
Hypothyroidism increases 90-day postoperative complications in patients undergoing primary single level anterior cervical disectomy and fusion: a matched control analysis
Introduction
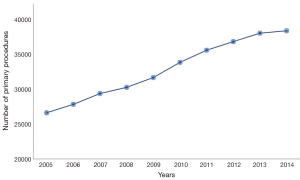
Anterior cervical discectomy and fusion (ACDF) is a proposed treatment for patients suffering from cervical radiculopathy or myelopathy (1). Current data trends have revealed that from 2006–2014 there were 1,059,403 primary ACDF procedures performed in the United States (2,3). In a national trends study performed by Marawar et al., there was almost an 8-fold increase in utilization of ACDF in the population (23/100,000 civilians to 157/100,000 civilians) over a 15-year period, from 1990–2004 (4). These trends were also seen by looking at the annual rates of ACDF performed in the Medicare population (Figure 1). The calculated annual growth rate (CAGR) was found to be 4.14% from 2005–2014 for primary ACDF procedures performed in the Medicare population. Despite the positive outcomes following this procedure, as with any surgical procedure, postoperative complications are inevitable.
The goal of any surgical planning should include identification of preoperative risk factors to reduce peri- and postoperative complications (5). Commonly known risk factors include: increasing age, high body mass index (BMI), tobacco usage, poor nutritional status, chronic obstructive pulmonary disease (COPD), illicit drug use, and poor nutritional status (6). Endocrinopathies such as diabetes and thyroid dysfunction can impact recovery following surgery (7,8). In a recent study by Rodondi et al. in 2005, the prevalence of the hypothyroidism was found to be 12.4% (8). This highlights how the prevalence of hypothyroidism has increased nearly 300% from 1988–2005. In this study, the prevalence of hypothyroidism was found to be 23.5% within the Medicare population.
Although the prevalence of patients undergoing primary ACDF and hypothyroid diagnoses are both increasing, the effect of hypothyroidism on postoperative complications in patients undergoing primary single-level ACDF is not well understood. The purpose of this study was to determine whether patients with hypothyroidism are at greater odds of: (I) developing 90-day medical complications; (II) 90-day readmission rates; and (III) incur greater total global 90-day episode of care costs compared to patients without hypothyroidism. We hypothesize that the patients with clinical hypothyroidism are at increased odds of developing postoperative complications than those patients without hypothyroidism, in addition to higher 90-day readmission rates and greater reimbursement rates.
Methods
A retrospective review from 2005–2014, was performed using the Medicare Standard Analytical Files from the Pearl Diver supercomputer (Pearl Diver Technologies, Fort Wayne, IN). Pearl Diver is compliant with the Health Information Portability and Affordability Act (HIPAA) and contains the records of over 100 million patients. The database allows institutions information such as diagnosis, procedures, length of stay, charges, reimbursements, and complications. Patients were queried using the International Classification of Disease, ninth revision (ICD-9) codes.
The inclusion criteria included all patients who underwent primary ACDF using the ICD-9 procedure code 81.02. All patients in the database with a prior diagnosis of hypothyroidism and diagnosis on the day of their ACDF were queried, and served as the study group. All patients without a diagnosis of hypothyroidism undergoing an ACDF served as the control group. Patients in the study group were randomly matched to patients in the control group with respect to age, gender, and Charlson-Comorbidity Index (CCI). CCI, a measurement of morbidity and mortality risk associated with worse outcomes following orthopedic surgery, was the parameter used to determine the similarity between the study group and control group (7). After the matching process, two mutually exclusive cohorts were formed and were followed for 90 days to determine the incidence of complications between both groups. Complications within the 90-day postoperative period were examined as hospitals are held accountable during this period for all Medicare payments per the Comprehensive Care for Joint Replacement (CJR) model (9). Excluding readmission rates for physical and occupational therapy, an adjusted relative risk (aRR) was calculated for readmission rates. Cost of care on the day of surgery along with 90-day cost of care was also compared between the cohorts.
Descriptive and statistical analyses was performed using the programming language R (University of Auckland, New Zealand). Univariate analysis with the use of odds ratios (OR), along with their respective 95% confidence interval (95% CI), and P values were used in our study. Significance was defined as P<0.05.
