
Successful treatment of lumbar ligamentum flavum hematoma using a spinal full-endoscopic system
IntroductionOther Section
Lumbar ligamentum flavum hematoma (LFH) is a rare cause of lumbar nerve root and/or cauda equina compression (1-4). Accurate preoperative diagnosis is relatively difficult because of the clinical and radiological similarity with tumors, infection, epidural hematoma, and other cystic lesions. Among these differential diagnoses, discrimination from a synovial cyst originating from the facet joint (also known as facet cyst or juxta-facet cyst) is the most difficult. Even on microscopic examination, it is difficult to completely distinguish LFH from a synovial cyst, as mentioned in previous reports (5-7). One of the reasons for this difficulty may be the sampling procedure of the pathological specimen. In previous reports, the specimens were obtained by open or microscopic operative procedures. These procedures make it possible to obtain a large-sized specimen, but it is difficult to selectively obtain the hematoma capsule without intraoperative contamination. We, therefore, used a full-endoscopic system for PELD for the diagnosis and treatment of lumbar LFH and obtained a new insight into the pathogenesis.
MethodsOther Section
Between April 2017 and June 2018, 7 consecutive patients with lumbar LFH underwent percutaneous endoscopic translaminar approach (PETA) with a 7-mm diameter spinal full-endoscopic system (Richard Wolf GmbH, Knittlingen, Germany). All patients had leg pain that was resistant to medical treatment, epidural steroid injection, and/or nerve block. To avoid misdiagnosis, we excluded two initial cases which lacked pathological examination of the hematoma capsule. For all patients, PETA was conducted at only one vertebral level by a single surgeon (Hisashi Koga). Neurological examination, preoperative magnetic resonance imaging (MRI), and computed tomography (CT) were performed to determine the precise anatomic extent of the hematoma and to evaluate postoperative improvement.
Surgical technique
Patients were carefully log-rolled into the prone position. The surgery was performed under general anesthesia and simultaneous motor evoked potential monitoring. During the operation, a fluoroscope was placed across the center of the operating table to ensure appropriate positioning. An 8-mm skin and fascia incisions were made, approximately 10 mm lateral from the midline towards the just above the hematoma under fluoroscopic guidance (anteroposterior view). The following basic operative procedure has already been described in our previous report (8). In addition to the basic PETA procedure, the method of manipulation of the hematoma has been described below.
After exposure of the ligamentum flavum, the part of the ligament lining the outer surface of the hematoma was removed by forceps and a small Kerrison rongeur (VITAL Co. Ltd., Tokyo, Japan). The brownish or pinkish blood clot was also removed by forceps, and then the endoscope sheath was placed into the hematoma cavity. The inner surface of the cavity was observed closely and under magnification by the endoscope; subsequently, the presence or absence of a bleeding point was examined. If a bleeding point was found, it was electrocoagulated by a bipolar radiofrequency electrode system (Elliquence, Baldwin, NY, USA) (case No. 2, Figure S1). We also examined the continuity of the hematoma capsule and the adjacent facet joint under endoscopic visualization. Finally, pathological specimens were obtained from both, the outer and inner walls of the hematoma cavity.

ResultsOther Section
Five patients were registered for this study, three males and two females. The mean patient age was 64 years (range, 50–77 years). The onset of symptoms was acute in three patients and chronic in one patient. Even in the chronic patient, the symptoms suddenly deteriorated during conservative therapy, and MRI showed enlargement of the cystic lesion (case No. 1).
The mean operative time was 84.6 min (range, 69–98 min), and blood loss was negligible in all the patients. Symptoms improved immediately after operation in all patients. We observed no complications in this case series. The mean postoperative duration of hospital stay was 2.2 days (range, 1–4 days).
Intraoperative endoscopic findings showed a brownish to pinkish blood clot in all patients and apparent bleeding from the inner surface of the hematoma cavity in three patients. We could not observe a distinct connection between the hematoma capsule and the adjacent facet joint (Table 1). Further pathological examination supported the endoscopic evidences. A fibrin clot was observed in the specimens from all the patients, and capillary proliferation surrounding the hematoma tissue was observed in 4 out of 5 cases. However, we did not observe a synovial layer in any specimen from the hematoma capsule (Table 1).
