
Baseline mental status predicts happy patients after operative or non-operative treatment of adult spinal deformity
Introduction
Adult spinal deformity (ASD) is a malalignment of the aging spine associated with significant impacts to health related quality of life (HRQL). ASD is a common medical disorder, with reported prevalence as high as 32% of the general population, and up to 68% in elderly populations (1-5). Treatment plans aim to reduce pain and improve function, and include conservative measures such as physical or exercise therapy, bracing, anti-inflammatories, and epidural steroid injections, as well as operative treatment (1,6,7). Previous studies have reported ASD patients to have significantly high rates of associated perioperative complications and comorbidities, specifically complication rates of 22.2% (7), 26.8% (8), 39.5% (9) 62% (10), and comorbidity rates of 50.81% (11), 58% (9), and 71% (10). Physical and functional limitations of ASD are known to significantly impact a patient’s psychological status, resulting in an abundance of comorbid psychiatric diagnoses including stress, anxiety and depression (1,12-14).
Previous studies have shown rates of self-reported depression in ASD patients to be 24.7% (15) and 43% (12), as well as rates of patient preoperative anti-depressant utilization to be as high as 85.1% (16). Baseline depression has been reported to predict development of any medical complication as well (8). The effect of lower baseline mental status on treatment outcomes is currently a trending and controversial topic in the literature. Numerous studies have reported baseline depression to be associated with comparatively worse or adverse treatment and HRQL outcomes (12,13,16,17), while others have reported no association at all (15). While the majority of literary reports investigating the impact of mental health burdens on treatment outcomes focus on predicting the occurrence of adverse outcomes, to the best of our knowledge, none have focused on identifying factors that predict non-depressed, satisfied patients with a good self-image score.
The goal of our study was to determine which factors best predicted non-depressed, satisfied ASD patients with a good self-image at 2-year follow-up, using HRQL and treatment outcome metrics such as the Oswestry disability index (ODI), the numerical rating scale (NRS), the Short-Form-36 version 2 (SF-36), and the Scoliosis Research Society-22r (SRS-22r) questionnaires for patients undergoing operative and non-operative treatments.
Methods
Data source
This study is a retrospective review of a multi-center database of consecutively enrolled ASD patients from 2008–2015 from 12 participating centers in the United States. Database inclusion criteria consisted of patients ≥18 years old, seeking operative or non-operative treatment for ASD. ASD is defined radiographically in this database as: coronal Cobb angle ≥20°, sagittal vertical axis (SVA, distance between C7 plumb line and sacral posterior superior margin) ≥5 cm, pelvic tilt (PT) ≥25° and/or thoracic kyphosis >60°. Database exclusion criteria were spinal deformity of neuromuscular etiology, presence of active infection, or malignancy. Internal Review Board approval was obtained at each participating site prior to study initiation and informed consent was obtained from each patient at enrollment.
Data collection
Descriptive data collected included demographic variables such as age, sex, Charlson comorbidity index (CCI), frailty score, base line (BL) and 2-year follow-up (2Y) radiographic profiles [sagittal vertical angle (SVA), pelvic incidence minus lumbar lordosis (PI-LL), PT], and having a history of depression or psychological disorder. Surgical measures included type of approach, procedure, length of stay (LOS), operative time, estimated blood loss (in cc), cell save, reoperation rates, and surgically related complication rates. Outcome measures assessed were standardized HRQL measures such as the modified ODI, the NRS scores of leg pain, the SF-36 physical component score (PCS), mental component scores (MCS), and various sub-domains including physical functioning (PF), physical role functioning (RP), emotional role functioning (RE), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), and mental health (MH). The SRS-22r total scores and sub-domains [activity, pain, self-image (perception of deformity), mental, satisfaction] were also assessed (18-20). Questionnaires were administered and collected at baseline BL and 2Y post-operative follow-up.
Inclusion criteria and patient stratification
Inclusion criteria consisted of primary ASD patients >18 years old, with follow-up data up to 2 years. Patients were further stratified into ‘happy’ and ‘control’ groups. ‘Happy’ group consisted of patients without clinical depression at 2Y (defined as SF 36 MCS >42), satisfied with treatment (SRS 22 Satisfaction >3), and with good self-image (SRS 22 Self-Image >3). ‘Control’ groups consisted of patients not included within the ‘happy’ group. Happy patients that underwent surgery (OP) were then propensity score matched to patients within the control group, by BL and 2Y sagittal deformity, leg pain, CCI, and frailty scores. Happy patients that did not undergo surgery (NOP) were matched by BL scores of the aforementioned variables.