Results
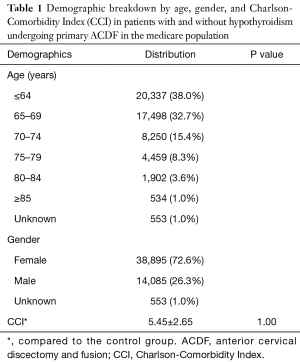
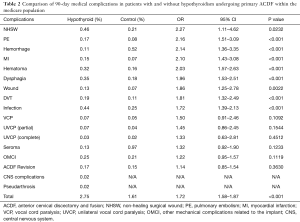
After the matching process, 107,066 patients met the inclusion criteria and were, split into those with hypothyroidism (n=53,533) and those without (n=53,533) the diagnosis (Table 1). CCI between the study group and control group was 5.45±2.65 with a P value of 1.00 indicating no difference between the groups. Patients with hypothyroidism undergoing ACDF were found to have greater total odds and incidence of postoperative complications than euthyroid patients 90 days following primary ACDF (2.75% vs. 1.61%; OR: 1.72; 95% CI: 1.58–1.87; P<0.001) (Table 2). Hypothyroid patients had greater odds of developing a non-healing surgical wound (NHSW) (OR: 2.27; 95% CI: 1.11–4.62; P=0.0232), pulmonary embolism (OR: 2.16; 95% CI: 1.51–3.09; P<0.001), and hemorrhage (OR: 2.14; 95% CI: 1.36–3.35; P<0.001) compared to patients without hypothyroidism.
Full table
Full table
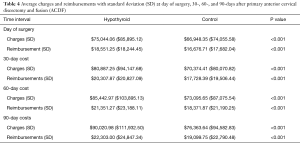
Readmission rates for hypothyroid patients were higher than the control group at each of the time intervals examined (Table 3). Patients with hypothyroidism had greater total odds and incidence (20.61% vs. 14.15%; OR: 1.45; 95% CI: 1.41–1.49; P<0.001) of readmission rates within the first 90 days following primary ACDF, compared to patients in the control group. Cost of care in patients with hypothyroidism was found to be statistically greater day of surgery ($75,044.06 vs. $66,948.35, P<0.001), 30-day ($80,887.25 vs. $70,374.41, P<0.001), 60-day ($85,442.97 vs. $73,095.65, P<0.001), and 90-day ($90,020.98 vs. $76,363.64, P<0.001) compared to patients without hypothyroidism undergoing primary ACDF (Table 4).

Full table
Full table
Discussion
ACDF is commonly indicated for patients suffering from cervical radiculopathy that has not resolved from conservative treatment with nonsteroidal anti-inflammatory drugs, physical therapy, or injection of cervical corticosteroids. Annual trends show the number of ACDF procedures being performed each year are increasing, as is the incidence of hypothyroidism (2,3). This study illustrates hypothyroidism as a modifiable risk factor for decreasing postoperative complications following primary ACDF, and is consistent with the current literature citing the significance of hypothyroidism on postoperative outcomes (10-14).
A database study utilizing the National Hospital Discharge Survey (NHDS) performed by Danescu et al. found that patients 60 years and older with hypothyroidism had a greater relative risk (RR) of DVT (RR: 2.23; 95% CI: 2.22–2.25) and PE (RR: 1.94; 95% CI: 1.92–1.96) compared to the control population (15). This finding is consistent with the findings of our study. Müller et al. found that 42 patients with hypothyroidism had higher levels of von Willebrand factor compared to patients in his control group (16). Another study performed by Cantürk et al. found patients with hypothyroidism presented with elevated levels of fibrinogen, factor VII, plasminogen activating inhibitor-1 (PAI-1), and decreased anti-thrombin III levels, which are associated with the development of thromboembolic and atheroscelerotic events (17). In a recent study of 214 patients, Tang et al. found that preoperative expression of PAI-1 was a risk factor for the development of DVTs in patients following total hip arthroplasty (OR: 1.18; 95% CI: 1.04–1.29; P=0.011) (18). Müller et al. discovered that supplementation of thyroid hormone decreased levels of factor VIII and PAI-1, thus reducing the incidence of DVTs in patients; suggestive that thyroid hormones within reference range have a protective effect against development of DVTs (16). Hypothyroidism is also associated with elevated levels of C-reactive protein (CRP) and triglyceride levels, both of which have been shown to be increase the risk of DVT (16-18).
