
Kyphoplasty patient-centered outcomes via questionnaire
Introduction
Cement augmentation of vertebral bodies began in 1987 with the treatment of vertebral hemangiomas by Gailbert et al. (1). In 2001, kyphoplasty was introduced as a novel method of augmenting vertebral bodies with cement (2). In 2009, two studies of vertebroplasty versus sham procedure concluded that vertebroplasty was unsuccessful (3,4). Kyphoplasty usage declined significantly in 2009, presumably secondary to the results published in these two studies (5). Despite these reported outcomes, anecdotal success with kyphoplasty continued among individual surgeons. Other publications subsequently appeared in the literature that directly contradicted the results from the sham studies, including one randomized controlled trial (6) and one large observational study (7). Results from these studies have highlighted the ability of kyphoplasty to decrease subjective measures such as back pain (6-9), improve quality of life (6,9), reduce physical disability and decrease mortality (10-12). The effect has been studied mainly in the osteoporosis literature but has also shown effectiveness in the groups of patients suffering from pathological fracture secondary to malignancy (13).
The economic impact of kyphoplasty has been studied and shown to reduce healthcare utilization (14), shorten hospital stay (10,11), decrease outpatient follow up visits (15), and reduce narcotic use (7). Currently, healthcare reimbursement is dependent upon not only standardized measures of success but also high patient satisfaction. Current research supports the use of kyphoplasty from a functional and economic standpoint but looking at patients’ perspective in medical research is important to complete the overall picture of efficacy. To date in the kyphoplasty literature, only one paper, the 2-year follow up from the FREE paper, has mentioned patient satisfaction using a 20-point Likert scale (9). They mention statistical significance but do not elaborate on the subject. The objective of our survey was to assess patient-centered outcome measures using specific questions directed at procedure tolerability, pain relief, and willingness to undergo the same procedure again to show the benefits of kyphoplasty not only objectively, but also subjectively from the patients’ perspective.
Methods
Patients
Patients were included in this study if they were >18 years old, with an acute compression fracture confirmed by MRI or nuclear bone scan and had a kyphoplasty performed. Patients were identified using a coding query from clinic and hospital electronic medical record. All patients who had undergone a kyphoplasty procedure from 2008–2011 were identified. Demographic data from these patients were obtained through electronic medical records. The social security numbers of the patients were checked against the Social Security Death Index (http://www.genealogybank.com/gbnk/ssdi/). The deceased patients were identified and excluded from the study. The indication for kyphoplasty was assessed using the medical records as well as pathological information from bone biopsy. They were separated into osteoporotic/spontaneous fractures, fractures related to biopsy-proven malignancy, or traumatic fractures.
Kyphoplasty
Patients were eligible for kyphoplasty based on magnetic resonance imaging or nuclear bone scan demonstrating an acute compression fracture, hyperintensity on STIR sequences and hypointensity on T1 sequences suggesting edema, as well as clinical findings of intractable back pain despite non-operative treatment. All patients identified had a kyphoplasty performed by unipedicular, bipedicular or extrapedicular approach depending upon surgeon preference. All kyphoplasty was performed using the Kyphon Balloon Kyphoplasty system (Medtronic Spine, LLC, Sunnyvale, CA, USA).
Survey
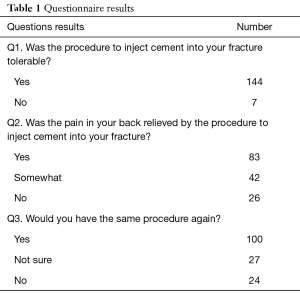
The included patients were contacted through telephone numbers obtained in the demographic data of their electronic health record. The “Kyphoplasty Telephone Satisfaction Survey”, a simple three-question survey, was administered to the patient. Institutional review board approval was obtained prior to data collection. Questions asked by the survey are presented in Table 1. No family member was allowed to take the survey for the patient. If the patient was unable to complete the interview through the telephone they were excluded from the survey and study. If the patient was unavailable for conversation or unreachable, two more attempts were made, for a total of three attempts, before the patient was counted as unreachable and excluded.
