroid injections and facet joint denervation with RF. The patients with recurrent disc herniation who did not respond to steroid injections were treated with re-discectomy first. Second re-herniations were treated with MIS-TLIF surgery.
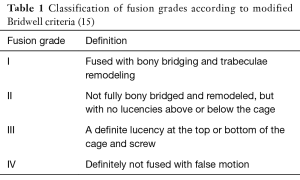
Eventually 27 patients underwent MIS-TLIF surgery and 12 patients responded well to the non-surgical treatments which are described in Figure 1 and had no need for surgery. Six of these patients who responded well to the non-surgical treatments had suffered from epidural fibrosis and four from a central or posterolateral recurrent disc herniation which were managed with a transforaminal or epidural steroid injection. Two patients with a facet joint arthrosis were treated with facet joint denervation using RF along with steroid injections responded well to the non-surgical treatment as well. Twenty-one of 25 patients with recurrent disc herniation were treated with re-discectomy. The complaints of 15 patients who had a re-discectomy completely resolved and had no need for further intervention. However, six patients who had a re-discectomy suffered from a second re-herniation and were treated with a MIS-TLIF. The diagnoses of 27 patients who underwent a MIS-TLIF surgery were epidural fibrosis in 11 patients, recurrent disc herniation in six patients, facet joint arthrosis in one patient, spondylodiscitis in two patients, erosive osteochondrosis in two patients, and segmental instability in five patients. All patients were evaluated using the 10-point visual analog scale (VAS) and Oswestry Disability Index (ODI) preoperatively and at the post-treatment or postoperative 6th week, 6th month, 1-year, and final follow-ups. The patients with a diagnosis of recurrent disc herniation were also checked with physical examination and a post-operative MRI with gadolinium enhancement after the re-discectomy procedure in order to confirm the success of the procedure. Furthermore, we obtained plain X-rays and physical examinations for the patients who underwent MIS-TLIF surgery at the postoperative follow-ups. Postoperative X-rays included anteroposterior, lateral, flexion and extension views of the lumbar spine. Since the patients who were treated non-surgically had no complaints, we did not obtain any radiological studies for these patients at their respective follow-ups. At the final follow-up we also evaluated the fusion with the modified Bridwell criteria which was described by Lee et al. (16) (Table 1). Grades I and II fusion in this classification system were considered to be solid fusion. We also asked the patients to rate their satisfaction as excellent, good, fair, or poor at their final follow-up. At the follow-ups, a physician who was not otherwise involved in the surgeries assessed the VAS and ODI and radiological fusion of the patients and recorded their satisfaction levels.
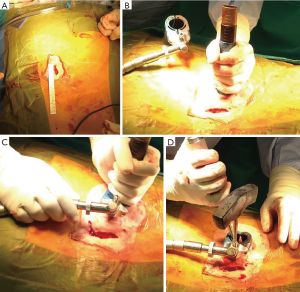
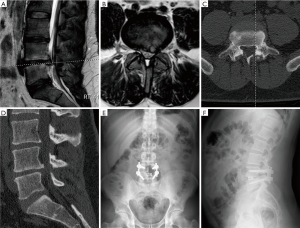
The mean interval between the index surgery and the MIS-TLIF surgery was 9 (range, 4–34) months. The fused levels were L3–L4 in 6 patients, L4–L5 in 11 patients and L5–S1 in 10 patients. During and after surgery detailed records were kept of any intraoperative difficulties and complications that arose. The surgical technique of the MIS-TLIF is summarized in Figure 2.
Statistical analysis was performed using IBM SPSS (Statistical Package for Social Sciences) for Windows 21 software (IBM Corp., Armonk, NY, USA). The mean VAS scores, ODI scores, and standard deviations were calculated and compared to each other using Friedman test and Wilcoxon Sign test. Statistical significance was defined as P<0.05.
