
View of U.S. spine surgeons regarding cost reduction measures
Introduction
The increasing cost of healthcare in the United States (US), approximately $2.8 trillion or 18% of the GDP, has produced a debate regarding how to curtail spending while still providing high-quality care (1). Because physicians play a critical role in influencing healthcare costs, their views are of particular importance. In 2013, Tilburt et al. reported that US physicians felt responsible to reduce costs and exhibited the most enthusiasm for promoting continuity of care, addressing systemic fraud and abuse, promoting coordinated care of chronic diseases, and limiting corporate influences (2). According to Raphael et al., US anesthesiologists similarly reported responsibility to reduce the costs associated with healthcare (3).
Notably, the rise of healthcare expenditure has been mirrored by the increasing cost of spine surgery. From 1999 to 2008, spine-related expenditures increased by 95% for adults with a primary diagnosis of a spine condition, after adjusting for inflation (4). In 2005, approximately $86 billion was spent in spine-related expenditures (5). Furthermore, because 20% of Americans are expected to be over age 65 by year 2030, the prevalence of degenerative spine conditions is expected to increase (6). Given that reducing costs associated with spine surgery will require surgeon buy-in, it is necessary to study the views of spine surgeons regarding cost reduction measures.
Methods
Instrument development
This cross-sectional study was reviewed and deemed exempt by the Institutional Review Board of the University of California, Irvine. After receiving approval, a multi-disciplinary team developed and revised a modified version of the survey instrument over the course of several months in order to compare the attitudes of North American spine surgeons directly with those of US physicians of various specialties and US anesthesiologists (2,3). An 8-item instrument was created with demographic questions in addition to items related to responsibility, strategy, and roles in cost reduction measures in healthcare (Figure S1). The strengthening the reporting of observational studies in epidemiology (STROBE) statement was used as an aid in the reporting of the results of this study (7).
Survey domains
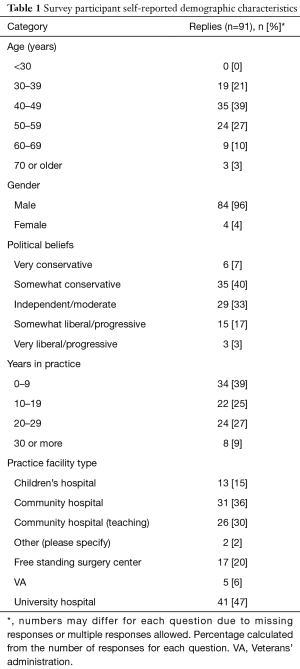
Demographic characteristics
Respondents were asked about age (<30, 30–39, 40–49, 50–59, 60–69, and ≥70), gender, political views, number of years in practice (0–9, 10–19, 20–29, and ≥30), and practice facility. Political beliefs were represented as the following spectrum: very conservative, somewhat conservative, independent/moderate, somewhat liberal/progressive, and very liberal/progressive. Practice facilities included: children’s hospital, community hospital, community hospital (teaching), other, free standing surgery center, veterans’ administration (VA), and university hospital. If “other” was selected, the respondent was asked to specify practice facility.
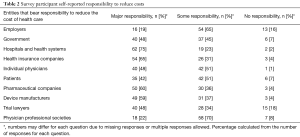
Responsibility to reduce healthcare costs
Participants were asked to indicate the level of responsibility (major responsibility, some responsibility, no responsibility) that the following entities bear to reduce the cost of healthcare: employers, government, hospitals and health systems, health insurance companies, individual physicians, patients, pharmaceutical companies, device manufacturers, trial lawyers, and physician professional societies.
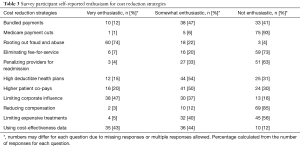
Enthusiasm for cost reduction strategies
Respondents were asked to rate degree of enthusiasm (very enthusiastic, somewhat enthusiastic, not enthusiastic) for the following cost reducing strategies: “bundled” payments, allowing Medicare payment cuts to take effect, rooting out fraud and abuse, eliminating fee-for-service, penalizing providers for readmissions, high deductible health plans, higher patient co-pays, limiting corporate influence, reducing compensation, limiting access to expensive treatments, and using cost-effectiveness data to determine available treatments.
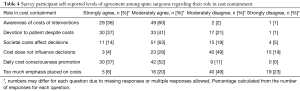
Role in cost containment
Respondents were also asked to indicate degree of agreement (strongly agree, moderately agree, moderately disagree, strongly disagree) regarding the following roles related to cost management: awareness of costs, devotion to patients’ best interests despite costs, cost-influenced decision-making, decision-making based on the costs to the healthcare system, daily cost consciousness promotion, and cost emphasis on tests and procedures.