Full table
Results
Four hundred ninety-two patients were identified from the coding query. Of these, 173 patients were excluded due to identification on the Social Security Death Index as being deceased. Three hundred nineteen patients remained. Nine patients refused to participate in the questionnaire and were excluded. One hundred and fifty-nine were unreachable or unable to complete the questionnaire. The remaining 151 of available 310 alive participants were reached and completed the survey, a response rate of 48.7%.
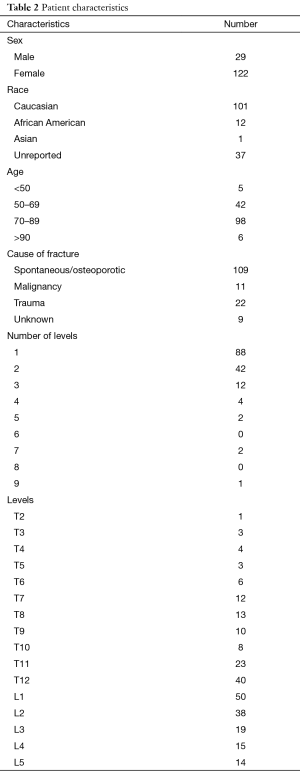
This patient cohort of respondents represents a typical variety for a private practice physician performing these procedures. Full characteristics of the respondents are presented in Table 2. The majority of the patients were Caucasian females. The age range was from 26–101, with an average age of 74.3. The most common level requiring kyphoplasty was L1, followed by T12 and then L2. Overall, 61.3% of fractures were at the thoracolumbar junction (T10–L2). Most patients (130 of 151) had either one or two levels treated. No patient had more than three levels performed at one time. The cause for surgery was mainly osteoporotic or spontaneous fractures, which accounted for 72.0% of all patients.
Full table
Overall, 95.4% of respondents said the procedure was tolerable. When asked regarding pain relief, 82.8% of respondents had partial or full pain relief from the procedure, with 55.0% overall stating “yes” to the pain relief question. When asked whether they would have the procedure again, 66.2% of respondents stated “yes”. Full survey results are listed in Table 1.
Discussion
This simple questionnaire study showed, from the patient perspective, that treating compression fractures by balloon kyphoplasty is a tolerable procedure that results in subjective pain relief. Based on our findings, most patients’ perspective on kyphoplasty is that given another compression fracture, they would opt for re-operation in the form of kyphoplasty.
Since the two studies in 2009 that showed no benefit of vertebroplasty over sham surgery, there have been large studies specifically regarding kyphoplasty which have contradicted this finding. While there have been many smaller non-randomized studies (8,14), two major studies (6,7) and a systematic review (16) have shown objective decrease in pain, improvement of quality of life and decrease in physical disability from kyphoplasty as compared to conservative management (6,7).
The patient population presented is similar to the only previous large kyphoplasty specific studies. The FREE trial had 149 patients in their kyphoplasty group of which 77% were female, the SWISS observational study 69.6% female, whereas our study contained 81% female. The average age of our patients was 74.0 while FREE had an average age of 72.2 and the SWISS study was 69.4.
Overall, 58.3% of patients had one fracture treated, compared with 67% for FREE and 77.1% for the SWISS study. The number of patients with two fractures treated was higher in our population at 27.8% than previously mentioned studies. Differences in these numbers may exist as many of our patients had more than one surgery within our four-year collection period, while the FREE study had only one surgical intervention, while it is not clear in the SWISS study if patients were treated in multiple surgeries. Most of the fractures treated were in a similar area to previous studies; 61.3% were treated at the thoracolumbar junction (T10–L2) in our respondents as compared to 59% in the FREE trial.
Our stratification of patients was similar to the stratification in the SWISS study. Spontaneous fracture was noted in 72.2% of our patients. Osteoporosis was noted in 83.5% of SWISS patients. Trauma was the cause in 14.6% of our patients, while the SWISS study had 12.2%. Finally, cancer or pathologic fracture was the cause of 7.3% of our patients and 4.3% of SWISS patients.