Statistical analysis
Descriptive statistics were used to quantify demographic variables such as age, sex, and radiographic profiles. Demographic, surgical, and outcome measures were compared among happy and control groups using student t-tests for continuous variables, and Chi-Square analysis for categorical variables. Binary forward stepwise logistic regression models were used to identify independent predictors of ‘happy’ patients in both the OP and NOP cohorts. Thresholds of factors that predicted happy patients were calculated using area under the curve (AUC) and 95% confidence interval (CI). The level of significance was set to P<0.05. All statistical tests were performed using IBM SPSS Statistics Version 23.0 (Armonk, NY: IBM Corp.) and R version 3.3.1 (2016-06-21) Copyright (C) 2016 The R Foundation.
Results
Descriptions
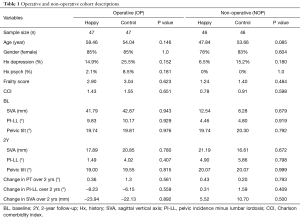
A total of 480 patients were included. Of the 480 patients, 263 underwent operations. Of the operative patients, 126 (47.9%) were happy (P=0.001). Of the happy patients, 47 were successfully propensity score matched to patients within the control group, creating a total of 94 patients (OP). The non-operative propensity score match (NOP) resulted in a total of 92 patients (46 happy vs. 46 control). In both OP and NOP, happy and control groups had similar age, gender, frailty score, history (Hx) of depression/psychological disorders, and radiographic profiles (P>0.05) (Table 1).
Full table
Surgical measures
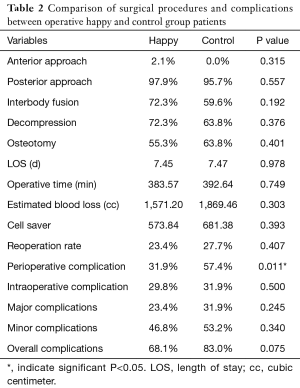
Within the operative cohort, there was insignificant variation (P>0.05) between Happy and Control groups in regards to the anterior approach, posterior approach, interbody fusion rates, decompressions, and osteotomies. Posterior fusions were the most common approach, accounting for 97.9% of happy patients and 95.7% of control patients. Measures such as LOS (7.45, 7.47 days), operative time (383.57, 392.64 min), blood loss (1,571.20, 1,869.46 cc), cell saver use (573.84, 681.38), and reoperation rates (23.4%, 27.7%) were all similar (P>0.05) between happy and control groups. Perioperative complication rates were significantly lower in happy patients (31.9% vs. 57.4%, P=0.011). Intraoperative complications, major complications, minor complications, and overall complication rates were similar between happy and control groups (P>0.05) (Table 2).
Full table
HRQL outcomes
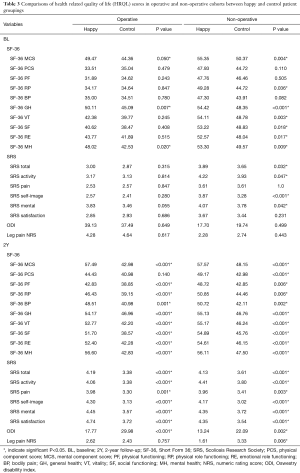
At 2Y, happy had significantly better ODI in both cohorts (OP: 17.77 vs. 29.98, NOP: 13.24 vs. 22.09). In NOP, happy had significantly better leg pain NRS scores (1.61 vs. 3.33, P=0.006). At baseline, the OP cohort was similar (P>0.05) in all HRQL measurements, with the exceptions of ‘Happy’ having higher SF36 MCS (49.47 vs. 44.36, P=0.050), SF36 GH (50.11 vs. 45.09, P=0.007), and SF36 MH scores (48.02 vs. 42.53, P=0.020). At baseline for the NOP cohort, Happy had significantly higher SF36 MCS, SF36 RP, SF36 GH, SF36 VT, SF36 SF, SF36 RE, SF36 MH, SRS activity, SRS self-image, SRS mental, and SRS total scores (P<0.05). For the OP cohort, happy had significantly better 2Y scores among all HRQL measures (P<0.05) except for SF36 PCS. For the NOP cohort, happy patients had significantly better 2Y scores among all HRQL measures (P<0.05) (Table 3).
