Microendoscopic discectomy (MED) for lumbar disc herniation: comparison of learning curve of the surgery and outcome with other established case studies
Introduction
The first surgery for lumbar disc herniation was performed by Oppenheim and Kruse [1909]. Mixter and Barr performed laminectomy and removed the disc via the transdural approach. Love introduced the intraluminal-extradural approach for discectomy between 1937 and 1939. Caspar and Yasargil introduced microsurgery for lumbar disc disease in 1977 (1), which was later refined by Williams in 1978. However, the procedure involved separation of paraspinal muscles of the lamina and spinous process, thus resulting in associated post-operative pain and morbidity. Percutaneous lumbar nucleotomy was another minimally invasive procedure for lumbar disc herniation, reported in 1975. Subsequently, percutaneous lumbar disc surgery evolved including percutaneous nucleotomy using automated disc removal devices, spinal endoscopy, and laser. These procedures used posterolateral or para-foraminal approach, and the indications for these procedures have been limited to contained lumbar disc herniation. Furthermore, they have not proven to be as effective as standard open lumbar discectomy, because of longer duration of surgery and some technical problems in addressing all the different aspects of lumbar disc disease.
In 1997, Foley and Smith introduced endoscopic discectomy, a technique that involved use of an operative endoscope with a tubular system. With time, the tubular retractors were modified to include a microscope instead of an endoscope. This alternative approach was introduced by Foley et al. in 2003, and termed as microendoscopic discectomy (MED). Currently the term has been used interchangeably for discectomy procedure utilizing tubular retractors, either with an endoscope or microscope. The muscle retracting posterior approach in MED reduces the approach site comorbidity and the endoscope yields visualization beyond the confines of the tubular retractor. Hence, advantageous over the previously developed minimally invasive procedures for discectomy.
Further, there are two major techniques for MED, the METRx-MD system (Medtronic Sofamor Danek, Memphis, TN, USA) and the Destandau’s procedure using Storz endoscopic microdiscectomy system. Many surgeons prefer the METRx-MD system, which allows the surgeons to operate under direct vision through the microscope. This method was first used in 2003, by the company Medtronic and later perfected by Ryang et al. in 2007.
Many surgeons prefer the METRx-MD system (Medtronic Sofamor Danek), which allows the surgeons to operate under direct vision through the microscope. In India, the Destandau’s technique has been widely accepted. It was developed by Destandau in early 1990s. This technique ensures minimal iatrogenic trauma and extreme efficiency. The size of the incision is small such that the scar does not exceed 3 cm. So, the procedure is less traumatic and more cosmetic. Moreover, this endoscopic approach to lumbar disc herniation gives maximum exposure to disc space with the goal of minimizing cutaneous incision. However, there is a steep learning curve associated with using the endoscopic operating system efficiently and safely. But once the technique is mastered, the modularity of the MED system allows for the development of expanded applications beyond lumbar nerve root decompression.
We have been doing regular laminectomy and discectomy for all kinds of lumbar disc prolapse, subsequently when the disc prolapse was on one side with the symptoms and signs presenting towards the same side our surgery was refined to one side muscle dissection and followed by hemi laminectomy and discectomy. Subsequent development in micro neurosurgery made our incision smaller in size followed by fenestration/microdiscectomy using microscope.
The aim of our study was to compare the results of a series of microendoscopic discectomies done at a government medical college in South India, with other published series. We have done 40 cases of microendoscopic discectomy, using the Destandau’s procedure using Storz endoscopic microdiscectomy system. The learning curve for the procedure was also analyzed. For this, certain main parameters such as number of days spent in hospital mean duration of surgery and mean blood loss were compared between the first 20 cases and the last 20 cases.
Methods
This was a prospective study conducted in the department of neurosurgery, Stanley Medical College between 2003–2007. The patients who had acute onset of symptoms of unilateral low back pain with sciatica and whose clinical examination showed signs of definitive radiculopathy and MRI showing sequestered disc prolapse at that corresponding level were included in to study protocol. Subsequently we have included two level discs in our study. We have excluded the patients with lumbar canal stenosis with disc prolapse, spondylolysis with listhesis with disc prolapse, old age with severe signs of degeneration (bone, disc, ligamentum flavum). We have also excluded patients with bilateral symptoms and signs and MRI showing bilateral root compression. Hence our selection for endoscopic discectomy was unilateral single or two level sequestrated and large contained discs.
Of the 40 cases operated, 39 were single level discs and 1 was a double level disc. In a span of 3 years from 2004 to 2007 we have done 40 cases of disc removal using endoscope. Among the cases that had met the criteria for using the endoscope, 31 were males, 9 were females. All the cases were in the age group between 20–50 years.
Clinically patients were examined to confirm the radicular involvement. We have ruled out the signs of Lumbar canal stenosis in the form of claudication and also ruled out lysis or listhesis clinically by absent low back pain in flexion, extension and step sign.