Results
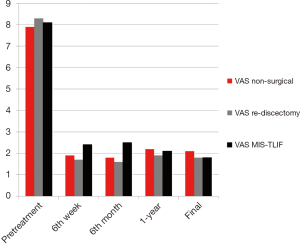
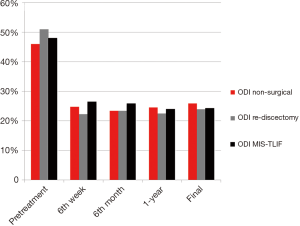
The mean follow-up for the patients who benefited from non-surgical treatments was 25.2 (range, 24–32) months. Pre-treatment mean VAS score of these patients was 7.9 (range, 6–9). The mean VAS score decreased to 1.9 (range, 0–3) at the 6th post-treatment week. The mean VAS scores were 1.8 (range, 0–3) at the 6th month, 2.2 (range, 0–4) at the 1-year and 2.1 (range, 0–4) at the final follow-up. The mean pre-treatment ODI was 46% (range, 28–62%), which decreased to 24.8% (range, 4–34%) at the postoperative 6th week, 23.4% (range, 4–30%) at the postoperative 6th month, 24.5% (range, 4–36%) at the postoperative 1-year, and 25.9% (range, 4–38%) at the final follow-up. The changes in VAS and ODI scores between the pre-treatment period and the post-treatment follow-ups were statistically significant (P<0.001).
The mean follow-up for the patients who benefited from re-discectomy was 28.4 (range, 27–38) months. Pre-treatment mean VAS score of these patients was 8.3 (range, 6–10). The mean VAS score decreased to 1.7 (range, 0–3) at the 6th post-treatment week. The mean VAS scores were 1.6 (range, 0–3) at the 6th month, 1.9 (range, 0–4) at the 1-year and 1.8 (range, 0–4) at the final follow-up. The mean pre-treatment ODI was 51% (range, 28–62%), which decreased to 22.3% (range, 4–26%) at the postoperative 6th week, 23.4% (range, 4–28%) at the postoperative 6th month, 22.5% (range, 4–30%) at the postoperative 1-year, and 23.9% (range, 4–30%) at the final follow-up. The changes in VAS and ODI scores between the pre-treatment period and the post-treatment follow-ups were statistically significant as well (P<0.001).
The mean follow-up for the patients who underwent MIS-TLIF surgery was 34.2 (range, 25–52) months. The average surgical time was 163 (range, 143–202) minutes. The mean blood loss during surgery was 243 (range, 186–300) mL. The average hospital stay was 3.4 (range, 2–14) days. Preoperative mean VAS score was 8.1 (range, 7–10). The average VAS score decreased to 2.4 (range, 1–4) at the 6th postoperative week, 2.5 (range, 0–5) at the 6th month follow-up, 2.1 (range, 0–4) at the 1-year follow-up and to 1.8 (range, 0–4) at the final follow-up. The mean preoperative ODI was 48% (range, 32–64%), which decreased to 26.4% (range, 5–40%) at the postoperative 6th week, 25.8% (range, 0–38%) at the 6th month follow-up, 23.9% (range, 0–34%) at the 1-year follow-up, and 24.2% (range, 0–36%) at the final follow-up. The changes in VAS and ODI scores between the pre-treatment period and the postoperative follow-ups were statistically significant (P<0.0001). Figures 3,4 demonstrate the results of patients who benefited from non-surgical treatments, re-discectomy and patients who have undergone a MIS-TLIF procedure. At the final follow-up, all patients who were treated with MIS-TLIF and who benefited from non-surgical treatments and re-discectomy rated their satisfaction as excellent or good. Transient sensorial disturbance which resolved without any additional intervention was the most common complication in our patients who were treated with MIS-TLIF, which occurred in 5 patients. In one patient who was diagnosed with epidural fibrosis, a CSF leak occurred and resolved with bed rest for 2 weeks. The CSF leak was not evident during this patient’s surgery. This patient stayed in the hospital during the healing process and was discharged 2 weeks after his surgery. There was no postoperative infection, permanent neurologic deficit, pseudarthrosis, and implant-related complications in our series. At the final follow-up, the radiological fusion of all patients in our series were accepted as Grade I or II fusion according to the Bridwell fusion criteria that was modified by Lee et al. (16). Figure 5 demonstrates a 31-year-old male patient in whom recurrent disc herniation occurred following the discectomy surgery. Finally, he underwent MIS-TLIF surgery at the L4–L5 level.
