Delayed surgery in neurologically intact patients affected by thoraco-lumbar junction burst fractures: to reduce pain and improve quality of life
Introduction
Thoraco-lumbar junction burst fractures (TLJBF) are the most common fractures of the spine (1).
In TLJBF the established indications for surgery are: patients affected by neurological deficits, massive height reduction of the vertebral body, severe kyphosis, severe reduction of the spinal canal, spinal instability. On the other hand, there are cases in which the patient is neurologically intact with no or minimum kyphosis, slight reduction of the spinal canal and moderate pain.
Currently there is no consensus regarding what is the best treatment in these cases. In our experience the clinical follow-up assumes a relevant importance in order to re-assess the patient in the following months.
Herein we report a series of 18 consecutive patients who presented to our Emergency Department for spinal trauma and radiological images demonstrated an A3 or A4 TLJBF according to AOSpine thoracolumbar spine injury classification system by Vaccaro et al. of 2013 (2). All the patients were neurologically intact, with no or minimum kyphosis or canal invasion; the pain was moderate. A conservative management was the treatment of choice and a strict clinical follow-up was arranged. Those patients who still presented pain at 3–4 months of follow-up underwent surgery. The outcome in terms of pain and quality of life has been analyzed comparing the preoperative and postoperative results.
Methods
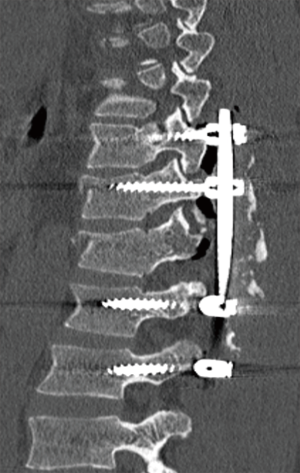
A retrospective study on 18 patients who referred to the Emergency Department of our hospital is reported. Patients included in this series were neurologically intact and affected by a TLJBF A3 or A4 at computed tomography (CT) scan, the height of the bursted vertebral body was >50%, the spinal canal invasion was <30% and the kyphosis deformity <30 degrees. Patients with multiple vertebral fractures or other several injuries after the trauma were excluded. In all the cases a conservative treatment with a brace was established, afterwards the patients were gradually mobilized and periodically followed-up in clinic for a clinical and radiological assessment. Standing thoraco-lumbar X-ray in anterior and lateral projections were executed to assess the kyphosis. Patients with a worsening kyphosis major than 30 degrees were excluded from the study. Pain and quality of life were assessed using the scores at the graphic rating scale (GRS) (3) and EuroQol (EQ-5D) (4) on admission and every month after the injury at clinical follow-up. Patients included in this study were those operated at 3–4 months after the injury since complaining pain at the clinical follow-up. In all the cases the fracture involved Th12 or L1, the spinal canal was decompressed at the level of the fracture and a posterior fixation 2 levels above and 2 levels below the fracture level was executed using pedicle screws and rods (Figure 1). In the postoperative period the patients were gradually mobilized and discharged. A follow-up in clinic was arranged and the pain was re-assessed using the GRS scores at 1, 2, 3, 6, 12 months.
An informed consent from the patients was obtained; this study respects the ethical standards in the Helsinky Declaration of 1975, as revised in 2000, as well as the national law.
Statistical analysis plan
We investigated the differences in pain and quality of life in pre- and post-surgical period. T-tests using the EQ5D and EQ5D-VAS scores in pre-surgical and post-surgical period were performed. A repeated measure analysis of variance was executed using the GRS assessed at 1, 2, 3 and 4 months before surgery and at 1, 2, 3 and 12 months after surgery.
The level of significance for all analyses was P=0.05. Statistical interpretation of the data was performed with SPSS version 19 software (SPSS Inc., Chicago, Illinois, USA).
Results
Eighteen patients were included: 12 males (66.7%) and 6 females (33.3%) with a mean age of 50.11 (SD =12.57) at the diagnosis. The pre-surgical and post-surgical scores at GRS and EQ-5D for all the patients are presented in Table 1.
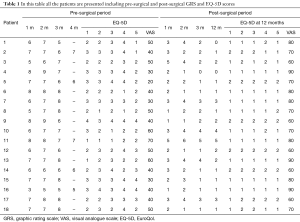
Full table
Both age and gender were not related with the scores considered in the following analysis. We obtained a mean score on EQ-5D (pre and post-surgery) that revealed a good internal reliability (respectively alpha =0.79 and 0.88).