Full table
Logistic regression models
Regression models determined BL SRS mental score (OR: 2.199, B coeff: 0.788, AUC 0.617, 95% CI: 1.199–4.033) and overall ODI improvement (OR: 1.055, B coeff: 0.044, AUC 0.717, 95% CI: 1.022–1.089) to be significant (P<0.05) independent indicators of becoming a ‘happy’ patient in the OP cohort at 2Y. Thresholds were (BL SRS mental >2.5 and ODI improvement >12). BL SRS self-image (OR: 5.195, B coeff: 1.648, AUC 0.740, 95% CI: 2.109–12.795) and overall ODI improvement (OR: 1.087, B coeff: 0.84, AUC 0.683, 95% CI: 1.025–1.153) were determined to be significant (P<0.05) independent indicators of becoming a ‘Happy’ patient in the NOP cohort at 2Y. Thresholds were (BL SRS self-image >3.5 and ODI improvement >9).
Discussion
While metrics such as frailty, LOS, complication rates, relief from pain, and correction of deformity remain some of the most commonly used treatment outcome assessments in the literature (21-24), a patient’s satisfaction is also one of the most important measures of treatment success (25-27). Currently, little is known as to what specifically drives satisfaction, good mental status, and development of good deformity perception in adult spinal deformity patients. Establishing a greater understanding of what makes ASD patients ‘happier’ with their treatment, will bolster management strategies and help guide treatment decisions.
This study found that for ‘happy’ and control groups of operative ASD patients at 2-year follow-up (with matched base-line and 2-year follow-up metrics for sagittal deformity, leg pain, comorbidity score and frailty status), ‘happy’ patients had significantly improved 2-year follow-up disability scores, physical functioning, role functioning, bodily pain, general health, vitality, social functioning, activity, self-image, satisfaction, mental health, and less perioperative complications in comparison to the control groups. In regards to Happy and control groups of non-operative ASD patients at 2-year follow-up (with matched base-line metrics for sagittal deformity, leg pain, comorbidity scores and frailty status), happy patients had significantly better disability scores, leg pain, mental component scores, physical component scores, physical functioning, role functioning, bodily pain, general health, vitality, social functioning, activity, self-image, satisfaction and mental health in comparison to the control groups. Logistic regressions revealed base-line SRS mental score and overall disability score (ODI) improvement to significantly predict becoming a ‘happy’ operative patient at 2-year follow-up. Base-line SRS self-image score and overall ODI improvement significantly predicted becoming a ‘happy” non-operative patient at 2-year follow-up.
Our findings make it apparent that a patient’s happiness and satisfaction at 2-year follow-up are significantly associated with positive HRQL outcomes. The debilitating nature of ASD is well known to have significant effects on a patient’s psychological health (28), and baseline mental health is reported to be associated with treatment outcomes (12,13,15-17). In both our operative and non-operative cohorts of ‘happy’ patients at 2-year follow-up, baseline values for SF36 mental component scores, mental health scores, and SRS mental scores were significantly better compared to the control group (with the exception of SRS mental scores for operative patients, which is just shy of reaching significance). This is consistent with the majority of literary reports that describe lower baseline mental health status adversely affecting various HRQL and disability outcomes (12,13,16,17).
The association between baseline mental status and treatment outcomes is exemplified in our operative cohort. Patients within both the happy and control groups, all of which who had statistically similar baseline deformities, underwent comparable surgeries (statistically insignificant variances in approaches, techniques, LOS, operative time, blood loss, cell saver use, and intra-operative complications), and who had achieved similar post-operative sagittal alignment, patients within the ‘happy’ group had significantly better disability outcomes and HRQL. Both happy and control patients also had comparable post-operative major, minor, and overall complication rates, most likely indicating equivalent post-operative care, and further strengthening the association between baseline mental status and treatment outcomes.
Previous reports have indicated that treatment dissatisfaction is associated with worse pain, disability, and function scores for patients who were younger or depressed (29). In our operative cohort, control group patients were on average 4 years younger, almost reaching a significant difference in age relative to the happy group. This is consistent with previous findings, in that our younger control cohort experienced less HRQL and disability improvements relative to the happy group. While this may cause concern that the age difference of our cohort confounds our results, patient age failed to make it into our regression equations after multiple adjustments. In our non-operative group, patients with in the control group were on average 6 years older, nearly reaching significance. Our non-operative control group showed similar result trends in relation to our operative control group, further strengthening our associations between patient satisfaction and positive HRQL/disability outcomes.
Previously, it has also been unclear as to what factors specifically drive a patient’s overall satisfaction. Recent studies have reported 2-year follow-up patient satisfaction to be moderately correlated with HRQL outcomes such as final ODI, SF-36, SRS-total, and VAS scores. Patients with high levels of satisfaction were also found to have statistically equal pre or postoperative radiographic profiles to patients with low levels of satisfaction. Occurrences of complications were also shown to have no effect on patient satisfaction. No association between radiographic deformity, complications, and only moderate HRQL correlations with increased patient satisfaction, have lead researchers to believe that patient expectations and the patient-physician relationship may play a greater role in patient satisfaction and treatment outcomes than previously thought (30).