Ethics committee of the institution approval was obtained prior to the commencement of the study.
The investigative procedures for all the patients included, X-ray lumbosacral spine AP, lateral, CT scan lumbosacral spine and MRI Lumbosacral spine.
X-ray lumbosacral spine had been useful to find out transitional vertebrae so as to help us to localize exactly during surgery. It had also been helpful to identify lysis, listhesis, or any other bony involvement.
CT scan had been useful to rule out lumbar canal stenosis and MRI lumbosacral spine to identify the sequestrated disc and root compression. After obtaining anesthetic fitness, surgery was done under General anesthesia. Although the METRx-MD system (Medtronic Sofamor Danek) is being used worldwide, we have followed Destandau’s procedure using Storz endoscopic micro discectomy system. This technique was the first to be introduced in India, and thereafter accepted by surgeons all over India. Contrary to other minimally invasive approaches, the visual field in discectomy by Destandau technique is broad and depending on the workability of the Endospine, an adequate access, even to two lumbar levels is possible and since the endoscope has four working portals, each of the portal will not interfere with the other. This is an added advantage. In addition to this, irrespective of the location of hernia, the procedure can be used for median, herniated, foraminal, extraforaminal and even recurrent types of hernia.
Discectomy by Destandau technique makes use of the following:
- 4 mm 0 deg telescope;
- Endospine operating tube with obturator;
- Endospine working sheath which has four portals
- For endoscope;
- For nerve retractor;
- For working channel for using instruments;
- For suction.
- 2 mm Kerrison Rongeur;
- 2 mm disc punch;
- Take apart bipolar forceps;
- Camera with light source and fibro optic cable;
- Monitor.
Procedure
Patient is at first positioned appropriately. Once patient is positioned, the affected disc is localized. After localization of the disc, determination of the point of incision and direction of approach to the disc, a skin incision between 10 to 15 mm is made, depending on the patient’s corpulence. Transection of the aponeurosis using scissors and dissection of the paravertebral muscles adjoining the hernia is done. Insertion of the Endospine operating tube, retracting the obturator, cleaning the window using disc forceps, positioning of the working insert with introduced telescope and continuation of the intervention under video endoscopic control is followed. Resection of a part of superior lamina so as to draw back the superior part of the yellow ligament, and resection of the latter as well as part of the articular process so as to expose the outer margin of the dural sac and proximal end of the nerve root concerned is done. Dissection of the nerve root allows access to the prolapse. The presence of several channels facilitates handling the anatomical structures within the vertebral canal. The use of nerve root retractor allows for fully exposing the disc prolapse and facilitates the surgical procedures by considerably reducing the risk of damaging nerve structures. The positioning of the endoscope close to the vertebral canal allows a panoramic view and the localization of the migrated fragments. Depending on the case, microdiscectomy is carried out once the hernia is removed. The cavity is then irrigated, and hemostasis generally achieved simply by packing or by bipolar coagulation. After removal of the endoscopic instruments, careful hemostasis of the muscle masses can be carried out. Intracutaneous sutures are applied followed by water impermeable dressing allowing showering and immediate rehabilitation. Suture removal is then done on the 10th postoperative day.
Results
In our series, number of patients who had undergone microendoscopic discectomy was 40. Among them 31 patients were male and 9 patients were females. All patients were between 20–50 years of age and the mean was 32.3. The most common level operated was L5–S1 [27] followed by L4–L5 [12]. We have operated double level in 1 patient at L4–L5 and L5–S1.
All patients were followed up regularly on 10th postoperative day, 1 month, 3 months and one year. Mean follow up of all patients were 14.1 months and the longest follow up was done at 38 months.
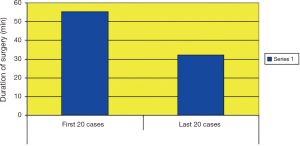
Since the procedure is technically demanding, it took initial 20 cases to complete our learning curve and in the next 20 cases we improved our technique, operating time, blood loss, and outcome. So, we have compared our results in the first 20 cases and last 20 cases.
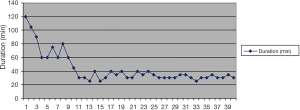
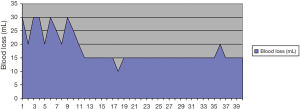
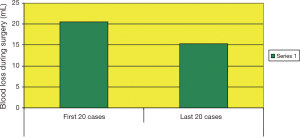
Mean hospital stay in our first 20 cases was 2.75 days and in our last 20 cases was 2.98 days. Mean hospital stay increased in our last 20 cases because of one patient who had wound infection had to stay in the hospital for 2 weeks (Figure 1). If we exclude the patient who had infection our mean hospital stay drops to 2.4 days as compared to the stay of initial 20 cases. Mean duration of surgery in the first 20 cases was 55.26 minutes and in our last 20 cases was 32.14 minutes and mean blood loss during the first 20 cases was 20.5 mL and in our last 20 cases was 15.25 mL.

