Disc herniation caused by a viscoelastic nucleus after total lumbar disc replacement—a case report
Introduction
Degenerative disc disease (DDD) is highly prevalent and is progressing over time (1). DDD alters biomechanical characteristics of intervertebral discs (IVD) and hence the motion segment is affected (2,3). Degenerated discs that cause back pain may be treated surgically if conservative treatment fails. Traditionally, fusion procedures are performed (4). Total disc replacement (TDR) is an alternative for a specific subset of patients—namely those with discogenic back pain without clinical signs of a facet syndrome. The clinical outcome of TDR may be superior to conservative treatment or fusion in patients with DDD (5,6). Furthermore, TDR should decrease the risk of adjacent segment disease (7). In a recent study, TDR was associated with a significantly decreased risk for complications in the early phase after surgery (8). According to a survey, spine surgeons raised concerns about revision procedures and long-term outcome after TDR (9). Here we describe an unreported complication of an artificial lumbar disc herniation caused by a viscoelastic nucleus after TDR.
Case presentation
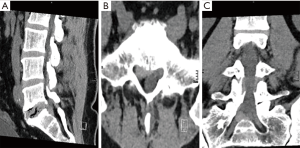
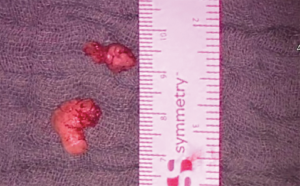
An otherwise healthy 34-year-old male presented to our department with an acute S1-syndrome on the right side. He had undergone TDR (Cadisc-L; Ranier Technology Ltd.; Cambridge, UK) at the level L5/S1 more than 2 years prior to this episode at another hospital. Computer tomography of the lumbar spine revealed an intraspinal mass at the prior TDR level (Figure 1). The patient underwent microscopic sequestrectomy. Intraoperatively, a viscoelastic structure mimicking a regular disc herniation was found to compromise the S1 root and was subsequently removed (Figure 2). Postoperatively, the radiculopathy resolved completely.
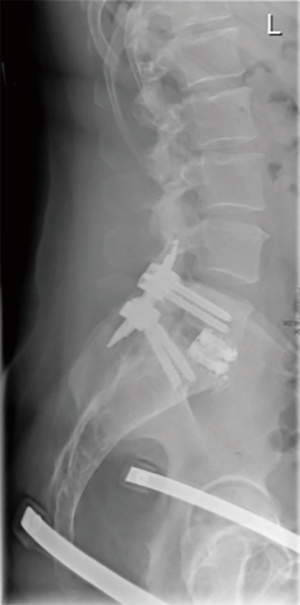
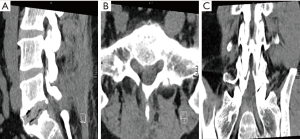
However, 3 weeks later he presented again with similar symptoms. Imaging studies showed again an intraspinal mass (Figure 3). Another surgery was performed. Further, TDR was removed and replaced by an interbody fusion cage via a transperitoneal approach. Additionally, dorsal lumbar instrumentation was performed (Figure 4). The patient’s condition is currently routinely followed-up. The radiculopathy has resolved, but the patient is now (2 years after fusion) experiencing adjacent segment disease with facet syndromes cranially to the instrumentation.
Discussion
DDD affects up to 40% of all patients with low back pain (4). Altered biomechanical properties eventually lead to spinal instability (2-4). TDR might be a valuable alternative to fusion procedures for some patients (10). Theoretically, TDR should decrease the risk of adjacent segment disease by maintaining range of motion (4,11). First clinical results have demonstrated this risk reduction in the clinical setting (12). Additionally, the effect on adjacent facet joints is minimal according to biomechanical investigations (13). Today numerous devices are available.