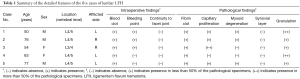
Full table
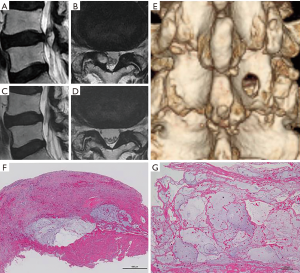
A representative case (case No. 2) is depicted in Figure 1. This 76-year-old man presented with lower back pain and right leg pain (L5 dermatome) that started 2 months prior to visiting our outpatient clinic. Neurological examination revealed a positive straight leg raise (SLR) on both sides (40°/60°), but no apparent muscle weakness. Lumbar T2-weighted MRI revealed a high intensity cystic lesion in the right juxta-facet region (Figure 1A,B). Immediately after the operation, the patient’s back and leg pain disappeared. Postoperative MRI revealed disappearance of the cystic lesion (Figure 1C,D). Postoperative three-dimensional CT scan showed appropriate bone removal of corresponding vertebral laminae (Figure 1E). Intraoperative findings revealed no continuity between the hematoma capsule and the adjacent facet joint. The apparent bleeding point on the inner surface of the hematoma cavity was also observed (Figure S1). Further pathological examination showed that the tissue surrounding the hematoma consisted of dense granulation tissue containing capillaries and myxoid degeneration (Figure 1F,G).
Another representative case (case No. 3) has been shown in Figure 2. This 54-year-old woman presented with right leg pain (L4 dermatome) that started 2 months prior to visiting our outpatient clinic. Neurological examination revealed a negative SLR and no apparent muscle weakness. Lumbar T2-weighted MRI revealed a high intensity cystic lesion in the right juxta-facet region (Figure 2A,B). Immediately after the operation, the patient’s leg pain disappeared. Postoperative MRI revealed disappearance of the cystic lesion and decompression of the cauda equina (Figure 2C,D). Postoperative three-dimensional CT scan indicated appropriate bone removal of corresponding vertebral laminae (Figure 2E). The intraoperative findings revealed no continuity between the hematoma capsule and the adjacent facet joint. The apparent bleeding point on the inner surface of the hematoma cavity was also observed (Figure S2). Further pathological examination showed that the tissue surrounding the hematoma consisted of coarse granulation tissue with abundant capillary proliferation (Figure 2F,G).


DiscussionOther Section
Lumbar LFH is a rare but distinct clinical and pathological entity causing extradural compression of nerve roots and/or cauda equina (1-4). The presence of a synovial cell layer in the pathological specimen obtained indicates that the hematoma may have originated from the adjoining facet joint (5-7). However, lumbar LFH without a synovial cell layer has also been reported in several cases (1,9-12). As we did not observe any synovial cell layer in the specimens, LFH extraneous to the synovial cyst was the most common pathological entity. In addition to this pathological finding, we also confirmed the discontinuity between the hematoma cavity and the adjacent facet joint under the endoscopic visual field. Although large surgical specimens can be obtained with open, microscopic, and microendoscopic surgeries (13-15), it is sometimes difficult to obtain a clear and bloodless visual field with these procedures.
We found slight bleeding from hematoma cavity on endoscopic observation (Figures S1,S2). As this endoscopic system allows the flow of physiological saline solution during the operation, we were able to detect even such minor bleeding. We also found capillary proliferation in 4 out of 5 pathological specimens. Especially in one case (case No. 3), more than 50% of the hematoma capsule showed capillary proliferation. Similar pathological findings have also been reported previously (9,10,12,16). These reported cases also lacked evidence of a synovial layer in their pathological specimens. These newly developed capillary vessels might be fragile and the subsequent destruction of the proliferated capillary vessels might be one of the mechanisms underlying the lumbar LFH.