In our series we also assessed the outcome based upon modified Macnab criteria.
Modified Macnab criteria
- Excellent: free of pain; no restriction of mobility & return to normal work;
- Good: occasional non-radicular pain; relief of presenting symptom; return to modified work;
- Fair: some improved functional capacity; still unemployed and or handicapped;
- Poor: continued objective symptoms of root involvement; additional operative intervention needed at index level irrespective of operative time or length of post op stay.
In our series according to modified Macnab criteria, 28 patients had excellent outcome, 5 patients had good outcome, 4 patients had fair outcome and 3 patient had poor outcome.
Discussion
Microendoscopic discectomy is one of the treatment modality for lumbar disc disease and it is an alternate for traditional microscopic lumbar discectomy. We have compared the following results with other published series: (I) mean operative duration; (II) blood loss during surgery; (III) mean hospital stay; (IV) time taken to return to work; (V) learning curve; (VI) complications; (VII) revision surgery; (VIII) reoccurrence.
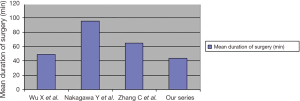
The mean operative duration in Wu et al. (2) series was 75±26 minutes in their early 220 patients and it was significantly reduced to 49±21 minutes in their last 653 patients. In Nakagawa et al. (3) series the mean duration for MED was 95.3 minutes. Zhang et al. (4) reported 64.77±17.83 as mean duration (Figure 2). In our series in the initial 20 cases the mean duration was 55.26 minutes and it was significantly reduced to 32.14 minutes in our last 20 cases. The mean duration for all 40 cases in our series was 43 minutes (Figures 3,4).
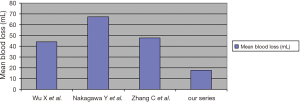
The mean blood loss in Wu et al. (2) series was 44 mL and in Nakagawa et al. (3) was 67.5 mL. In Zhang et al. (4) series it was 47.5±11.62 mL. In our series the mean blood loss in the initial 20 cases was 20.5 mL and it was significantly reduced to 15.25 mL in our last 20 cases (Figure 5). We have used adrenaline-soaked gauzes during paraspinal muscle separation and we kept adrenaline-soaked gauzes for few minutes before placing the Endoscopic microdiscectomy system. The mean blood loss taking in to account of all 40 patients in our series was 17.8 mL (Figures 6,7).
The mean hospital stay in Wu et al. (2) series was 4.8 days and in Perez-Cruet et al. (5) series it was 7.7 hours. In our series the mean hospital stay in our first 20 cases was 2.75 days and in our last 20 cases it was 2.98 days. The mean hospital stay in our last 20 cases increased than our first 20 cases because in our last 20 patients one patient had wound infection and stayed 14 days in the hospital. The mean hospital stay taking in to account of all 40 cases in our series was 2.8 days or 67.2 hours.
The average days taken to return to work in Wu et al. (2) series was 15 days and in Perez-Cruet et al. (5) series it was 17 days. Destandau et al. (6), who has reported the largest MED series in the world, reported 4 weeks as the average duration taken to return to work. In our series the mean duration to return to work was 4.05 weeks.
With regards to the post-operative complications in patients, Wu et al. (2) series 5.3% of the patients had significant medical complications and 20 patients underwent redo surgery. Perez-Cruet et al. (5) reported 5% of the patients in his early cases had significant medical complications. In Nakagawa et al. (3) series 4% of the patients had complications and 12 patients underwent redo surgery. Destandau et al. (6) reported 10.6% of his patients had significant medical complications and 44 patients underwent redo surgery. In our series 10% of cases had complications, among them 1 patient had wound infection, 1 patient had dural tear, and in 2 patients pain didn’t subside and they underwent redo open laminectomy. The complication rate of 10% was due to the initial learning curve. Dural tear and redo open laminectomy for persistent pain was seen in the first 20 cases. With practice, surgeons were able to overcome this, thereby leading to a decrease in complication rate.
Lastly, in the outcome assessment, according to modified Macnab criteria, Wu et al. (2) series 74% patients had excellent outcome, 19% patients had good outcome, 3% had fair outcome, and 4%patients had poor outcome. In Perez-Cruet et al. (5) series 77% patients had excellent outcome, 17% patients had good outcome, 3% patients had fair outcome, and 3% patients had poor outcome. Ranjan et al. (7), reported in their series as 76 patients had excellent outcome, 22 patients had good outcome, 5 patients had fair outcome and 3 patients had poor outcome. In Destandau et al. (6) series out of 1,027 patients, 980 patients had excellent outcome, 6 patients had good outcome, 1 patient had fair outcome and 40 patients had poor outcome.