The Cadisc-L device is an elastomeric, monobloc disc prosthesis. It derives from a polyurethane-polycarbonate polymer with hard end plates and an internal structure consisting of a soft nucleus surrounded by a harder annulus (14). The design aims to mimic biomechanical and motion properties of IVD more physiologically (14,15). In a biomechanical study, this device caused a reduction in axial stiffness, but was able to maintain disc height and flexion stiffness within a physiological range (15). We are not aware of a published clinical outcome study. Clinical experience with a similar device has been published recently with a 2-year follow-up after cervical TDR (16).
In general, appropriate patient selection remains crucial, as several predictors favoring surgical or conservative treatment options have been identified (17). TDR might be statistically superior to fusion in some aspects (6). The reduction or prevention of adjacent segment disease needs to be studied appropriately as there is still weak evidence available (7,10,18). Concerns about revisions and long-term outcome after TDR remain among spine surgeons (9,19). So far, TDR has not been implemented at a large scale (10,18).
At the lumbar level, microdiscectomy or microscopic sequestrectomy may be performed routinely, if conservative treatment fails in patients with herniated discs. Both treatment options are comparable, with some studies favoring sequestrectomy in the mid-term clinical follow-up (20). In the clinical management of this patient, lumbar sequestrectomy alone was obviously insufficient. Hence, as advocated by others interbody fusion should be considered as the primary option for failure of TDR (6). Noteworthy fusion tends to increase intradiscal pressure in adjacent segments and range of motion in non-fused segments (21). These biomechanical observations may contribute to the adjacent segment disease and facet syndromes in this case.
We agree with previous reports that delayed development or reoccurrence of pain with or without neurologic impairment should lead to early imaging studies in order to rule out a mass effect compromising neural structures (22). Although anterior dislocation after TDR has been described (23), we are not aware of previously reported posterior dislocation of the viscoelastic nucleus after TDR as seen in our patient. Despite the fact that the device has been removed from the market, we strongly believe that this report is relevant for spine surgeons as multiple devices have been implanted and similar devices are still available.
Conclusions
In summary, we present a to the best of our knowledge unreported complication after TDR with a very distinct failure mode due to the device design. Since there are only a few long-term outcome studies available (24), spine surgeons should be able to recognize and respond to similar complications appropriately.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Waris E, Eskelin M, Hermunen H, et al. Disc degeneration in low back pain: a 17-year follow-up study using magnetic resonance imaging. Spine (Phila Pa 1976) 2007;32:681-4. [Crossref] [PubMed]
- Burton AK, Battie MC, Gibbons L, et al. Lumbar disc degeneration and sagittal flexibility. J Spinal Disord 1996;9:418-24. [Crossref] [PubMed]
- Mimura M, Panjabi MM, Oxland TR, et al. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine (Phila Pa 1976) 1994;19:1371-80. [Crossref] [PubMed]
- Shedid D, Ugokwe KT, Benzel EC. Lumbar total disc replacement compared with spinal fusion: treatment choice and evaluation of outcome. Nat Clin Pract Neurol 2005;1:4-5. [Crossref] [PubMed]
- Hellum C, Berg L, Gjertsen O, et al. Adjacent level degeneration and facet arthropathy after disc prosthesis surgery or rehabilitation in patients with chronic low back pain and degenerative disc: second report of a randomized study. Spine (Phila Pa 1976) 2012;37:2063-73. [Crossref] [PubMed]