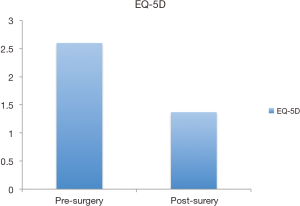
Two t-test were conducted in order to investigate the quality of life using both the EQ-5D scale and the EQ5D-VAS depending from surgery. Results showed that the score on the EQ-5D scale had a statistically significant decrease (P<0.001). The mean score on EQ-5D pre-surgery was 2.60 (SD =0.67) while the mean score on EQ-5D post-surgery was 1.37 (SD =0.41) (Figure 2).
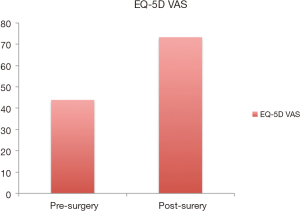
For what concern the score on EQ5D-VAS, the t-test revealed that surgery had a statistically significant effect (P<0.01) in improving the quality of life (EQ5D-VAS pre =43.89, SD =12.43 and EQ5D-VAS post =73.33, SD =10.84) (Figure 3).
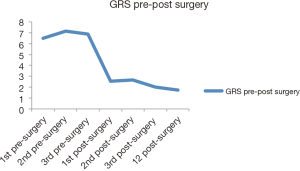
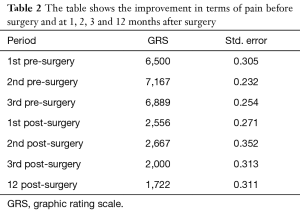
The pain was assessed using the GRS once a month for 3 months before the surgery and once a month for 3 months after surgery. Another GRS score was obtained at 12 months after surgery.
A repeated measures analysis of variances showed that the pain had a statistically significant increase from the first to second month before surgery (△=0.667, P<0.001) while no differences was found from the first to the third month (△=0.389, P=0.99). However, in pre-surgical and post-surgical months the pain decreased significantly with a maximum mean difference among the 2nd and 3rd month before surgery and at 12 months after surgery (respectively △=5.444, P<0.001 and △=5.167, P<0.001).
The results showed that pain did not show difference at 3 and 12 months after surgery (△=0.278, P=0.17) while during the post-surgical period there was a statistically significant improvement (reduction) in terms of pain (Table 2) (Figure 4).
Full table
A Pearson correlation among age and gender and EQ-5D scale, EQ5D-VAS (pre-post) and GRS revealed no significant correlation.
Discussion
Traumatic fractures of the thoracolumbar spine, especially at the thoracolumbar junction, are the most common spinal column fractures. High activity and lack of stability make the thoracolumbar spine more prone to fracture (5).
The thoracolumbar injury classification and severity score (TLICS) is widely used, but progressive kyphotic deformity in conservatively managed TLJBF has been reported as the Achilles tendon (6).
In 2013 Vaccaro et al. proposed a new AOSpine thoracolumbar spine injury classification system in order to develop a widely accepted, comprehensive and simple classification system with clinically acceptable intra- and inter-observer reliability for use in both clinical practice and research. In addition to a morphological description, this system considered the neurological status and patient specific modifiers that are important for surgical decision making.
Herein we report a retrospective series of patients who according to this classification presented a TLJBF classified as A3 or A4 N0. The spinal canal invasion was <30%, kyphosis <30 degrees, vertebral body height >50% and the pain was moderate, so we decided for a strict clinical follow-up. Patients who presented a worsening kyphosis superior than 30 degrees were excluded from the study. Patients who complained pain at 3–4 months from the initial injury underwent surgical operation consisting in laminectomy at the fracture level and pedicle screws fixation 2 levels above and 2 levels below the fracture level. This series of patients was included in the study.
The aim of the operation was to decompress the spinal cord and stabilize the thoraco-lumbar spine in order to reduce the pain. In executing the laminectomy we extended into the foramen to decompress the adjacent nerve root. The fixation was executed with the aim to reduce the instability (considered a possible source of pain). The results were assessed analyzing pain and quality of life through the GRS scale and EQ-5D scores in pre and post-operative period.
Our results suggest that the surgery had a significant effect in reducing pain, as for the improvement of quality of life. Moreover, after an analysis of the GRS scores, a linear reduction of pain was also evident months after surgery.
The quality of life was investigated using both the EQ-5D scale and the EQ5D-VAS before and after the surgery. Comparing pre- and post-operative EQ-5D, the scores had a statistically significant decrease (P<0.001), since the mean score on EQ-5D pre-surgery was 2.60 (SD =0.67) while the mean score on EQ-5D post-surgery was 1.37 (SD =0.41).
Also analyzing the EQ5D-VAS score, the t-test revealed that surgery had a statistically significant effect (P<0.01) in improving the quality of life. (EQ5D-VAS pre =43.89, SD =12.43 and EQ5D-VAS post =73.33, SD =10.84).