Data collection
Practicing members of AO Spine North America (AOSNA) were recruited to participate in an anonymous, online survey. Non-practicing members were excluded. A power analysis for a population of 582 individuals with a margin of error of ±0.05 and 95% confidence level indicated that a sample size of 232 would be required. In April 2015, a recruitment email containing a request to complete the 9-item survey, contact information of the research team, and an active hyperlink to the online survey (Qualtrics, Salt Lake City, UT, USA) was disseminated. A second reminder email was sent in May of 2015. Data were collected between April and May 2015.
Data analysis
Demographic data including age, gender, political beliefs, years in practice, and practice facility (Questions 2–6, Figure S1) were described with simple quantification and percentages. The following variables were dichotomized: age (less than 40 years old versus greater than or equal to 40 years), political views (very to somewhat conservative versus moderate to somewhat or very liberal), years in practice (0–9 years versus 10 or more years). Dichotomized variables (age, political views, years in practice, and practice facility) were then incorporated into analyses. Post-hoc scales were developed to describe the level of responsibility of entities to reduce healthcare costs, enthusiasm for cost reduction strategies, and agreement for role in cost reduction (Questions 7–9, Figure S1). For each item, the percentage of responses was calculated from the total number of responses for each answer choice and descriptive statistics were applied to the dataset. In addition, individual items for responsible entities, cost reduction strategies, and role in cost reduction were grouped into related categories:
- Entities with responsibility to reduce the cost of healthcare were grouped into five separate categories: policy makers (government, trial lawyers), healthcare systems (employers, hospitals and health systems, health insurance companies), providers (individual physicians and physician professional societies), patients only, and developers (pharmaceutical companies, device manufacturers);
- Cost reduction strategies were grouped into three separate categories: physician reimbursement (bundled payments, Medicare payment cuts, eliminating fee-for-service, penalizing providers for readmission, reducing physician compensation), patient expenses (high-deductible health plans and higher patient co-pays), and efficiency promotion (rooting out fraud and abuse, limiting corporate influence, limiting expensive treatments, and using cost-effectiveness data);
- Roles in cost reduction were grouped into two separate categories: engagement in cost reduction (awareness of costs of interventions, societal costs affecting decisions, and daily cost consciousness promotion) and avoidance of cost reduction (devotion to patient despite costs, costs do not influence decisions, and too much emphasis placed on costs).
Level of responsibility allocated to various entities was determined by scoring each individual item (0= no responsibility; 1= some responsibility; 2= major responsibility) and calculating a composite score for each of the five categories described above. For enthusiasm for cost reduction strategies, a similar strategy was used by scoring each item (0= not enthusiastic; 1= somewhat enthusiastic; 2= very enthusiastic) and calculating a composite sum for each of the three aforementioned categories. For level of agreement among spine surgeons regarding their role in cost containment, each item was scored (0= strongly disagree, 1= moderately disagree, 2= moderately agree, 3= strongly agree) and a composite score was calculated for each of the two categories created. Multiple linear regression analysis was used to determine the predictive value of demographic variables (age, gender, political views, years in practice, and practice facility) for each related category of entities responsible for cost reduction (n=5), strategies for cost reduction (n=3), and roles in cost reduction (n=2). Analyses were conducted using Microsoft® Excel Version 15.11.2 (Microsoft, Redmond, WA, USA) and IBM® SPSS® Statistics Version 25.0 (SPSS Inc., Chicago, IL, USA).
Results
The recruitment email reached 582 members of AOSNA. A total of 91 members participated (16.0%) with 11 partially-completed responses.
Responses
Demographic characteristics
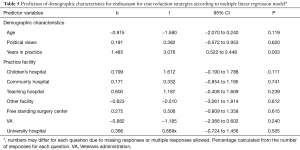
Of all respondents, 0% were less than 30 years old (n=0), 21% were 30–39 years old (n=19), 39% were 40–49 years old (n=35), and 27% were 50–59 years old (n=24). Another 10% were 60–69 years old (n=9) and the remaining 3% were 70 years or older (n=3). Participants were 96% male (n=84) and 4% female (n=4). Nearly half of the respondents were politically conservative with 7% considering themselves very conservative (n=6) and 40% somewhat conservative (n=35). Other respondents were 33% independent or moderate (n=29) and few respondents considered themselves liberal/progressive (n=15, 17%) or very liberal/progressive (n=3, 3%). Also, the majority had been practicing for less than 30 years, with 39% for 0–9 years (n=34), 25% for 10–19 years (n=22), and 27% for 20–29 years (n=24). Only 9% of participants reported more than 30 years in practice (n=8). Demographic data are presented in Table 1.