While it is difficult to quantify how greatly the patient-physician relationship affects a patient’s overall satisfaction and treatment outcomes, our analysis points to quantifiable factors of baseline mental status, self-perception of deformity, and overall disability improvement as indicators of satisfied, non-depressed patients with a positive perception of their deformity. Patients who were ‘happy’, had significantly improved ODI scores and HRQL measures in comparison to control patients, in both operative and non-operative cohorts. Further investigation is needed for a complete understanding of the relationships between baseline mental health status, baseline self-perception of deformity, and disability score improvement on 2-year follow-up patient happiness and HRQL outcomes.
Limitation
The associations shown in our study and previous studies are useful in isolating relationships that warrant further scrutiny, but it is difficult to determine whether patients were dissatisfied because of worse disability outcomes, satisfied because of better outcomes, or if disability outcomes and HRQL scores are a result of a patient’s satisfaction level. Our study is also limited by a relatively small sample size. More powerful studies may describe different associations and change the nature of our results. As with all database studies, the data used is dependent on the accuracy of the inputters. While 12 institutions supply the database used with ASD patients, sampling bias may also occur, dependent on the institution, location, and physician.
Conclusions
This was a retrospective review of a multi-center database of consecutively enrolled ASD patients from 2008–2015 from 12 participating centers in the United States. Satisfied, non-depressed adult spinal deformity patients with superior self-image (happy) were propensity score matched with non-happy control patients with ASD in both operative and non-operative cohorts. Baseline mental status, self-image, and overall disability (ODI) improvement significantly predicted satisfied, non-depressed ASD patients with superior perceptions of deformity. Happy patients were associated with significantly improved HRQL and disability score outcomes at 2-year follow-up in comparison to non-happy patients, with operative happy patients displaying 13 points of better disability scores and 9 for non-operative patients. Relationships between baseline mental status, self-image, patient happiness, disability improvements, and HRQL outcomes require further investigation. It is recommended that clinicians assess baseline mental health status, and tailor management strategies accordingly to maximize HRQL and treatment outcomes.
Acknowledgements
The International Spine Study Group is funded through grants from DePuy Spine and individual donations.
Footnote
Conflicts of Interest: E Klineberg (DePuy Synthes—consulting, Stryker—consulting, Springer—consulting, Trevana—consulting, AOSpine—honoraria, fellowship support, K2M—honoraria); V Lange (Nemaris—stock ownership, DePuy Synthes—teaching/speaking, Nuvasive—teaching/speaking, K2M—teaching/speaking, Medtronic—teaching/speaking, Nemaris—board of directors); F Schwab (Zimmer Biomet—speaking/teaching, consulting, royalties/patents, NuVasive—speaking/teaching, consulting, royalties/patents, K2M—speaking/teaching, consulting, royalties/patents, MSD—speaking/teaching, consulting, royalties/patents, Medicrea—speaking/teaching, consulting, Nemaris—board of directors, shareholder); PG Passias (Medicrea—consulting, SpineWave—consulting, Allosource—Scientific Advisory Board, Zimmer Biomet—teaching/speaking, Globus—teaching/speaking, CSRS—grant, Aesculap—research study). The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional/regional/national ethics committee/ethics board of New York University School of Medicine (No. 17-00565) and written informed consent was obtained from all patients.