Furthermore, wound and infection rates were also higher in the study cohort compared to the control group. In a recent animal study, total thyroidectomy performed on rats was done followed by midline abdominal incisions and of suturing the wound (19). Assays of rats with hypothyroidism had decreased type-IV collagen and hydroxyproline during the proliferative phase of wound healing (20). Oral triiodothyronine (T3) and thyroxine (T4) have been shown to promote wound healing and improve quality of wounds and increase tensile strength (21,22) Thyroid hormones have been shown to have a protective effect on the epidermal and dermal layers following surgery, by accelerating barrier formation by serving as a catalyst for enzymes in cholesterol sulfate cycle, and hypothyroidism may hinder the epidermal barrier function (22,23). Hypothyroidism also affects synthesis of lamellar granules known as Odland bodies, vital for establishment of normal stratum corneum. In tissue culture studies, triiodothyronine has been shown to directly stimulate proliferation of both epidermal keratinocytes and dermal fibroblasts. Tan et al. found hypothyroidism to be a modifiable condition, which predisposed patients undergoing primary total joint arthroplasty to infections (24). In their study, the microorganism profile most commonly affecting their study population was vancomycin-resistant Enterococcus, methicillin-resistant Staphylococcus Aureus, and coagulase-negative Staphylococcus Aureus (24).
Finally, this study demonstrates that hypothyroid patients ensue higher day of care, 30-, 60-, and 90-day costs (Table 4). Secondary to the results of this study, it can easily be implied that these higher costs are related to increased complication rates in this population. Dasta et al. calculated that patients with DVT and PE incurred an additional charge of $1,594 and $1,735 per hospitalization day, respectively. Depending on the degree of the severity, patients with DVT or PE required more expensive care compared to patients without these complications (25). Moreover, surgical site infections (SSI) were also higher in our study group and recent studies show that patients with SSI incurred an additional charge of $52,620 compared to patients without SSI (26). In this study, patients with hypothyroidism had an excess charge of $13,657.34±$17,349.67 within 90 days of their procedure, compared to their counterparts (Table 4).
As most large database studies, this review relies heavily on accurate procedural and diagnosis coding, translating to the fact that miscoding and noncoding by providers is a potential source of error. Currently, it is estimated that 1.3% of coding errors are present within the Medicare population (27). Additionally, the study only looked at a single insurer’s database, and may not be an accurate representation of patients with hypothyroidism in the United States. Moreover, a selection bias may be present as patients in the study may enter or exit the database as a natural manifestation (28). Lastly, patients undergoing multilevel ACDF are prone to greater complications compared to a single level, however due to the nature of our study it was not possible for us to numerically differentiate the number of levels operated on, as there is not a different ICD-9 code for multilevel ACDF (1,29).
Conclusions
Various studies have highlighted the increasing prevalence of hypothyroidism, which has been shown to increase in incidence as patients’ age. Concurrently, rates of primary ACDF are also increasing within the general population. This study highlights the complications which can arise in patients with hypothyroidism undergoing primary ACDF. The study can serve as another educational tool for physicians to be cognizant of this endocrinopathy and its surgical impact. Furthermore, it can be used to educate hypothyroid patients on the potential complications of ACDF. Optimization of thyroid function preoperatively can minimize the potential complications of ACDF in hypothyroid patients. Future prospective studies should aim at stratifying patients based on thyroid-stimulating hormone (TSH) levels, T3, and T4 and comparing postoperative complications following various orthopedic procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Due to the retrospective nature of the study, i.e., via a HIPAA compliant database without patient identifiers—no Institutional Review Board (IRB) approval was needed.
References
- Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310-7. [Crossref] [PubMed]
- Xie JC, Hurlbert RJ. Discectomy versus discectomy with fusion versus discectomy with fusion and instrumentation: a prospective randomized study. Neurosurgery 2007;61:107-16; discussion 116-7. [Crossref] [PubMed]