Full table
Responsibility to reduce healthcare costs
The majority of respondents indicated that hospital and health systems, health insurance companies, pharmaceutical companies, and device manufacturers had major responsibility to reduce the costs associated with healthcare. Most respondents also assigned some degree of responsibility to employers, individual physicians, patients, and physician professional societies. Trial lawyers had the least responsibility to manage the cost of healthcare. Entities allocated responsibility to reduce the costs of healthcare are indicated in Tables 2,3.
Full table
Full table
Enthusiasm for cost reduction strategies
Most participants were very enthusiastic about rooting out fraud and abuse and somewhat enthusiastic about high deductible health plans and higher patient co-pays. There was also more enthusiasm for limiting corporate influences and using cost-effectiveness data to guide implementation of cost reduction measures. However, there was considerably less enthusiasm for bundled payments. Furthermore, the majority of respondents were not enthusiastic about Medicare payment cuts, eliminating fee-for-service models, penalizing for re-admissions, reducing compensation to physicians, and limiting expensive treatments. Enthusiasm for cost reduction strategies is described in Tables 2,3.
Role in cost containment
The majority of respondents moderately agreed that they were aware of the cost of their interventions, influenced by cost awareness in terms of choice of treatment, and responsible to promote cost-conscious decision-making in daily patient care. There was also considerable agreement that respondents should be devoted to a patient’s best interests regardless of the costs. In contrast, participants mostly disagreed with the assertion that they did not consider the costs to the healthcare system when making treatment decisions or that there was too much emphasis placed on the costs of tests and procedures. Levels of agreement in terms of role in cost containment are described in Table 4.
Full table
Demographic predictors of views of spine surgeons
Age, gender, political views, years in practice, and practice facility demographics reported by spine surgeons were not statistically significant predictors for responsibility allocated to policy makers, healthcare systems, providers, patients, or developers to reduce the cost of healthcare according to the multiple linear regression model (P>0.05). By comparison, the model significantly predicted enthusiasm for strategies to reduce healthcare costs that involved reducing physician reimbursement (P=0.049). According to the model, spine surgeons who were in practice for longer were more enthusiastic about implementing strategies to reduce physician reimbursement to reduce to the cost of healthcare (b=1.485, t=3.076, P=0.003).
Based on the multiple linear regression model, demographic variables were not statistically significant predictors of the remaining categories of cost reduction strategies such as increasing patient expenses and efficiency promotion (P>0.05). Finally, none of the demographic variables were significant predictors of surgeons’ agreement regarding their role in cost reduction as indicated by engagement in or avoidance of cost containment (P>0.05) (Table 5).
Full table
Discussion
Due to the large cost associated with spine procedures and the expectation that spine-related conditions are to be more common in an aging population, it is necessary to determine the opinions of spine surgeons regarding reducing the costs associated with healthcare. Surgeons responded that hospitals and health systems, health insurance companies, pharmaceutical firms, and device manufacturers bore major responsibility to reduce the cost of healthcare. Although employers, individual physicians, patients, and physician professional societies were also given some responsibility, trial lawyers were held least responsible. Notably, these views were not significantly influenced by respondent demographics, suggesting the spine surgeons’ held healthcare systems accountable regardless of political attitudes or other personal characteristics.
Spine surgeons were most enthusiastic about rooting out fraud and abuse but also expressed enthusiasm for addressing insurance plans with high deductibles and higher co-pays. However, there was less enthusiasm for bundled payments and the vast majority of spine surgeons were not enthusiastic about Medicare payment cuts, removing fee-for-service, penalizing re-admission, reducing compensation to surgeons, and limiting access to costly treatments. Although spine surgeons attributed responsibility for healthcare costs to several entities, they disagreed with most cost containment strategies proposed in the survey. These findings indicate that spine surgeons prioritize limiting wastefulness in healthcare but do not support measures that reduce reimbursement to individual physicians. Notably, strategies to reduce cost that involved limiting physician reimbursement were met with more enthusiasm by surgeons who had been in practice for longer. This may be in-part because orthopedic surgeons are be concerned with student loan repayment that may have interest rates as high as 6%, resulting in debt greater than $150,000 following post-graduate education and sub-specialty training (8). But, spine surgeons that have completed their training, received much higher salary for several years, and/or repaid debt may therefore be more willing to accept strategies limiting physician reimbursement to reduce the overall costs of healthcare.
Regarding their role in controlling healthcare costs, spine surgeons agreed that they were aware of the costs of interventions, factored these costs into decision-making, and had a responsibility to promote cost-conscious decision-making in their practices. Conflictingly, there was also considerable agreement for devotion to patients’ best interests regardless of the associated cost. These responses indicate that spine surgeons view themselves as advocates for their patients but must reconcile these attitudes with a duty to reduce costs to society and the healthcare system. Not only did surgeons indicate that costs were factored into treatment decisions but adequate emphasis was being placed on the costs of procedures and tests. Furthermore, attitudes regarding roles in cost containment were not affected by political beliefs, years in practice, or other demographic traits.
