A comparison of narcotic usage and length of post-operative hospital stay in open versus minimally invasive lumbar interbody fusion with percutaneous pedicle screws
Introduction
Instrumented lumbar fusion is a widely accepted surgical treatment for symptomatic degenerative spine disease (1). With an aging population, this procedure remains in high demand (2). Lumbar fusion can be accomplished through open or minimally invasive techniques. The open interbody fusions require more extensive tissue take down, while minimally invasive spinal surgery (MISS) utilizes multiple small incisions and minimizes muscle dissection (3). Multiple studies have reported detrimental effects of extensive muscle dissection and retraction often employed in open transforaminal lumbar interbody fusion (TLIF) procedures (4,5).
Despite these disadvantages, open instrumented spinal fusions reliably result in high fusion rates, increased foraminal height, and improved post-operative patient satisfaction (6,7). The goal of MISS is to minimize soft tissue trauma, thereby decreasing pain levels and improving post-operative rehabilitation, while maintaining the clinical and radiographic outcomes seen with an open approach (3,4,7). In the hands of an experienced surgeon, MISS has also been shown to be cost effective, result in a shorter length of stay, and decrease the need for perioperative blood transfusions (4,8,9). The disadvantages of MISS include longer operating times, higher intraoperative radiation exposure, a learning curve for the surgeon, and increased risk of cage and pedicle screw misplacements, in addition to cage migrations (10).
Both MISS and open techniques necessitate the use of narcotics for post-operative pain management. Options for perioperative analgesia include opioid and non-opioid medications as well as patient-controlled analgesia (PCA) (either epidural or intravenous), spinal analgesia, and oral medications (11,12). Post-operative nausea and vomiting is a concern when using opioids; lower doses and alternative routes of administration can provide relief from these symptoms (12). Options for non-opioid analgesia such as gabapentin, pregabalin, acetaminophen, dexamethasone, ketamine, and nonsteroidal anti-inflammatory drugs (NSAIDs) can be considered and have been shown to be efficacious. Recent research suggests that a multimodal approach to pain control involving opioids, NSAIDs, neuromodulatory agents, acetaminophen, and extended-action local anesthesia can reduce patient exposure to narcotics while adequately controlling pain (13,14).
To compare opioid dosage through multiple modalities across MISS and open spinal surgery, we standardized the dosage using the equianalgesic conversion chart. The equianalgesic dose ratio (EDR) is an evidence-based method of correlating doses of different strength opioids when administering for pain control (15). Using conversion tables to equate differing opioid modalities is controversial. While there is literature to support its accuracy, physicians are encouraged to use clinical judgement in addition to direct conversions (16). Additionally, research suggests that MISS is associated with a shorter hospital stay when compared to open surgery (17).
Methods
This study was approved by the Institutional Review Board for a retrospective review of medical records for patients age 18 to 65 years who underwent lumbar fusion by 1 of 2 spinal surgeons over 2 years. Patients treated with minimally invasive surgery were treated with lateral lumbar interbody fusion surgery with percutaneous pedicle screws while open surgeries were open transforaminal interbody fusion cases. Exclusion criteria included patients with revision surgeries and those concurrently hospitalized for co-existing morbidities. The study group included 41 patients that underwent LLIF and 69 that had open surgery. Two surgeons performed these procedures. Surgeon A performed 60 open procedures and 13 LLIF procedures. Surgeon B performed 9 open and 28 LLIF procedures.
A retrospective analysis of 110 patients meeting the inclusion criteria was performed. Data including patient’s demographics, clinical presentation, indications for surgery, surgery performed, number of levels fused and medication administration was collected through Cerner EMR for each case. Length of hospital stay was defined as the number of days between the date of surgery to the date of discharge.
Inpatient narcotic usage was defined as narcotics used intra-operatively and narcotics used during the post-operative recovery period, including scheduled medications, PCA and pain score as recorded in the Medication Administration Record (MAR) in Cerner EMR. Peri-operative period was defined as the time from anesthesia administration on date of surgery until return to the general floor post-operatively. Opioid use was standardized using an equianalgesia chart and total dose was calculated for each patient as morphine equivalents and adjusted to patient dosage weight.
Statistics
Mean and standard deviation were used to describe total opioid dose as a continuous variable. Data was separated into two independent populations, minimally invasive vs. open surgery. Univariate analysis using a one-tailed pooled t-test was used to compare the interventions. A P value <0.05 was consider statistically significant. Other outcomes included length of hospital stay and number of spinal levels fused.
Analysis was performed using Statistical Product and Service Solutions software (version 13; SPSS, Chicago, IL).