- Wei J, Song Y, Sun L, et al. Comparison of artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Int Orthop 2013;37:1315-25. [Crossref] [PubMed]
- Wang JC, Arnold PM, Hermsmeyer JT, et al. Do lumbar motion preserving devices reduce the risk of adjacent segment pathology compared with fusion surgery? A systematic review. Spine (Phila Pa 1976) 2012;37:S133-43. [Crossref] [PubMed]
- Eliasberg CD, Kelly MP, Ajiboye RM, et al. Complications and Rates of Subsequent Lumbar Surgery Following Lumbar Total Disc Arthroplasty and Lumbar Fusion. Spine (Phila Pa 1976) 2016;41:173-81. [Crossref] [PubMed]
- Whang PG, Simpson AK, Rechtine G, et al. Current trends in spinal arthroplasty: an assessment of surgeon practices and attitudes regarding cervical and lumbar disk replacement. J Spinal Disord Tech 2009;22:26-33. [Crossref] [PubMed]
- Ding F, Jia Z, Zhao Z, et al. Total disc replacement versus fusion for lumbar degenerative disc disease: a systematic review of overlapping meta-analyses. Eur Spine J 2017;26:806-15. [Crossref] [PubMed]
- Pitzen T, Kettler A, Drumm J, et al. Cervical spine disc prosthesis: radiographic, biomechanical and morphological post mortal findings 12 weeks after implantation. A retrieval example. Eur Spine J 2007;16:1015-20. [Crossref] [PubMed]
- Zigler JE, Glenn J, Delamarter RB. Five-year adjacent-level degenerative changes in patients with single-level disease treated using lumbar total disc replacement with ProDisc-L versus circumferential fusion. J Neurosurg Spine 2012;17:504-11. [Crossref] [PubMed]
- Gao SG, Lei GH, He HB, et al. Biomechanical comparison of lumbar total disc arthroplasty, discectomy, and fusion: effect on adjacent-level disc pressure and facet joint force. J Neurosurg Spine 2011;15:507-14. [Crossref] [PubMed]
- Mahomed A, Moghadas PM, Shepherd DE, et al. Effect of axial load on the flexural properties of an elastomeric total disc replacement. Spine (Phila Pa 1976) 2012;37:E908-12. [Crossref] [PubMed]
- McNally D, Naylor J, Johnson S. An in vitro biomechanical comparison of Cadisc-L with natural lumbar discs in axial compression and sagittal flexion. Eur Spine J 2012;21 Suppl 5:S612-7. [Crossref] [PubMed]
- Chin KR, Lubinski JR, Zimmers KB, et al. Clinical experience and two-year follow-up with a one-piece viscoelastic cervical total disc replacement. J Spine Surg 2017;3:630-40. [Crossref] [PubMed]
- Hellum C, Johnsen LG, Gjertsen O, et al. Predictors of outcome after surgery with disc prosthesis and rehabilitation in patients with chronic low back pain and degenerative disc: 2-year follow-up. Eur Spine J 2012;21:681-90. [Crossref] [PubMed]
- Jacobs WC, van der Gaag NA, Kruyt MC, et al. Total disc replacement for chronic discogenic low back pain: a Cochrane review. Spine (Phila Pa 1976) 2013;38:24-36. [Crossref] [PubMed]
- Park CK. Lumbar total disc replacement: does it still need further follow-up? J Spine Surg 2017;3:460-2. [Crossref] [PubMed]
- Barth M, Weiss C, Thome C. Two-year outcome after lumbar microdiscectomy versus microscopic sequestrectomy: part 1: evaluation of clinical outcome. Spine (Phila Pa 1976) 2008;33:265-72. [Crossref] [PubMed]
- Weinhoffer SL, Guyer RD, Herbert M, et al. Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine (Phila Pa 1976) 1995;20:526-31. [Crossref] [PubMed]
- Guyer RD, Shellock J, MacLennan B, et al. Early failure of metal-on-metal artificial disc prostheses associated with lymphocytic reaction: diagnosis and treatment experience in four cases. Spine (Phila Pa 1976) 2011;36:E492-7. [Crossref] [PubMed]
- Gragnaniello C, Seex KA, Eisermann LG, et al. Early postoperative dislocation of the anterior Maverick lumbar disc prosthesis: report of 2 cases. J Neurosurg Spine 2013;19:191-6. [Crossref] [PubMed]
- Siepe CJ, Heider F, Wiechert K, et al. Mid- to long-term results of total lumbar disc replacement: a prospective analysis with 5- to 10-year follow-up. Spine J 2014;14:1417-31. [Crossref] [PubMed]