Spine surgeons’ preferences were compared to those of US physicians of various specialties and US anesthesiologists by examining the findings of Tilburt et al. and Raphael et al., respectively (2,3). The majority of respondents from all 3 studies indicated major responsibility for health insurance companies, hospitals, and healthcare systems alike to regulate healthcare costs (2,3). However, unlike spine surgeons, the majority of US physicians held trial lawyers to be highly responsible (2). Respondents from all three studies expressed similarly little enthusiasm for fixed or “bundled” payments, Medicare payment cuts, and eliminating the fee-for-service model (2,3). The majority of US physicians, including the spine surgeons surveyed in this study, were very enthusiastic about rooting out fraud and abuse (2). One notable difference was that although Tilburt et al. found that American physicians were predominantly very enthusiastic about limiting access to expensive treatments, the majority of spine surgeons that responded to this survey were not enthusiastic about this (2). These differences in enthusiasm for limiting access to expensive treatment may be attributable to medical specialty. While the majority of physicians, including anesthesiologists, are in charge of wide-ranging care to a relatively large number of patients, spine surgeons deliver an expensive but necessary treatment option to a small group of individuals who have failed to respond to conservative treatment. Therefore, although the attitudes of spine surgeons greatly align with those of US anesthesiologists and various US physicians in relation to cost reduction in healthcare, there remain some key differences in terms of which entities bear the responsibility (lawyers) and which strategies should be implemented to limit expenditures (limiting access to expensive treatment options).
Limitations
Although cause-and-effect relationships could not be established due to the cross-sectional study design, significant demographic variations were documented. Also, though the sample was adequate for the statistical tests that were performed, the response rate of 16% was only sufficient for a margin of error of approximately ±0.09. Despite our attempt to increase the number of responses by sending reminder emails, similar response rates for electronic surveys have been commonly documented in the literature (9). Non-response bias could not be compensated for due to lack of population data and social desirability bias may have affected results. Moreover, the views expressed by spine surgeons of one organization may not be representative of all spine surgeons in North America.
Conclusions
In conclusion, spine surgeons allocated major responsibility to healthcare systems to manage the cost of healthcare, supported curbing wasteful spending rather than measures that may reduce compensation to physicians, and agreed to a role in cost control despite also being devoted to the best interests of their patients. Also, spine surgeons who had been in-practice for longer expressed more enthusiasm for reducing compensation to better manage the costs of healthcare. Compared to US physicians of various specialties, spine surgeons placed less responsibility on lawyers to control healthcare costs and did not support limiting expensive treatment options. These findings indicate that spine surgeons share similar values compared to other physicians regarding healthcare cost reduction, but differ with regards to who should be held responsible and what strategies should be employed to control expenditures.
Acknowledgements
We thank Drs. Tuyen Hoang, PhD and Yanjun Chen, MS for their statistical support.
Funding: This work was partially supported by National Institutes of Health grant UL1 TR001414 from the National Center for Advancing Translational Sciences.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board approval (HS#2014-1694) was obtained at the University of California Irvine.
References
- Menger RP, Wolf ME, Kukreja S, et al. Medicare payment data for spine reimbursement; important but flawed data for evaluating utilization of resources. Surg Neurol Int 2015;6:S391-7. [Crossref] [PubMed]
- Tilburt JC, Wynia MK, Sheeler RD, et al. Views of US physicians about controlling health care costs. JAMA 2013;310:380-8. Erratum in: JAMA 2013;310:2102. JAMA 2013;310:857. [Crossref] [PubMed]
- Raphael DR, Cannesson M, Rinehart J, et al. Health Care Costs and the Perioperative Surgical Home: A Survey Study. Anesth Analg 2015;121:1344-9. [Crossref] [PubMed]
- Davis MA, Onega T, Weeks WB, et al. Where the United States spends its spine dollars: expenditures on different ambulatory services for the management of back and neck conditions. Spine (Phila Pa 1976) 2012;37:1693-701. [Crossref] [PubMed]
- Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. Erratum in: JAMA 2008;299:2630. [Crossref] [PubMed]
- O'Lynnger TM, Zuckerman SL, Morone PJ, et al. Trends for Spine Surgery for the Elderly: Implications for Access to Healthcare in North America. Neurosurgery 2015;77 Suppl 4:S136-41. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. [Crossref] [PubMed]
- Johnson JP, Cassidy DB, Tofte JN, et al. Orthopedic Surgery Resident Debt Load and Its Effect on Career Choice. Orthopedics 2016;39:e438-43. [Crossref] [PubMed]
- Braithwaite D, Emery J, De Lusignan S, et al. Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract 2003;20:545-51. [Crossref] [PubMed]