In our series out of 40 patients, 28 patients had excellent outcome, 5 patients had good outcome, 4 patients had fair outcome and 3 patients had poor outcome. Moreover, excellent to good outcome was observed in the last 20 cases, after the initial learning curve was complete, as compared to poor to fair outcome in the first 20 patients. Hence, it was observed in the study that the MED procedure requires a steep learning curve and it required 20 cases for us to complete it. Nakagawa et al. (3) reported in their series as it required 30 cases for them to complete the learning curve.
Conclusions
Endoscopic discectomy is a minimally invasive procedure with less tissue disruption to achieve the results of the traditional surgery. The major advantages of microscopic endoscopic discectomy are as follows:
- Early mobilization of the patient on the same day;
- Negligible intra operative blood loss;
- Lesser postoperative pain;
- Lesser days in hospital. Procedure can be done as day care surgery;
- Early return to work;
- Minimized hospital expenditure.
Based upon Sasaoka et al. (8), Chao et al. (9), Zhang et al. (4), Huang et al. (10), and Schick et al. (11) series, the magnitude of tissue damage and surgical trauma response in MED are significantly lower than traditional lumbar disc surgeries.
Sasani et al. (12), reported that the MED procedure can be considered as a safe alternative for extraforaminal disc migrations. Le et al. (13), and Isaacs et al. (14) reported as it is also a treatment modality for recurrent lumbar disc herniation.
Thus, microendoscopic discectomy in properly trained hands is an additional efficient armamentarium in the management of lumbar disc disease. However, there is a learning curve, which could range from 20–30 cases. It is an excellent technique that could replace the conventional open surgery, if the learning curve could be overcome.
Acknowledgements
The authors thank Prof. K Deiveegan, MS, MCh (Neuro) and Prof. S Eswaramurthy, MS, MCh (Neuro), Professor and Head, Department of Neurosurgery.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics committee of the institution approval was obtained prior to the commencement of the study (SMC-NSEC No. 01-JUL2003). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Chedid KJ, Chedid MK. The "tract" of history in the treatment of lumbar degenerative disc disease. Neurosurg Focus 2004;16. [Crossref] [PubMed]
- Wu X, Zhuang S, Mao Z, et al. Microendoscopic discectomy for lumbar disc herniation: surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976) 2006;31:2689-94. [Crossref] [PubMed]
- Nakagawa Y, Yoshida M, Maia K. Microendoscopic Discectomy (MED) For Surgical Management Of Lumbar Disc Disease: Technical Note. The Internet Journal of Spine Surgery 2005;2:1-7.
- Zhang C, Zhou Y, Chu TW, et al. Traumatic responses following microendoscopic discectomy: clinical analysis of 44 patients. Zhonghua Yi Xue Za Zhi 2006;86:3039-42. [PubMed]
- Perez-Cruet MJ, Foley KT, Isaacs RE, et al. Microendoscopic lumbar discectomy: technical note. Neurosurgery 2002;51:S129-36. [Crossref] [PubMed]
- Destandau J. Endoscopic Lumbar Disc Surgery: A Study of 1562 cases. Internet Journal of Minimally Invasive Surgical Technology 2008;2:16.
- Ranjan A, Lath R. Microendoscopic discectomy for prolapsed lumbar intervertebral disc. Neurol India 2006;54:190-4. [PubMed]
- Sasaoka R, Nakamura H, Konishi S, et al. Objective assessment of reduced invasiveness in MED. Compared with conventional one-level laminotomy. Eur Spine J 2006;15:577-82. [Crossref] [PubMed]
- Chao Z, Yue Z, Tong-wei C, et al. Microendoscopic discectomy, a less traumatic procedure for lumbar disk herniation. Chin J Traumatol 2007;10:311-4. [PubMed]
- Huang TJ, Hsu RW, Li YY, et al. Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res 2005;23:406-11. [Crossref] [PubMed]
- Schick U, Döhnert J, Richter A, et al. Microendoscopic lumbar discectomy versus open surgery: an intraoperative EMG study. Eur Spine J 2002;11:20-6. [Crossref] [PubMed]
- Sasani M, Ozer AF, Oktenoglu T, et al. Percutaneous endoscopic discectomy for far lateral lumbar disc herniations: prospective study and outcome of 66 patients. Minim Invasive Neurosurg 2007;50:91-7. [Crossref] [PubMed]
- Le H, Sandhu FA, Fessler RG. Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Neurosurg Focus 2003;15. [Crossref] [PubMed]
- Isaacs RE, Podichetty V, Fessler RG. Microendoscopic discectomy for recurrent disc herniations. Neurosurg Focus 2003;15. [Crossref] [PubMed]