
Comparison of implant survivability in primary 1- to 2-level lumbar fusion amongst opioid abusers and non-opioid abusers
Introduction
Lumbar fusion (LF) is a treatment option for degenerative disc disease (DDD) in those with signs of instability having failed conservative treatment options (1-3). Minimizing postoperative complications and attaining excellent patient-reported outcome measurements (PROMs) is the ultimate goal for any surgeon (4). Identification of preoperative comorbidities and rectifying modifiable risk factors have been shown to directly improve outcomes (5-8). Unfortunately, there is a high correlation of patients with DDD that rely on opioids for temporary relief (9). In addition to its analgesic effect, opioids have been shown to negatively impact endocrine, immune, gastrointestinal and musculoskeletal systems (10). Opioids are also associated with impairing bone density by hindering the synthesis of androgens as well as the maturation of osteoblastic precursor cells—both of which are vital for bone mineralization (11,12). Furthermore, animal studies have shown that opioids delay healing following spinal fusion (13).
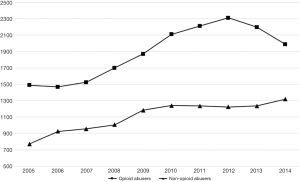
Orthopaedic surgeons are the third highest prescribers of opioids following internists and dentists (14,15). Results from the 2015 National Survey on Drugs and Health, an estimated 12.5 million people were found to be non-prescription opioid users, and an estimated 0.8 million were heroin users (16). Findings from the Medicare population show an increasing trend in the number of patients being diagnosed with opioid abuse or dependency from 2005–2014 (Figure 1). The literature is limited with respect to evaluating the influence of opioid abuse and dependency on orthopaedic implant survivability, infection rates, readmission rates, and its associated costs following primary LF.
The purpose of this study was to analyze and compare: (I) 2-year short term implant related complications; (II) 30-day infection and wound complication rates; (III) 90-day readmission rates; (IV) in-hospital length of stay (LOS); and (V) day of surgery and total global 90-day episode of care cost amongst opioid abusers (OAS) and non-opioid abusers (NAS) undergoing primary 1- to 2-level primary lumbar fusion. We hypothesize that following primary 1-2LF OAS will have greater odds and incidence of short term implant related complications, infection and wound complications, greater in-hospital LOS and greater care of cost compared to NAS.
Methods
A retrospective review from 2005–2014 using the Medicare Standard Analytical Files of the PearlDiver supercomputer (PearlDiver Technologies, Fort Wayne, IN, USA) was performed. PearlDiver is compliant with the Health Information Portability and Affordability Act (HIPAA) and contains the records of over 100 million patients. The database contains information such as diagnosis, procedures, complications, discharge disposition, in-hospital length of stay, cost, reimbursement in addition to other information. The study was exempt from the International Review Board (IRB) review as PearlDiver does not provide identifiable information regarding the patients in the database.
Patients who underwent primary lumbar fusion were identified using the International Classification of Disease, ninth revision (ICD-9) procedural codes 81.04–81.08. Patients undergoing primary 1- to 2-level lumbar fusion were filtered using ICD-9 procedural code 81.62. The inclusion criteria for the study group consisted of all patients with a history of opioid abuse or dependency within 90 days prior to 1-2LF. Patients with a BMI <20 kg/m2, chronic liver disease, diabetes mellitus, hyperthyroidism, tobacco users, alcohol users, osteoporosis, osteopenia, or those who use certain medications that have been known to interfere with bone mineralization were excluded from our study (17). The control group consisted of all patients who underwent 1-2LF with no history of opioid abuse or dependency. Patients in the study group were matched to patients in the control group with respect to age, gender, and Charlson-Comorbidity Index (CCI) to allow for accurate comparison between the two groups.
Two mutually exclusive cohorts were formed and were followed for two years following their index procedure. In-hospital length of stay, 2-year short term implant related complications, 90-day readmission rates, 30-day infection and wound complications, and day of surgery and total global 90-day episode of care costs were compared amongst OAS and NAS (online: http://jss.amegroups.com/public/system/jss/supp-jss.2018.07.07.pdf).
Descriptive and statistical analysis was performed with the programming language R (University of Auckland, New Zealand) with univariate analysis calculating odds-ratios (OR) with their respective 95% confidence interval (95% CI), and P. The threshold for statistical significance was set at P<0.05.
Results
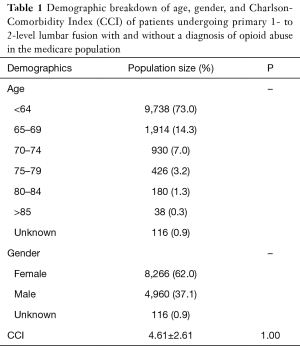
After the matching process, 13,342 (female =8,266, male =4,960, unknown =116) patients who underwent primary 1-2LF were identified, with equal distribution in the study (n=6,671) and control (n=6,671) groups. Both cohorts had an average CCI of 4.61±2.61 with a P of 1.00, indicating the two groups were statistically identical, and were matched appropriately (Table 1). The incidence of OAS undergoing primary 1-2LF increased across the study period (R2=0.78; P<0.001) with a calculated annual growth rate of 3.21% (Figure 1).