Results
A total of 110 patients presenting for lumbar spinal fusion were included in this study. There were 41 patients included in the MISS group and 69 included in the open surgery group. The average post-operative equianalgesic dose was 278.48 mg for the MISS group. The average post-operative equianalgesic dose for the open group was 442.06 mg. Average narcotic usage post-operatively was significantly lower for the MISS group relative to those who underwent open lumbar fusion (P=0.03) (Figure 1).
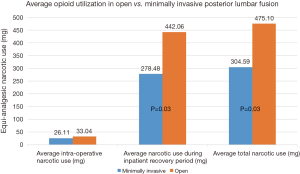
Average total narcotic use during the patient’s hospital stay was also recorded with 304.59 mg for the MISS group and 475.10 mg for the open group. A comparison of intra-operative narcotic use did not reveal a statistically significant difference (26.11 vs. 33.04 mg, P=0.06).
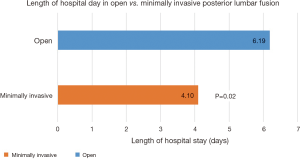
Additionally, we measured length of hospital stay for MISS patients compared to open surgery patients and found that MISS patients had an average stay of 4.10 days (STD DEV 2.4) and open surgery patients had an average stay of 6.19 days (STD DEV 6.1). The average length of post-operative hospital stay was significantly shorter for patients who underwent MISS compared to those who had an open procedure (P=0.02) (Figure 2).
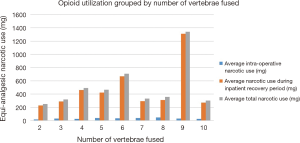
Data was also collected on opioid usage based on number of vertebrae fused. We measured average intraoperative narcotic usage as well as during the inpatient recovery period. No significant trend was found in the equianalgesic narcotic use when comparing number of vertebrae fused. This data was also stratified by MISS vs. open surgery groups and no significant difference was found (Figure 3).
Discussion
The minimally invasive technique for spinal fusion attempts to reduce iatrogenic injury to soft tissue associated with open spinal fusion (3-5). The literature supports that MISS with LLIF is associated with a decrease in soft tissue injury, blood loss, hospital length of stay, as compared to open procedure (4,8,9). In addition to recording additional data on hospital length of stay, this study examines how narcotics are used in LIFF MISS when compared to open surgery. Clarke et al. reported that approximately 3% of patients who previously did not use opioids continued use for more than 90 days after major elective surgery (18). Opioid use following orthopedic surgery can be correlated to how opioids are administered in perioperative period. According to Nora et al, in a survey 2 weeks after discharge, patients who expressed satisfaction with pain management in the hospital used significantly less opioids compared with patients who were not always satisfied (19).
The current literature has not adequately explored the amount of opioid use in the perioperative period in LLIF minimally invasive fusion techniques compared to open techniques. Previous studies have shown that high preoperative opioid use is associated with high perioperative opioid demand and continued opioid use 12 months postoperatively (20). However, these patients do not have increased intraoperative opioid use. This study demonstrated that patients who received minimally invasive lumbar fusion via LLIF had decreased overall use of opioids in the perioperative period and shorter hospital stays relative to the open procedure. Of the 41 minimally invasive surgeries included in this study, the average perioperative opioid use was significantly less than the 69 open cases. Total opioid use during the hospital course was also higher in the open surgery population. This greater exposure to opioids could correlate to a higher risk of long term opioid use. According to Clarke et al., the risk of long-term opioid use following major surgery is 3.1% (18). If perioperative opioid exposure can be reduced than perhaps long-term opioid use can be reduced.
Intraoperative narcotic usage was not statistically different between the two groups. This may be because of differences in physician preference, length of surgery, and type of anesthetics administered by anesthesia. Ketamine can decrease opioid use in the perioperative setting, which may influence our results because intraoperative anesthesia was not standardized (21). Previous literature has indicated that increased procedural invasiveness has led to increased intraoperative opioid demand, possibly secondary to more extensive soft-tissue dissection and additional instrumentation (20).
This study supports evidence from the literature that have shown MISS to have better short-term outcomes in terms of pain control and length of hospital stay relative to open surgery. In 2016, Kulkarni et al. (22) found that MISS results in significantly shorter hospital stays 4.11 days when compared to open surgery 5.84 days. This was similar to our results where we found that MISS has an average stay of 4.1 days vs. open surgery with and average stay of 6.2 days. As longer hospital stay is associated with increasing risk of morbidity to the patient, providers may consider MISS over open procedure when weighing this fact (23).
