Spinal extradural angiolipoma: a report of two cases and review of literature
Introduction
Spinal extradural angiolipomas (SEAL) are extremely extraordinary benign extradural lesions. They constitute about 0.04–1.2% of all spinal axis tumors and about 2–3% of all extradural spinal tumors (1-4). SEALs are benign tumors comprising of both mature fatty tissue and anomalous vascular rudiments. The above features make these lesions clinically and pathologically unique (3,5). SEALs are classified into two subtypes: non-infiltrating and infiltrating (5-7). While the non-infiltrating types are more common and normally well encapsulated, the infiltrating types are sporadic, and usually unencapsulated with imprecise edges. They usually infiltrate nearby tissues, particularly the bone (3,6,8). The gold standard radiological diagnostic method is MRI while the gold standard treatment option is surgery (3,8). Patient usually attain good recovery as well as good prognosis with partial or total resection of the lesion (1,8). We present two cases of SEAL which we successfully surgical resected with no further neurological deficits.
Case presentation
Case 1
We present a case of 39-year-old woman with 6-month history of numbness at the low extremities. Her symptoms progressed very gradually until she noticed slight weakness in both limbs. She did not have urine or fecal incontinence. All other systems very grossly normal. On examination, all systems were grossly normal. The muscle bulk, power and reflexes on the upper limbs as well as the lower limbs were normal. However, pin pricks examinations revealed numbness at the T5–T7 dermatome levels. Digital rectal examination revealed normal sphincter tone. All other ancillary investigation [chest X-ray (CXR), electrocardiogram (ECG), etc.] as well as laboratory investigation were normal.
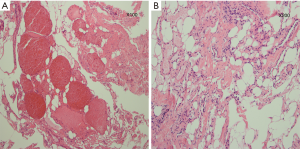
MRI done at facility revealed T5–T7 intrathoracic extradural spinal lesions. The lesion measured about 6.0 cm × 2.0 cm × 2.0 cm and located at the dorsal spinal cord. The lesion appeared as hyperintense on T2-weighted images and as heterogeneous iso-hyperintense on T1-weighted images. The lesion showed maximal enhancement after intravenous (IV) contrast administration. The lesion exerted compressive effect on the spinal cord from T5–T7. The vertebral bones were however spared by the lesion (Figure 1A,B,C). Our working diagnosis was spinal angiolipomas to rule out meningioma. After education and counselling of the patients and her relatives, operation was scheduled.
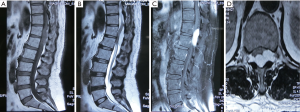
The goal of the operation was to decompress T5–T7 spinal nerve root via T5–T7 laminotomy as well as internal fixation. Intraoperatively, we found the lesion at the T5–T7 dorsal spinal cord. The lesion was at epidural space. It measured about 6.0 cm × 2.0 cm × 2.0 cm (Figure 1D). The lesion was yellow in color and tough in consistence with irregular margins. It had very rich blood supply. We achieved total resection after dissecting the tissue around the tumor. We carried out internal fixation to stabilize the spine. Postoperative MRI done revealed total resection of the tumor and the internal fixation well in place. The histopathological examination of the specimens obtained during operation showed that the lesion was made up of fatty tissue and angioma-like tissue (Figure 2A,B). The patient recovered very remarkably postoperative without any further neurological complication. The presenting symptoms resolved after the operation. The patient was discharged home two weeks after the operation. Three-year follow-up revealed massive improvement in her quality of life.
Case 2
Our second case is a 53-year-old man with 2-year history of numbness and pain at right lower extremity. His symptoms progressed very gradually until she could no longer walk. He also experienced severe backache with difficulty in passing urine as well as fecal incontinence. All other systems were essentially normal. On examination, all systems were grossly normal. The muscle bulk, power and reflexes on the upper limbs as well as the lower limbs were normal. However, pin pricks examinations revealed numbness at the T12–L1 dermatome levels. Digital rectal examination revealed a weak sphincter tone. All other ancillary investigation [chest X-ray (CXR), electrocardiogram (ECG), etc.] as well as laboratory investigation were normal.
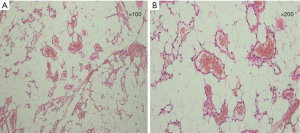
MRI done at facility revealed T12–L1 intrathoracic extradural spinal lesions. The lesion measured about 4 cm × 3 cm × 2 cm and located at the dorsal spinal cord. The lesion appeared as hyperintense on T2-weighted images and as heterogeneous iso-hyperintense on T1-weighted images. The lesion showed maximal enhancement after IV contrast administration. The lesion exerted compressive effect on the spinal cord from T12–L2. The vertebral bones were however not spared by the lesion (Figure 3). The tumor infiltrated the surrounding tissues as well as the bone. Our working diagnosis was spinal angiolipomas to rule out meningioma. After education and counselling of the patients and her relatives, operation was scheduled.