Full table
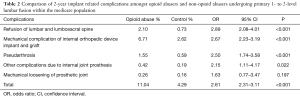
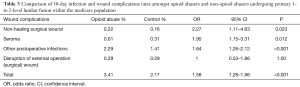
OAS undergoing primary 1-2LF fusion had a greater incidence and odds of short term implant related complications (11.04% vs. 4.29%; OR: 2.61, 95% CI: 2.31–3.11, P<0.001). Specifically, mechanical complications of the internal orthopedic device (6.71% vs. 2.62%; OR: 2.67, 95% CI: 2.23–3.19, P<0.001), and pseudarthrosis (1.55% vs. 0.59%; OR: 2.50, 95% CI: 1.74–3.58, P<0.001). Due to these complications, OAS abusers were at greater odds of requiring a refusion procedure (2.10% vs. 0.73%; OR: 2.89, 95% CI: 2.08–4.01, P<0.001) within 2-year following the index procedure (Table 2). Furthermore, OAS undergoing primary 1-2LF had greater incidence and odds of developing short-term infection and wound related complications (3.41% vs. 2.17%; OR: 1.58, 95% CI: 1.28–1.96, P<0.001) compared to NAS. Opioid abusers were more susceptible to developing a non-healing surgical wound (0.22% vs. 0.16%; OR: 2.27, 95% CI: 1.11–4.63, P=0.023), seroma (0.61% vs. 0.31%; OR: 1.95, 95% CI: 1.15–3.31, P=0.012), and other postoperative infections (2.29% vs. 1.41%; OR: 1.64, 95% CI: 1.26–2.12, P<0.001) (Table 3). OAS were also found to have greater in-hospital LOS compared to NAS (5.11±7.81 vs. 4.57±5.53; P<0.001) as well as greater odds of 90-day readmission rates (OR: 1.29, 95% CI: 1.18–1.40, P<0.001) (Tables 4,5). Day of surgery costs were higher in OAS ($143,057.38±$128,353.26 vs. $121,450.45±$108.249.77; P<0.001) compared to NAS. Similarly, 90-day total costs of care were higher in the opioid abuser group in comparison to non-opioid abuser group ($165,306.00±$158,542.62 vs. $135,867.60±$130,306.90, respectively) (P=0.788), but no statistical significance was found (Table 5).
Full table
Full table

Full table

Full table
Discussion
Opioid abuse and dependence are a nationwide concern, and addiction and abuse potential of these medications is greater than other medications (18-21). Currently, there is limited literature on the effects opioids have on implant survivability along with infection and wound complications following primary 1- to 2-level lumbar fusion. The study demonstrated that opioid abuse and dependency to be a potentially modifiable risk factor associated with suboptimal postoperative outcomes in patients undergoing primary 1- to 2-level lumbar fusion. The cohort of opioid abusers had higher odds and incidences of implant related complications, infections and wounds, in-hospital length of stay, 90-day readmission rates, total cost of care the day of surgery.
Sing et al. presented similar findings, where 6.89% of their patients consuming either short-acting or long-acting opioids prior to orthopaedic surgery subsequently went onto developing superficial infections in addition to other wound infections; whereas patients in the control group had no wound- or infection-related complications (22). 3.44% of the patients consuming opioids developed complications related to wound and infections and subsequently required a revision procedure (22). Recent studies have shown that opioids induce an immunosuppressive state by negatively affecting macrophage and T-cell function by decreasing the maturation of macrophage progenitor cells, which serve as the first line of defense against foreign pathogens. Another study implicated that morphine acts on the Fcy receptors on macrophages affecting the migration and phagocytic capabilities (23-26). The increase in wound complications seen in this cohort could explain the need for revision surgery in opioid abusers following primary 1-2LF.
Furthermore, opioids have an antagonistic effect on bone density via two methods. Opioids act on the hypothalamic-pituitary axis and decrease synthesis of androgen hormones which are vital for proper bone mineralization (12,27-29). Secondly, opioids indirectly impair the maturation of osteoblastic cells, which are vital for bone formation (11,12). Furthermore, long-term use of opioids for the treatment of pain has shown to impair normal cognition and motor function. In a study by Kerr et al. it was found infusion of morphine to normal plasma concentrations led to significant impairments. Their study found processing time of verbal commands increased and being able to maintain low consistent levels of force also decreased. Additionally, long-term opioid use has been shown to lead to development of dizziness and sedation that can lead to consequences such as falls and fractures (10). The compounding insult of decreased bone mineralization and increased susceptibility to falls may explain the dislocation of prosthetic joints, mechanical complications, and mechanical loosening in opioid abusers undergoing primary 1-2LF.