Discussion
Long-term studies have shown that 11% to 30% of the patients who are treated with discectomy suffer from disabling lower-back pain (4,10,17-22). Recurrence of disc herniation has been reported as 5–11% after discectomy in literature (2,7-9). Treatment of recurrent disc herniation is still controversial. Success rates of a repeat discectomy are reported as lower (60–80%) when compared with the primary discectomy (80–90%) (2,9,23-26). Recurrent disc herniation and perineural fibrosis are major the causes of pain after discectomy. Differential diagnosis of recurrent disc herniation and perineural fibrosis is important and influences clinical outcomes (2). Suk et al. (2) reported their patients’ clinical improvement after re-discectomy as good as yielded by the primary discectomy and related this good clinical outcome to distinguishing recurrent disc herniation with perineural fibrosis by using MRI with gadolinium enhancement. In our series, we differentiated recurrent disc herniation from perineural fibrosis by using MRI with gadolinium enhancement as well. We also evaluated all patients who were suffering from post-discectomy pain with 3D-CT, and dynamic X-rays in order to show all possible underlying causes of post-discectomy pain.
There are controversies regarding the surgical treatment of recurrent disc herniation, and post-discectomy lower back pain. The surgical options include re-discectomy (1,2,7-9,13), posterior-only fusion (27-29), interbody fusion (12), 360-degree circumferential fusion (30-33), total disc replacement (10), and ALIF surgery (34). We prefer to perform re-discectomy for patients with recurrent disc herniation and use MIS-TLIF for patients with a second recurrence. Six of the 21 patients in our series who underwent a re-discectomy needed MIS-TLIF.
MIS-TLIF certainly provides several theoretical advantages. The approach addresses most of the underlying pathologies of PDPS. MIS-TLIF with bilateral pedicle screw fixation and fusion allows cleaning of the epidural fibrotic tissue with the posterior approach, to treat the recurrent disc herniation and spondylodiscitis by excising the remaining disc tissue, and provides 360 degrees stable fusion for facet joint arthrosis, erosive osteocondritis, and instability. This method also provides access to disc herniations that have migrated rostrally or caudally from the disc space, and eliminates the chance of additional recurrent disc herniations at the affected level (34-37). The patients who were treated with a minimally invasive approach experience improved cosmoses and less postoperative pain and intraoperative blood loss related to limited surgical incision. However, this is a technically demanding technique and there is a learning curve for this procedure (16). Conversely, radiographic evaluation is sometimes limited to diagnose postoperative pathologies. In these cases, in whom radiographic and EMG studies cannot confirm a diagnosis, open surgery, e.g., conventional PLIF or TLIF, might be better to confirm the possible pathologies and treat them properly and adequately.
Disadvantages of the MIS-TLIF approach for PDPS include the need of mobilization of scarred dura or nerve roots and increased risk of dural injury and cerebrospinal fluid leak. This can be avoided with meticulous dissection of scarred dural tissue. Although we experienced only one CSF leak in a patient with epidural fibrosis, which resolved with bed rest, it can be managed with repair of the dura with sutures, facial patch, fibrin glue, and placement of a lumbar drain if it is noticed during the surgery.