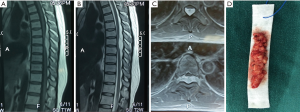
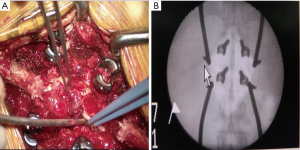
The goal of the operation again was to decompress T12–L1 spinal nerve root via T12–L1 laminotomy as well as internal fixation. Intraoperatively, we found the lesion at the T12–L1 dorsal spinal cord. The lesion was at epidural space. It measured about 4 cm × 3 cm × 2 cm. The lesion was yellow in color, tough in consistence with irregular margins as well as fat-like changes. It had very rich blood supply. We however observed that the tumor infiltrated the surrounding tissues as well as the bone. We attained total resection after dissecting the tissue around the tumor. We carried out internal fixation to stabilize the spine (Figure 4A). Postoperative MRI done revealed total resection of the tumor and the internal fixation well in place (Figure 4B). The histopathological examination of the specimens obtained during operation also showed that the lesion was made up of fatty tissue and angioma-like tissue (Figure 5A,B). This patient also recovered very remarkably postoperative without any further neurological complication. The presenting symptoms resolved after the operation. The patient was discharged home two weeks after the operation. One-year follow-up revealed massive improvement in her quality of life.
Discussion
SEALs are extremely rare benign extradural tumefactions. This lesion constitutes about 0.04–1.2% of all spinal axis neoplasms and 2–3% of all extradural spinal neoplasms (1-3,9). SEALs are classified into two types: “non-infiltrating” and “infiltrating” (6,10). Our cases comprise of a male and a female. The female patient in cases series above had a non-infiltrating type while the male patient had the infiltrating type. Studies have shown that majority of SEALs are non-infiltrating and do not invade the vertebra or adjacent tissues (1,4,10). Studies have further shown that the non-infiltrative SEALs have a female preponderance while the infiltrative types have equal male and female ratios (2,6). The female preponderance of the non-infiltrative SEALs is as a result of hormonal influence on the growth, continuance, or advancement of neoplasm (6,11). The ages of our cases range from 30–60 years. These ages are consistent with the average ages of patients initially reported in literature (40–60 years) (1,6,8). Spinal extradural non-infiltrative angiolipomas commonly originate from the posterior epidural space at the thoracic levels and typically extend over 3 to 4 vertebral bodies while that infiltrating types correspondingly are often situated at the thoracic levels (6,11,12). Although several single cases as well as case series have been document, the etiology and pathogenesis of SEALs are still not well exploited and for that matter not well understood. A few authors hypothesized that they originate from pluripotential mesenchymal stem cells with secretory activity (5,6).
The clinical presentations of SEALs are generally not different from any other benign spinal neoplasm. They mostly present with signs and symptoms of spinal cord compression as well as back pain (6,8,10,12). Idiosyncratic presentations are typically of sensory disorders as well as motor deficits below the level of the lesion that frequently advance to weakness in the lower limbs for long periods with sphincter dysfunction in the advanced stages (3). The manifestation of the sensory disorders often precedes the motor deficits since most SEALs are transcendently located in the dorsal part of the spinal cord. Precipitous onset or deteriorating of neurological symptoms arises when there is a fast upsurge in the size of the neoplasm. This usually due to intratumoral thrombosis, haemorrhage, or a steal phenomenon (3,13). Several patients present with a remitting and relapsing course of symptoms. These relapses are often linked to pregnancy (13).
Although plain X-ray imaging is outmoded, it is still very useful in facilities that do not have modern radiological diagnostic modalities. On plain X-ray, infiltrating tumors may mimic vertebral hemangioma with trabeculation of the affecting vertebral body (6,14). On CT however, SEALs are seen as low or intermediate-density masses. They are readily enhanced with IV contrast medium because of their rich vascular component (15). The gold standard radiological diagnosis is MRI. The MRI feature observed in our two cases is not different from what has been reported in literature. Studies have shown that SEALs are usually hyperintense and inhomogeneous on T1-weighted images with intense homogeneous enhancement, and hyperintense on T2-weighted images (3,6,8,15). The masses are usually bright on T1 and T2-weighted images (15). Another modern radiological modality that is used to the diagnose and treat of SEALs is angiography. This diagnostic modality is preferred in situations where hypointense foci are found on non-contrast T1-weighted images. In case like these, angiography can be done to explore further as well as aid in embolization treatment. Embolization of a highly vascularized SEALs can facilitate surgical removal (10).