The presence of myxoid degeneration (also known as mucinous/mucoid degeneration) suggested that the hematoma might have arisen from a ganglion cyst. As we also found myxoid degeneration in three cases (case No. 1, 2, and 5), LFH might have a greater association with a ganglion cyst rather than a synovial cyst. Myxoid degeneration is not a rare degenerative change of ligamentum flavum (4,17), and similar hemorrhagic ganglion cysts without a synovial layer have been reported previously (11,18). In contrast, the presence of myxoid degeneration may be a coincidental finding in elderly LFH patients because both LFH and ganglion cysts usually occur in elderly patients (2,18,19). Similarly, we also observed other degenerative changes of ligamentum flavum (hyalinization, calcification, and fibrous cartilage) in the same pathological specimens; thus, myxoid degeneration of the surrounding hematoma should be considered to be one of the alterations due to aging of the ligamentum flavum (4).
In this paper, we have summarized 5 cases of lumbar LFH treated by PELD via the PETA. Although operative time was not very short [84.6 min (range, 69–98 min)], the operative outcomes were not inferior compared to previous outcomes of open, microsurgery, and microendoscopic surgery. Owing to the minimally invasive nature of the full-endoscopic system, not only the facet joint of the patients was preserved, but the patients were also discharged and returned to their social activities immediately after the operation.
Previously, we have emphasized the significance of spinal full-endoscopic system not only for LDH, but also lumbar foraminal stenosis (8) and symptomatic discal pseudocysts (20). Other investigators have also reported the operative indication of this system for other spinal diseases, such as lateral recess stenosis (21) and lumbar aneurysmal bone cyst (22). In this report, we have also proved the significance of this system even for lumbar LFH. Although further research on the operative indication of this system is largely expected, the development of new instruments, such as forceps and a navigation system for the spinal full-endoscope, is also required.
ConclusionsOther Section
The preliminary results obtained from a small sample show that PETA is feasible for the treatment of lumbar LFH. The superiority of the spinal full-endoscopic system is not only due to the minimal invasiveness, but also due to the ability to acquire a correct diagnosis from both intraoperative and pathological findings.
AcknowledgementsOther Section
We thank all the operating room staff for their technical assistance and the medical records clerks, who helped to collect patient data. We also thank the radiological department staff for recording CT and MRI data. This work was partly supported by a grant from the Iwai Medical Foundation.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethics Committee of the Iwai Medical Foundation, and informed consent was obtained from the patients for publication of this study and any accompanying images.
ReferencesOther Section
- Ghent F, Ye X, Yan M, et al. A contrast-enhancing lumbar ligamentum flavum haematoma. BMJ Case Reports 2014. [Crossref] [PubMed]
- Ozdemir B, Kanat A, Batcik OE, et al. Ligamentum flavum hematomas: Why does it mostly occur in old Asian males? Interesting point of reported cases: Review and case report. J Craniovertebr Junction Spine 2016;7:7-12. [Crossref] [PubMed]
- Kono H, Nakamura H, Seki M, et al. Foot drop of sudden onset caused by acute hematoma in the lumbar ligamentum flavum: a case report and review of the literature. Spine (Phila Pa 1976) 2008;33:E573-5. [Crossref] [PubMed]
- Taha H, Bareksei Y, Albanna W, et al. Ligamentum flavum cyst in the lumbar spine: a case report and review of the literature. J Orthop Traumatol 2010;11:117-22. [Crossref] [PubMed]
- Xu R, Solakoglu C, Maleki Z, et al. Hemorrhagic synovial cyst: the possible role of initial trauma and subsequent microtrauma in its pathogenesis: case report. Neurosurgery 2011;68:E858-65; discussion E865.