Based on the early clinical results of this study, MIS-TLIF with bilateral pedicle screw fixation seems as an effective procedure for the relief of post-discectomy pain that is resistant to treatment options which were described here. However, our study has some limitations. Although thin sliced CT would be better for fusion evaluation, we used X-ray fusion evaluation because of the fact that we reserved the use of CT only for patients whose radiological fusion were doubtful or delayed or where there was a suspicion of pseudarthrosis. Despite the promising results, the study is nonetheless a low level of evidence because of its retrospective nature and lack of a “control” group. Our outcomes can only be compared with similar studies involving other fusion techniques. It would be useful to know how the initial non-responders respond to continued non-operative treatment and compare their results with our surgical group. Also comparing the results of MIS-TLIF on patients with a first-time recurrence of disc herniation to the patients who have undergone re-discectomy alone would be beneficial in order to better understand the effectiveness of the surgical procedure mentioned above.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study has been approved by the hospital committee and the local ethics committee. Written informed consent was obtained from the patients for publication of the images.
References
- Law JD, Lehman RA, Kirsch WM. Reoperation after lumbar intervertebral disc surgery. J Neurosurg 1978;48:259-63. [Crossref] [PubMed]
- Suk KS, Lee HM, Moon SH, et al. Recurrent lumbar disc herniation: results of operative management. Spine 2001;26:672-6. [Crossref] [PubMed]
- Frymoyer JW, Hanley E, Howe J, et al. Disc excision and spine fusion in the management of lumbar disc disease. A minimum ten-year follow up. Spine 1978;3:1-6. [Crossref] [PubMed]
- Atlas SJ, Keller RB, Wu YA, et al. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10-year results from the maine lumbar spine study. Spine 2005;30:927-35. [Crossref] [PubMed]
- Martin G. Recurrent disc prolapse as a cause of recurrent pain after laminectomy for lumbar disc lesions. N Z Med J 1980;91:206-8. [PubMed]
- Crock HV. Observations on the management of failed spinal operations. J Bone Joint Surg Br 1976;58:193-9. [Crossref] [PubMed]
- Connolly ES. Surgery for recurrent lumbar disc herniation. Clin Neurosurg 1992;39:211-6. [PubMed]
- Fandiño J, Botana C, Viladrich A, et al. Reoperation after lumbar disc surgery: results in 130 cases. Acta Neurochir (Wien) 1993;122:102-4. [Crossref] [PubMed]
- O'Sullivan MG, Connolly AE, Buckley TF. Recurrent lumbar disc protrusion. Br J Neurosurg 1990;4:319-25. [Crossref] [PubMed]
- Leahy M, Zigler JE, Ohnmeiss DD, et al. Comparison of results of total disc replacement in postdiscectomy patients versus patients with no previous lumbar surgery. Spine 2008;33:1690-3. [Crossref] [PubMed]
- Bernard TN. Repeat lumbar spine surgery. Factors influencing outcome. Spine 1993;18:2196-200. [Crossref] [PubMed]
- Gepstein R, Shabat S, Reichel M, et al. Treatment of postdiscectomy low back pain by percutaneous posterior lumbar interbody fusion versus open posterior lumbar fusion with pedicle screws. Spine J 2008;8:741-6. [Crossref] [PubMed]
- Jönsson B, Strömqvist B. Repeat decompression of lumbar nerve roots. A prospective two-year evaluation. J Bone Joint Surg Br 1993;75:894-7. [Crossref] [PubMed]
- Jackson RK. The long-term effects of wide laminectomy for lumbar disc excision.A review of 130 patients. J Bone Joint Surg Br 1971;53:609-16. [Crossref] [PubMed]
- White AA III, Panjabi MM. Clinical biomechanics of the spine. 2nd edition. Philadelphia: Lippincott, 1990.