Limitations of this study include a small patient population. Patients were not matched based on demographics and were grouped only based on type of surgery. Patients were not monitored after discharge to determine opioid use after leaving the hospital. Limitations may also exist in the equianalgesic dosage chart used for conversions in this study. This may lead to opioid doses being misconstrued as higher or lower in efficacy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board of The George Washington University (No. 031558).
References
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am 2009;91:1295-304. [Crossref] [PubMed]
- Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. [Crossref] [PubMed]
- Goldstein CL, Macwan K, Sundararajan K, et al. Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res 2014;472:1727-37. [Crossref] [PubMed]
- Vazan M, Gempt J, Meyer B, et al. Minimally invasive transforaminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion: a technical description and review of the literature. Acta Neurochir (Wien) 2017;159:1137-46. [Crossref] [PubMed]
- Goldstein CL, Macwan K, Sundararajan K, et al. Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. J Neurosurg Spine 2016;24:416-27. [Crossref] [PubMed]
- Whitehouse JD, Friedman ND, Kirkland KB, et al. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol 2002;23:183-9. [Crossref] [PubMed]
- Wu AM, Chen CH, Shen ZH, et al. The Outcomes of Minimally Invasive versus Open Posterior Approach Spinal Fusion in Treatment of Lumbar Spondylolisthesis: The Current Evidence from Prospective Comparative Studies. Biomed Res Int 2017;2017. [PubMed]
- Adogwa O, Parker SL, Bydon A, et al. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech 2011;24:479-84. [PubMed]
- Cheng JS, Park P, Le H, et al. Short-term and long-term outcomes of minimally invasive and open transforaminal lumbar interbody fusions: is there a difference? Neurosurg Focus 2013;35. [Crossref] [PubMed]
- Lee KH, Yue WM, Yeo W, et al. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 2012;21:2265-70. [Crossref] [PubMed]
- Lu S, Ma SC, Wang YY, et al. Comparison of pain relief between patient-controlled epidural analgesia and patient-controlled intravenous analgesia for patients undergoing spinal fusion surgeries. Arch Orthop Trauma Surg 2015;135:1247-55. [Crossref] [PubMed]
- Wu MH, Wong CH, Niu CC, et al. A comparison of three types of postoperative pain control after posterior lumbar spinal surgery. Spine (Phila Pa 1976) 2011;36:2224-31. [Crossref] [PubMed]
- Kurd MF, Kreitz T, Schroeder G, et al. The Role of Multimodal Analgesia in Spine Surgery. J Am Acad Orthop Surg 2017;25:260-8. [Crossref] [PubMed]
- Rivkin A, Rivkin MA. Perioperative nonopioid agents for pain control in spinal surgery. Am J Health Syst Pharm 2014;71:1845-57. [Crossref] [PubMed]
- Patanwala AE, Duby J, Waters D, et al. Opioid conversions in acute care. Ann Pharmacother 2007;41:255-66. [Crossref] [PubMed]
- Berdine HJ, Nesbit SA. Equianalgesic dosing of opioids. J Pain Palliat Care Pharmacother 2006;20:79-84. [Crossref] [PubMed]
- Goldstein CL, Phillips FM, Rampersaud YR. Comparative Effectiveness and Economic Evaluations of Open Versus Minimally Invasive Posterior or Transforaminal Lumbar Interbody Fusion: A Systematic Review. Spine (Phila Pa 1976) 2016;41 Suppl 8:S74-89. [PubMed]
- Clarke H, Soneji N, Ko DT, Yun L, et al. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ 2014;348:g1251. [Crossref] [PubMed]
- Nota SP, Spit SA, Voskuyl T, et al. Opioid Use, Satisfaction, and Pain Intensity After Orthopedic Surgery. Psychosomatics 2015;56:479-85. [Crossref] [PubMed]
- Armaghani SJ, Lee DS, Bible JE, et al. Preoperative opioid use and its association with perioperative opioid demand and postoperative opioid independence in patients undergoing spine surgery. Spine (Phila Pa 1976) 2014;39:E1524-30. [Crossref] [PubMed]
- Loftus RW, Yeager MP, Clark JA, et al. Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. Anesthesiology 2010;113:639-46. [PubMed]
- Kulkarni AG, Bohra H, Dhruv A, et al. Minimal invasive transforaminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion. Indian J Orthop 2016;50:464-72. [Crossref] [PubMed]
- Pirson M, Dehanne F, Van den Bulcke J, et al. Evaluation of cost and length of stay, linked to complications associated with major surgical procedures. Acta Clin Belg 2018;73:40-9. [Crossref] [PubMed]