The gold standard treatment modality for SEALs is surgical resection of the lesion via anterior approach or posterior laminectomy (6,8,11). We used posterior approach to access the tumor in our cases above. We attained total tumor resection in our cases. Total surgical removal of the tumor is usually the first-choice treatment modality for SEALs. However, total resection can be more difficult in the infiltrating types as compare to the non-infiltrative types. Some authors are of the view that total resection may be achievable only with an anterior approach. Nevertheless, even with subtotal removal, most patients have a good prognosis because the tumors are typically slow growing and do not undergo malignant changes (6,12). Furthermore, recurrence is very exceptional in SEALs. A combine treatment with surgery and radiotherapy has also been used by Gonzalez-Crussi et al. with success (10,16). Conversely, neither adjuvant chemotherapy nor radiotherapy is advocated as sole or combination treatment modality for these benign lesions, even when incomplete removal is attained (10). Non-encapsulated or rarely partially encapsulated tumor comprising of mature lipocytes with delicate proliferating blood vessels wedging haphazardly into the neighboring tissue is seen histologically (6,11). Furthermore, the ratio of fat to vessels is often capricious and varies from 1:3 to 2:3 (6). Pathologically, lesions with copious smooth muscle proliferation are subclassified as angiomyolipomas (6). The only difference between infiltrating and noninfiltrating types is that infiltrating angiolipoma is non-encapsulated. Atypia, pleomorphism, and mitotic figures of both adipose and angiomatous constituents are usually not seen (6,11).
Conclusions
The diagnosis of SEALs initially can be challenging radiologically since the may mimic the other spinal lesions. The gold standard treatment modality should always be surgery although total resection may not be achievable in some cases. We attained total resection in both cases without any further neurological complication. The prognosis of our cases is very good on follow-ups. Our patients regained their normal functions and are able to carry out their normal day to day activities. We have not observed recurrence of their lesions so far.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Gelabert-González M, García-Allut A. Spinal extradural angiolipoma: report of two cases and review of the literature. Eur Spine J 2009;18:324-35. [Crossref] [PubMed]
- Anson JA, Cybulski GR, Reyes M. Spinal extradural angiolipoma: a report of two cases and review of the literature. Surg Neurol 1990;34:173-8. [Crossref] [PubMed]
- Si Y, Wang Z, Pan Y, et al. Spinal angiolipoma: etiology, imaging findings, classification, treatment, and prognosis. Eur Spine J 2014;23:417-25. [Crossref] [PubMed]
- Carrasco Moro R, Gutiérrez Cierco JA, Martínez San Millán JS, et al. Spinal extradural angiolipomas: 7 new cases and review of the literature. Neurologia 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Onishi FJ, Salem FAS, de Melo Lins DL, et al. Spinal thoracic extradural angiolipoma manifesting as acute onset of paraparesis: Case report and review of literature. Surg Neurol Int 2017;8:150. [Crossref] [PubMed]
- Guzey FK, Bas NS, Ozkan N, et al. Lumbar extradural infiltrating angiolipoma: a case report and review of 17 previously reported cases with infiltrating spinal angiolipomas. Spine J 2007;7:739-44. [Crossref] [PubMed]
- Shweikeh F, Sangtani A, Steinmetz MP, et al. Spinal angiolipomas: A puzzling case and review of a rare entity. J Craniovertebr Junction Spine 2017;8:91-6. [Crossref] [PubMed]
- Wang FF, Wang S, Xue WH, et al. Epidural spinal angiolipoma: a case series. BMC Res Notes 2017;10:128. [Crossref] [PubMed]
- Akyuva Y, Gonultas A, Karaaslan N, et al. Lumbar Spinal Angiolipoma with Expanding Left Neural Foramen Mimicking Lumbar Schwannoma; Case Report and Review of The Literature. Open Neurol J 2017;11:20-6. [Crossref] [PubMed]
- Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer 1974;34:720-7. [Crossref] [PubMed]
- Leu NH, Chen CY, Shy CG, et al. MR imaging of an infiltrating spinal epidural angiolipoma. AJNR Am J Neuroradiol 2003;24:1008-11. [PubMed]
- Tsutsumi S, Nonaka Y, Abe Y, et al. Spinal angiolipoma in a pregnant woman presenting with acute epidural hemorrhage. J Clin Neurosci 2011;18:849-51. [Crossref] [PubMed]
- Kuroda S, Abe H, Akino M, et al. Infiltrating spinal angiolipoma causing myelopathy: case report. Neurosurgery 1990;27:315-8. [Crossref] [PubMed]
- Mascalchi M, Arnetoli G, Dal Pozzo G, et al. Spinal epidural angiolipoma: MR findings. AJNR Am J Neuroradiol 1991;12:744-5. [PubMed]
- Gonzalez-Crussi F, Enneking WF, Arean VM. Infiltrating angiolipoma. J Bone Joint Surg Am 1966;48:1111-24. [Crossref] [PubMed]
- Konya D, Ozgen S, Kurtkaya O, et al. Lumbar spinal angiolipoma: case report and review of the literature. Eur Spine J 2006;15:1025-8. [Crossref] [PubMed]