Due to these adverse events it can be conjectured that those with opioid dependence undergoing spine surgery would have higher total cost of care compared to those without this diagnosis. Waljee et al. found that opioid abusers undergoing abdominal surgery incurred greater costs of care due to having longer hospital stays (2.9 vs. 2.5 d, P<0.001) and increased likelihood of being discharged to a rehabilitation facility (3.5% vs. 2.5%, P<0.001) Additionally, 30-day readmission rates were greater in opioid abusers (4.5% vs. 3.6%, P<0.001) compared to non-abusers. 90-day cost of care was also found to be higher in opioid abusers ($12,036.60 vs. $3,863.40, P<0.001), which was consistent with our findings (29).
Opioid-related adverse events such as constipation, emesis, and confusion can result in an increased length of stay (LOS) for all patients. Cozowicz et al. found patients a direct correlation of cost of care with opioid prescription dosage. Patients in the high-consuming group of ≥370 mg/day had an average cost of $21,734 compared to patients in the low-consuming group, >0–130 mg/day who had an average cost of $15,091 (P<0.001) (30).
Despite the many strengths from a large national database, there are limitations inherent to these administrative data systems. The current study was constructed by utilizing ICD-9 codes, which were not developed for the use of research purposes and are subject to human error (31). ICD-9 coding is also prone to significant inaccuracies that can diminish the research-quality data. While the use of large databases are prone to selection bias, utilizing the random matching process of populations would help to rectify any potential bias in this study’s methodology (32). The strength of this study was controlling for covariates which may have potentially been present in the study group and control group. Excluding these covariates and matching both groups randomly increased the validity of this study and reduced potential bias.
Conclusions
This study illustrated opioid abusers having increased complication rates related to postoperative implant failures, infection and wound complications, 90-day readmission rates, and cost of care following primary 1-2LF. The results should motivate surgeons to optimize their patients prior to undergoing spine surgery as opioid use is a modifiable comorbidity. Proper counseling and educating patients of potential risk factors following surgery may help in reducing the number of opioids consumed by patients. Future prospective studies should evaluate the surgical outcomes of those with preoperative opioid dependence who have been weaned from opioid use compared to those who were not able to cease opioid usage prior to lumbar surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was exempt from the International Review Board (IRB) review as PearlDiver does not provide identifiable information regarding the patients in the database.
References
- Wang JC, Dailey AT, Mummaneni PV, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine 2014;21:48-53. [Crossref] [PubMed]
- Drazin D, Ugiliweneza B, Al-Khouja L, et al. Treatment of Recurrent Disc Herniation: A Systematic Review. Cureus 2016;8. [PubMed]
- Chen Z, Zhao J, Liu A, et al. Surgical treatment of recurrent lumbar disc herniation by transforaminal lumbar interbody fusion. Int Orthop 2009;33:197-201. [Crossref] [PubMed]
- Bourne RB, Chesworth B, Davis A, et al. Comparing Patient Outcomes After THA and TKA: Is There a Difference? Clin Orthop Relat Res 2010;468:542-6. [Crossref] [PubMed]
- Duchman KR, Gao Y, Pugely AJ, et al. The Effect of Smoking on Short-Term Complications Following Total Hip and Knee Arthroplasty. J Bone Joint Surg Am 2015;97:1049-58. [Crossref] [PubMed]
- Werner BC, Kurkis GM, Gwathmey FW, et al. Bariatric Surgery Prior to Total Knee Arthroplasty is Associated With Fewer Postoperative Complications. J Arthroplasty 2015;30:81-5. [Crossref] [PubMed]
- Buller LT, Best MJ, Klika AK, et al. The influence of psychiatric comorbidity on perioperative outcomes following primary total hip and knee arthroplasty; a 17-year analysis of the National Hospital Discharge Survey database. J Arthroplasty 2015;30:165-70. [Crossref] [PubMed]
- Lim JBT, Bin Abd Razak HR, Zainul-Abidin S, et al. What Are the Preoperative Outcome Measures That Predispose to Periprosthetic Fractures After Primary Total Knee Arthroplasty? J Arthroplasty 2017;32:2531-4. [Crossref] [PubMed]
- Schoenfeld AJ, Nwosu K, Jiang W, et al. Risk Factors for Prolonged Opioid Use Following Spine Surgery, and the Association with Surgical Intensity, Among Opioid-Naive Patients. J Bone Joint Surg Am 2017;99:1247-52. [Crossref] [PubMed]
- Kerr, B, Hill, H, Coda B, et al. Concentration-related effects of morphine on cognition and motor control in human subjects. Neuropsychopharmacology 1991;5:157-66.