The FREE study also collected patient satisfaction data based on a 20-point Likert scale and noted statistical significance to from 1 to 24 months post operatively. The data presented here show similar results and attempt to build on the FREE results. The questionnaire used in this study was aimed at gathering additional and more specific patient-centered outcomes on kyphoplasty.
Our questionnaire is subject to recall bias. The patients who had procedures in 2008 were called in 2013, thereby introducing approximately 5 years between time of procedure and questionnaire administration. When breaking down the data to compare years, patients who had the procedure in 2008 had the same overall trend in answer choice, with one exception. Patients in 2008 responded “somewhat” to pain relief question 2 53.8%, and “yes” only 28.6% of the time. This trend was reversed in all following years. This finding could be a result of improved surgeon skill over time or recall bias as described above. A perceived limitation of this study may be the lack of objective data such as ODI, RM scale, VAS scale, but we were only attempting to elicit the patients’ individual perspective using patient-centered outcome data.
Since kyphoplasty’s inception, a rocky road has lead from individual anecdotal success to large randomized and observational evidence supporting its use in selected populations. In a changing healthcare environment, it is paramount that patient satisfaction is high among selected procedures. Our population of patients has now shown that kyphoplasty is also well-tolerated, effective, and desirable, based on individual patient perspective.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gailbert P, Deramond H, Rosat P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987;33:166-8. [PubMed]
- Lieberman IH, Dudeney S, Reinhardt MK, et al. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine 2001;26:1631-8. [Crossref] [PubMed]
- Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009;361:557-68. [Crossref] [PubMed]
- Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009;361:569-79. [Crossref] [PubMed]
- Goz V, Errico TJ, Weinreb JH, et al. Vertebroplasty and kyphoplasty: national outcomes and trends in utilization from 2005 through 2010. Spine J 2015;15:959-65. [Crossref] [PubMed]
- Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 2009;373:1016-24. [Crossref] [PubMed]
- Heubschle L, Borgstreom F, Olafsson G, et al. Real-life results of balloon kyphoplasty for vertebral compression fractures from the SWISS spine registry. Spine J 2014;14:2063-77. [Crossref] [PubMed]
- Dong R, Chen L, Tang T, et al. Pain reduction following vertebroplasty and kyphoplasty. Int Orthop 2013;37:83-7. [Crossref] [PubMed]
- Boonen S, Van Meirhaeghe J, Bastian L, et al. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 2011;26:1627-37. [Crossref] [PubMed]
- Chen AT, Cohen DB, Skolasky RL. Impact of Nonoperative Treatment, Vertebroplasty, and Kyphoplasty on Survival and Morbidity After Vertebral Compression Fracture in the Medicare Population. J Bone Joint Surg Am 2013;95:1729-36. [Crossref] [PubMed]
- Edidin AA, Ong KL, Lau E, et al. Mortality Risk for Operated and Nonoperated Vertebral Fracture Patients in the Medicare Population. J Bone Miner Res 2011;26:1617-26. [Crossref] [PubMed]
- Lange A, Kasperk C, Alvares L, et al. Survival and Cost Comparison of Kyphoplasty and Percutaneous Vertebroplasty Using German Claims Data. Spine 2014;39:318-26. [Crossref] [PubMed]
- Berenson J, Pflugmacher R, Jarzem P, et al. Cancer Patient Fracture Evaluation (CAFE. Investigators. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol 2011;12:225-35. [Crossref] [PubMed]
- Grafe IA, Da Fonseca K, Hillmeier J, et al. Reduction of pain and fracture incidence after kyphoplasty: 1-year outcomes of a prospective controlled trial of patients with primary osteoporosis. Osteoporos Int 2005;16:2005-12. [Crossref] [PubMed]
- Kasperk C, Hillmeier J, Nöldge G, et al. Treatment of painful vertebral fractures by kyphoplasty in patients with primary osteoporosis: a prospective nonrandomized controlled study. J Bone Miner Res 2005;20:604-12. [Crossref] [PubMed]
- Papanastassiou ID, Phillips FM, Van Meirhaeghe J, et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J 2012;21:1826-43. [Crossref] [PubMed]