- Lee JC, Jang HD, Shin BJ. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: our experience in 86 consecutive cases. Spine 2012;37:1548-57. [Crossref] [PubMed]
- DePalma AF, Rothman RH. Surgery of the lumbar spine. Clin Orthop Relat Res 1969.162-70. [PubMed]
- Hanley EN Jr, Shapiro DE. The development of low-back pain after excision of a lumbar disc. J Bone Joint Surg Am 1989;71:719-21. [Crossref] [PubMed]
- Dvorak J, Gauchat MH, Valach L. The outcome of surgery for lumbar disc herniation. I. A 4-17 years' follow-up with emphasis on somatic aspects. Spine 1988;13:1418-22. [Crossref] [PubMed]
- Lewis PJ, Weir BK, Broad RW, et al. Long-term prospective study of lumbosacral discectomy. J Neurosurg 1987;67:49-53. [Crossref] [PubMed]
- Loupasis GA, Stamos K, Katonis PG, et al. Seven to 20-year outcome of lumbar discectomy. Spine 1999;24:2313-7. [Crossref] [PubMed]
- Naylor A. Late results of laminectomy for lumbar disc prolapse. A review after ten to twenty-five years. J Bone Joint Surg Br 1974;56:17-29. [PubMed]
- Herron L. Recurrent lumbar disc herniation: results of repeat laminectomy and discectomy. J Spinal Disord 1994;7:161-6. [Crossref] [PubMed]
- Findlay GF, Hall BI, Musa BS, et al. A 10-year follow-up of the outcome of lumbar microdiscectomy. Spine 1998;23:1168-71. [Crossref] [PubMed]
- Goffin J. Microdiscectomy for lumbar disc herniation. Clin Neurol Neurosurg 1994;96:130-4. [Crossref] [PubMed]
- Kulali A, von Wild K. Microsurgical management of the lumbar intervertebral disc-disease. Neurosurg Rev 1995;18:183-8. [Crossref] [PubMed]
- Jackson RK, Boston DA, Edge AJ. Lateral mass fusion. A prospective study of a consecutive series with long-term follow-up. Spine 1985;10:828-32. [Crossref] [PubMed]
- O'Beirne J, O'Neill D, Gallagher J, et al. Spinal fusion for back pain: a clinical and radiological review. J Spinal Disord 1992;5:32-8. [Crossref] [PubMed]
- Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine 1996;21:626-33. [Crossref] [PubMed]
- Ray CD. Threaded titanium cages for lumbar interbody fusions. Spine 1997;22:667-79. [Crossref] [PubMed]
- Christensen FB, Hansen ES, Eiskjaer SP, et al. Circumferential lumbar spinal fusion with Brantigan cage versus posterolateral fusion with titanium Cotrel-Dubousset instrumentation: a prospective, randomized clinical study of 146 patients. Spine 2002;27:2674-83. [Crossref] [PubMed]
- Leufvén C, Nordwall A. Management of chronic disabling low back pain with 360 degrees fusion. Results from pain provocation test and concurrent posterior lumbar interbody fusion, posterolateral fusion, and pedicle screw instrumentation in patients with chronic disabling low back pain. Spine 1999;24:2042-5. [Crossref] [PubMed]
- Kuslich SD, Ulstrom CL, Griffith SL, et al. The Bagby and Kuslich method of lumbar interbody fusion.History, techniques, and 2-year follow-up results of a United States prospective, multicenter trial. Spine 1998;23:1267-78. [Crossref] [PubMed]
- Choi JY, Choi YW, Sung KH. Anterior lumbar interbody fusion in patients with a previous discectomy: minimum 2-year follow-up. J Spinal Disord Tech 2005;18:347-52. [Crossref] [PubMed]
- Lee CK, Langrana NA. Lumbosacral spinal fusion.A biomechanical study. Spine 1984;9:574-81. [Crossref] [PubMed]
- Schlegel KF, Pon A. The biomechanics of posterior lumbar interbody fusion (PLIF) in spondylolisthesis. Clin Orthop Relat Res 1985.115-9. [PubMed]
- Regan JJ, Yuan H, McAfee PC. Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery. A prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine 1999;24:402-11. [Crossref] [PubMed]