- Chrastil J, Sampson C, Jones KB, et al. Evaluating the Affect and Reversibility of Opioid-induced Androgen Deficiency in an Orthopaedic Animal Fracture Model. Clin Orthop Relat Res 2014;472:1964-71. [Crossref] [PubMed]
- Thakur NA, DeBoyace SD, Margulies BS. Antagonism of the Met5-enkephalin-opioid growth factor receptor-signaling axis promotes MSC to differentiate into osteoblasts. J Orthop Res 2016;34:1195-205. [Crossref] [PubMed]
- Jain N, Himed K, Toth JM, et al. Opioids Delay Healing of Spinal Fusion: a Rabbit Posterolateral Lumbar Fusion Model. Spine J 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Bedard NA, Pugely AJ, Westermann RW, et al. Opioid Use After Total Knee Arthroplasty: Trends and Risk Factors for Prolonged Use. J Arthroplasty 2017;32:2390-4. [Crossref] [PubMed]
- Morris BJ, Mir HR. The opioid epidemic: impact on orthopaedic surgery. J Am Acad Orthop Surg 2015;23:267-71. [Crossref] [PubMed]
- “RESULTS FROM THE 2015 NATIONAL SURVEY ON DRUG USE AND HEALTH: DETAILED TABLES PREVALENCE ESTIMATES, STANDARD ERRORS, P VALUES, AND SAMPLE SIZES.” Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 8 Sept. 2016, Available online: www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf.
- Schürer C, Wallaschofski H, Nauck M, et al. Fracture Risk and Risk Factors for Osteoporosis. Dtsch Arztebl Int 2015;112:365-71. [PubMed]
- Kolcun JPG, Madhavan K, Wang MY. Citizens Urge U.S. Food and Drug Administration to Restrict High-Potency Opioids. World Neurosurg 2017;108:959-60. [Crossref] [PubMed]
- Volkow ND, Frieden TR, Hyde PS, et al. Medication-assisted therapies--tackling the opioid-overdose epidemic. N Engl J Med 2014;370:2063-6. [Crossref] [PubMed]
- Ling W, Mooney L, Hillhouse M. Prescription opioid abuse, pain and addiction: Clinical issues and implications. Drug Alcohol Rev 2011;30:300-5. [Crossref] [PubMed]
- Morgan MM, Christie MJ. Analysis of opioid efficacy, tolerance, addiction and dependence from cell culture to human. Br J Pharmacol 2011;164:1322-34. [Crossref] [PubMed]
- Sing DC, Barry JJ, Cheah JW, et al. Long-Acting Opioid Use Independently Predicts Perioperative Complication in Total Joint Arthroplasty. J Arthroplasty 2016;31:170-4.e1. [Crossref] [PubMed]
- Ninković J, Roy S. Morphine Decreases Bacterial Phagocytosis by Inhibiting Actin Polymerization through cAMP-, Rac-1-, and p38 MAPK-Dependent Mechanisms. Am J Pathol 2012;180:1068-79. [Crossref] [PubMed]
- Breslow JM, Feng P, Meissler JJ, et al. Potentiating Effect of Morphine on Oral Salmonella enterica serovar Typhimurium Infection is µ-Opioid Receptor Dependent. Microb Pathog 2010;49:330-5. [Crossref] [PubMed]
- Banerjee A, Strazza M, Wigdahl B, et al. Role of mu-opioids as cofactors in human immunodeficiency virus type 1 disease progression and neuropathogenesis. J Neurovirol 2011;17:291-302. [Crossref] [PubMed]
- Seyfried O, Hester J. Opioids and endocrine dysfunction. Br J Pain 2012;6:17-24. [Crossref] [PubMed]
- Vuong C, Van Uum SHM, O'Dell LE, et al. The Effects of Opioids and Opioid Analogs on Animal and Human Endocrine Systems. Endocr Rev 2010;31:98-132. [Crossref] [PubMed]
- Demarest SP, Gill RS, Adler RA. Opioid endocrinopathy. Endocr Pract 2015;21:190-8. [Crossref] [PubMed]
- Waljee JF, Cron DC, Steiger RM, et al. Effect of Preoperative Opioid Exposure on Healthcare Utilization and Expenditures Following Elective Abdominal Surgery. Ann Surg 2017;265:715-21. [Crossref] [PubMed]
- Cozowicz C, Olson A, Poeran J, et al. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain 2017;158:2422-30. [Crossref] [PubMed]
- Hashimoto RE, Brodt ED, Skelly AC, et al. Administrative Database Studies: Goldmine or Goose Chase? Evid Based Spine Care J 2014;5:74-6. [Crossref] [PubMed]
- Maltenfort MG. Understanding Large Database Studies. J Spinal Disord Tech 2015;28:221. [Crossref] [PubMed]