- Saifi C, Fein AW, Cazzulino A, et al. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J 2018;18:1022-9. [Crossref] [PubMed]
- Marawar S, Girardi FP, Sama AA, et al. National trends in anterior cervical fusion procedures. Spine (Phila Pa 1976) 2010;35:1454-9. [Crossref] [PubMed]
- Lim S, Kesavabhotla K, Cybulski GR, et al. Predictors for Airway Complications Following Single- and Multilevel Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:379-84. [Crossref] [PubMed]
- Ling XW, Howe TS, Koh JS, et al. Preoperative thyroid dysfunction predicts 30-day postoperative complications in elderly patients with hip fracture. Geriatr Orthop Surg Rehabil 2013;4:43-9. [Crossref] [PubMed]
- Wukich DK. Diabetes and its negative impact on outcomes in orthopaedic surgery. World J Orthop 2015;6:331-9. [Crossref] [PubMed]
- Rodondi N, Newman AB, Vittinghoff E, et al. Subclinical hypothyroidism and the risk of heart failure, other cardiovascular events, and death. Arch Intern Med 2005;165:2460-6. [Crossref] [PubMed]
- Ellimoottil C, Ryan AM, Hou H, et al. Implications of the Definition of an Episode of Care Used in the Comprehensive Care for Joint Replacement Model. JAMA Surg 2017;152:49-54. [Crossref] [PubMed]
- Voskuijl T, Hageman M, Ring D. Higher Charlson Comorbidity Index Scores are associated with readmission after orthopaedic surgery. Clin Orthop Relat Res 2014;472:1638-44. [Crossref] [PubMed]
- Hostiuc M, Curca GC, Dermengiu D, et al. Can subclinical hypothyroidism explain some sudden deaths due to pulmonary embolism without evident risk factors? Med Hypotheses 2011;76:855-7. [Crossref] [PubMed]
- Pingitore A, Chen Y, Gerdes AM, et al. Acute myocardial infarction and thyroid function: new pathophysiological and therapeutic perspectives. Ann Med 2012;44:745-57. [Crossref] [PubMed]
- Yaylali O, Kirac S, Yilmaz M, et al. Does hypothyroidism affect gastrointestinal motility? Gastroenterol Res Pract 2009;2009. [Crossref] [PubMed]
- Hostiuc S, Capatina CO, Sinescu CJ, et al. Lethal pulmonary thromboembolism associated with decreased thyroid hormone levels. Arch Endocrinol Metab 2015;59:355-8. [Crossref] [PubMed]
- Danescu LG, Badshah A, Danescu SC, et al. Venous thromboembolism in patients hospitalized with thyroid dysfunction. Clin Appl Thromb Hemost 2009;15:676-80. [Crossref] [PubMed]
- Müller B, Tsakiris DA, Roth CB, et al. Haemostatic profile in hypothyroidism as potential risk factor for vascular or thrombotic disease. Eur J Clin Invest 2001;31:131-7. [Crossref] [PubMed]
- Cantürk Z, Cetinarslan B, Tarkun I, et al. Hemostatic system as a risk factor for cardiovascular disease in women with subclinical hypothyroidism. Thyroid 2003;13:971-7. [Crossref] [PubMed]
- Tang J, Zhu W, Mei X, et al. Plasminogen activator inhibitor-1: a risk factor for deep vein thrombosis after total hip arthroplasty. J Orthop Surg Res 2018;13:8. [Crossref] [PubMed]
- Folsom AR, Lutsey PL, Astor BC, et al. C-reactive protein and venous thromboembolism. A prospective investigation in the ARIC cohort. Thromb Haemost 2009;102:615-9. [PubMed]
- Doggen CJ, Smith NL, Lemaitre RN, et al. Serum lipid levels and the risk of venous thrombosis. Arterioscler Thromb Vasc Biol 2004;24:1970-5. [Crossref] [PubMed]
- Holst AG, Jensen G, Prescott E. Risk factors for venous thromboembolism: results from the Copenhagen City Heart Study. Circulation 2010;121:1896-903. [Crossref] [PubMed]
- Natori J, Shimizu K, Nagahama M, et al. The influence of hypothyroidism on wound healing. An experimental study. Nihon Ika Daigaku Zasshi 1999;66:176-80. [Crossref] [PubMed]
- Safer JD. Thyroid hormone and wound healing. J Thyroid Res 2013;2013. [Crossref] [PubMed]
- Tan TL, Rajeswaran H, Haddad S, et al. Increased Risk of Periprosthetic Joint Infections in Patients With Hypothyroidism Undergoing Total Joint Arthroplasty. J Arthroplasty 2016;31:868-71. [Crossref] [PubMed]
- Dasta JF, Pilon D, Mody SH, et al. Daily hospitalization costs in patients with deep vein thrombosis or pulmonary embolism treated with anticoagulant therapy. Thromb Res 2015;135:303-10. [Crossref] [PubMed]
- Schweizer ML, Cullen JJ, Perencevich EN, et al. Costs Associated With Surgical Site Infections in Veterans Affairs Hospitals. JAMA Surg 2014;149:575-81. [Crossref] [PubMed]
- Cancienne JM, Dempsey IJ, Holzgrefe RE, et al. Is Hepatitis C Infection Associated With a Higher Risk of Complications After Total Shoulder Arthroplasty? Clin Orthop Relat Res 2016;474:2664-9. [Crossref] [PubMed]
- Burrus MT, Werner BC, Cancienne JM, et al. Shoulder arthroplasty in patients with Parkinson's disease is associated with increased complications. J Shoulder Elbow Surg 2015;24:1881-7. [Crossref] [PubMed]
- Wu XD, Wang XW, Yuan W, et al. The effect of multilevel anterior cervical fusion on neck motion. Eur Spine J 2012;21:1368-73. [Crossref] [PubMed]