In pre-surgical and post-surgical months the pain decreased significantly with the maximum mean difference among the 2nd and 3rd month before surgery and at 12 months after surgery (respectively D =5.444, P<0.001 and D =5.167, P<0.001).
Nevertheless the literature demonstrates that a conservative management for TLJBP is able to obtain good results.
Weinstein et al. (7) reported a series of patients with burst fractures treated non-operatively who had excellent results, with more than 80% able to resume their pre-trauma occupation.
Studies comparing operative and non-operative management of burst fracture concluded that even though short- and long-term radiological results may be better in the operative group, there is no significant difference in treatment outcome in terms of back pain and functionality between the groups (8-10).
Wood et al. (11) reported significantly lower pain scores in conservatively managed group than in the operative group.
Resch et al. (12) stated that all patients in the nonoperative group were satisfied, while 15% of the surgical group were unsatisfied with the outcome.
Hitchon et al. (13) reported a series of 68 neurologically intact patients with TLJBF initially treated conservatively with bracing and gradual mobilization. Owing to pain limiting mobilization, 18 patients failed nonoperative management and required instrumentation, but those who failed nonsurgical management were significantly more kyphotic and stenotic than those successfully treated nonoperatively.
In our experience these patients may still complain pain at the clinical follow-up and there is a lack of knowledge if surgery is indicated for these cases. To our knowledge this is the first study about pain and quality of life after decompression and thoraco-lumbar fixation in neurologically intact patients affected by TLJBF who underwent surgery at 3–4 months from the initial injury.
Our results demonstrate that surgery determined a significant reduction of pain and improvement of the quality of life.
Conclusions
In literature there is controversy regarding the pain may be an indication for surgery in TLJBF and series of patients successfully managed conservatively have been reported. Herein we report a series of patients still complaining pain at 3–4 months from the initial injury who underwent surgery. The surgical results show good results in terms of pain and quality of life in performing decompression at the fracture level and fixation 2 levels above and 2 levels below. We conclude that patients affected by TLJBF require a strict clinical follow-up since pain may be present in the following months and it affects the quality of life. Surgery should be considered for these cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: An informed consent from the patients was obtained; this study respects the ethical standards in the Helsinki Declaration of 1975, as revised in 2000, as well as the national law.
References
- Cahueque M, Cobar A, Zuñiga C, et al. Management of burst fractures in the thoracolumbar spine. J Orthop 2016;13:278-81. [Crossref] [PubMed]
- Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013;38:2028-37. [Crossref] [PubMed]
- Freyd M. The Graphic Rating Scale. J Educ Psychol 1923;14:83-102.
- Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337-43. [Crossref] [PubMed]
- Tang P, Long A, Shi T, et al. Analysis of the independent risk factors of neurologic deficit after thoracolumbar burst fracture. J Orthop Surg Res 2016;11:128. [Crossref] [PubMed]
- Mattei TA, Hanovnikian J, H, Dinh D. Progressive kyphotic deformity in comminuted burst fractures treated non-operatively: the Achilles tendon of the Thoracolumbar Injury Classification and Severity Score (TLICS). Eur Spine J 2014;23:2255-62. [Crossref] [PubMed]
- Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar ‘‘burst’’ fractures treated conservatively: a long-term follow-up. Spine (Phila Pa 1976) 1988;13:33-8. [Crossref] [PubMed]
- Knight RQ, Stornelli DP, Chan DP, et al. Comparison of operative versus nonoperative treatment of lumbar burst fractures. Clin Orthop Relat Res 1993.112-21. [PubMed]
- Domenicucci M, Preite R, Ramieri A, et al. Thoracolumbar fractures without neurological involvement: surgical or conservative treatment? J Neurosurg Sci 1996;40:1-10. [PubMed]
- Seybold EA, Sweeny CA, Fredrickson BE, et al. Functional outcome of low lumbar burst fractures. A multicenter review of operative and nonoperative treatment from L3–L5. Spine (Phila Pa 1976) 1999;24:2154-61. [Crossref] [PubMed]
- Wood K, Buttermann G, Mehbod A, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am 2003;85-A:773-81. [Crossref] [PubMed]
- Resch H, Rabl M, Klampfer H, et al. Surgical versus conservative treatment of fractures of the thoracolumbar transition. Unfallchirurg 2000;103:281-8. [Crossref] [PubMed]
- Hitchon PW, Abode-Iyamah K, Dahdaleh NS, et al. Nonoperative Management in Neurologically Intact Thoracolumbar Burst Fractures: Clinical and Radiographic Outcomes. Spine (Phila Pa 1976) 2016;41:483-9. [Crossref] [PubMed]