- Cannarsa G, Clark SW, Chalouhi N, et al. Hemorrhagic lumbar synovial cyst: case report and literature review. Nagoya J Med Sci 2015;77:481-92. [PubMed]
- Nishida K, Iguchi T, Kurihara A, et al. Symptomatic hematoma of lumbar facet joint: joint apoplexy of the spine?. Spine (Phila Pa 1976) 2003;28:E206-8. [Crossref] [PubMed]
- Koga H. Improved percutaneous endoscopic translaminar approach for lumbar foraminal stenosis at L5/S1. Mini-invasive Surg 2017;1:3-5. [Crossref]
- Mizuno J, Nakagawa H, Inoue T, et al. Ligamentum flavum hematoma in the lumbar spine. Neurol Med Chir (Tokyo) 2005;45:212-5. [Crossref] [PubMed]
- Miyatake N, Aizawa T, Hyodo H, et al. Facet cyst haematoma in the lumbar spine: a report of four cases. J Orthop Surg (Hong Kong) 2009;17:80-4. [Crossref] [PubMed]
- Gazzeri R, Canova A, Fiore C, et al. Acute hemorrhagic cyst of the ligamentum flavum. J Spinal Disord Tech 2007;20:536-8. [Crossref] [PubMed]
- Takahashi H, Wada A, Yokoyama Y, et al. Ligamentum flavum haematoma: a report of two cases. J Orthop Surg (Hong Kong) 2009;17:212-5. [Crossref] [PubMed]
- Miyakoshi N, Kasukawa Y, Ando S, et al. Two-level ligamentum flavum hematoma in the lumbar spine. Case report. Neurol Med Chir (Tokyo) 2008;48:179-82. [Crossref] [PubMed]
- Takeno K, Kobayashi S, Miyazaki T, et al. Microsurgical excision of hematoma of the lumbar ligamentum flavum. Joint Bone Spine 2010;77:351-4. [Crossref] [PubMed]
- Ohba T, Ebata S, Ando T, et al. Lumbar ligamentum flavum hematoma treated with endoscopy. Orthopedics 2011;34:e324-7. [PubMed]
- Yamaguchi S, Hida K, Akino M, et al. Ligamentum flavum hematoma in the lumbar spine. Neurol Med Chir (Tokyo) 2005;45:272-6. [Crossref] [PubMed]
- Miyauchi A, Sumida T, Kaneko M, et al. Morphology and clinical importance of epidural membrane and periradicular fibrous tissue in lumbar spinal stenosis. Eur Spine J 2017;26:382-8. [Crossref] [PubMed]
- Park JH, Im SB, Kim HK, et al. Histopathological findings of hemorrhagic ganglion cyst causing acute radicular pain: a case report. Korean J Spine 2013;10:242-5. [Crossref] [PubMed]
- Miscusi M, Petrozza V, Polli FM, et al. Symptomatic ganglion cyst of ligamentum flavum as a late complication of lumbar fixation. Neurol Neurochir Pol 2012;46:82-6. [Crossref] [PubMed]
- Shiboi R, Oshima Y, Kaneko T, et al. Different operative findings of cases predicted to be symptomatic discal pseudocysts after percutaneous endoscopic lumbar discectomy. J Spine Surg 2017;3:233-7. [Crossref] [PubMed]
- Birjandian Z, Emerson S, Telfeian AE, et al. Interlaminar endoscopic lateral recess decompression-surgical technique and early clinical results. J Spine Surg 2017;3:123-32. [Crossref] [PubMed]
- Shibuya I, Dezawa A, Urayama S, et al. Surgical treatment of a lumbar aneurysmal bone cyst using percutaneous endoscopic lumbar discectomy. Eur Spine J 2018;27:368-74. [Crossref] [PubMed]
- Kaneko T, Oshima Y, Inoue H, et al. Intraoperative video in a patient with lumbar ligamentum flavum hematoma (case 2): after insertion the endoscope into the hematoma cavity, we could find slight bleeding. Asvide 2018;5:911. Available online: http://www.asvide.com/article/view/28927
- Kaneko T, Oshima Y, Inoue H, et al. Intraoperative video in a patient with lumbar ligamentum flavum hematoma (case 3): after insertion the endoscope into the hematoma cavity, we could find slight bleeding. Asvide 2018;5:912. Available online: http://www.asvide.com/article/view/28928