References
- Ames CP, Scheer JK, Lafage V, et al. Adult Spinal Deformity: Epidemiology, Health Impact, Evaluation, and Management. Spine Deform 2016;4:310-22. [Crossref] [PubMed]
- Pérennou D, Marcelli C, Hérisson C, et al. Adult lumbar scoliosis. Epidemiologic aspects in a low-back pain population. Spine (Phila Pa 1976) 1994;19:123-8. [Crossref] [PubMed]
- Francis RS. Scoliosis screening of 3,000 college-aged women. The Utah Study--phase 2. Phys Ther 1988;68:1513-6. [PubMed]
- Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: results from the first National Health and Nutrition Examination Survey. Int J Epidemiol 1987;16:537-44. [Crossref] [PubMed]
- Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30:1082-5. [Crossref] [PubMed]
- Daniels AH, DePasse JM, Eberson CP, et al. Adult Spinal Deformity: Contemporary Treatment and Patient Outcomes. R I Med J (2013) 2015;98:32-41. [PubMed]
- La Maida GA, Luceri F, Gallozzi F, et al. Complication rate in adult deformity surgical treatment: safety of the posterior osteotomies. Eur Spine J 2015;24 Suppl 7:879-86. [Crossref] [PubMed]
- Soroceanu A, Burton DC, Oren JH, et al. Medical Complications After Adult Spinal Deformity Surgery: Incidence, Risk Factors, and Clinical Impact. Spine (Phila Pa 1976) 2016;41:1718-23. [Crossref] [PubMed]
- Bhagat S, Vozar V, Lutchman L, et al. Morbidity and mortality in adult spinal deformity surgery: Norwich Spinal Unit experience. Eur Spine J 2013;22 Suppl 1:S42-6. [Crossref] [PubMed]
- Acosta FL Jr, McClendon J Jr, O'Shaughnessy BA, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: complications and predictive factors. J Neurosurg Spine 2011;15:667-74. [Crossref] [PubMed]
- Worley N, Marascalchi B, Jalai CM, et al. Predictors of inpatient morbidity and mortality in adult spinal deformity surgery. Eur Spine J 2016;25:819-27. [Crossref] [PubMed]
- Bakhsheshian J, Scheer JK, Gum JL, et al. Impact of poor mental health in adult spinal deformity patients with poor physical function: a retrospective analysis with a 2-year follow-up. J Neurosurg Spine 2017;26:116-24. [Crossref] [PubMed]
- Bakhsheshian J, Scheer JK, Gum JL, et al. Comparison of Structural Disease Burden to Health-related Quality of Life Scores in 264 Adult Spinal Deformity Patients With 2-Year Follow-up: Novel Insights into Drivers of Disability. Clin Spine Surg 2017;30:E124-31. [Crossref] [PubMed]
- Schwab FJ, Hawkinson N, Lafage V, et al. Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 2012;21:2603-10. [Crossref] [PubMed]
- Theologis AA, Ailon T, Scheer JK, et al. Impact of preoperative depression on 2-year clinical outcomes following adult spinal deformity surgery: the importance of risk stratification based on type of psychological distress. J Neurosurg Spine 2016;25:477-85. [Crossref] [PubMed]
- Elsamadicy AA, Adogwa O, Lydon E, et al. Depression as an independent predictor of postoperative delirium in spine deformity patients undergoing elective spine surgery. J Neurosurg Spine 2017;27:209-14. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Lafage V, et al. Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up. J Neurosurg Spine 2015;23:349-59. [Crossref] [PubMed]
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473-83. [Crossref] [PubMed]
- Asher MA, Lai SM, Glattes RC, et al. Refinement of the SRS-22 Health-Related Quality of Life questionnaire Function domain. Spine (Phila Pa 1976) 2006;31:593-7. [Crossref] [PubMed]
- Oglesby M, Fineberg SJ, Patel AA, et al. Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine (Phila Pa 1976) 2013;38:1226-32. [Crossref] [PubMed]
- Armaghani SJ, Lee DS, Bible JE, et al. Increased Preoperative Narcotic Use and Its Association With Postoperative Complications and Length of Hospital Stay in Patients Undergoing Spine Surgery. Clin Spine Surg 2016;29:E93-8. [Crossref] [PubMed]
- Goz V, Weinreb JH, Schwab F, et al. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nationwide Inpatient Sample database. Spine J 2014;14:2019-27. [Crossref] [PubMed]
- Puvanesarajah V, Jain A, Kebaish K, et al. Poor Nutrition Status and Lumbar Spine Fusion Surgery in the Elderly: Readmissions, Complications, and Mortality. Spine (Phila Pa 1976) 2017;42:979-83. [Crossref] [PubMed]
- Pakarinen M, Koivumaa-Honkanen H, Sinikallio S, et al. Life dissatisfaction burden is associated with a poor surgical outcome among lumbar spinal stenosis patients: a 5-year follow-up study. Int J Rehabil Res 2014;37:80-5. [Crossref] [PubMed]
- Passias PG, Soroceanu A, Yang S, et al. Predictors of Revision Surgical Procedure Excluding Wound Complications in Adult Spinal Deformity and Impact on Patient-Reported Outcomes and Satisfaction: A Two-Year Follow-up. J Bone Joint Surg Am 2016;98:536-43. [Crossref] [PubMed]
- Hart RA, Hiratzka J, Kane MS, et al. Stiffness After Pan-Lumbar Arthrodesis for Adult Spinal Deformity Does Not Significantly Impact Patient Functional Status or Satisfaction Irrespective of Proximal Endpoint. Spine (Phila Pa 1976) 2017;42:1151-7. [Crossref] [PubMed]
- Bess S, Line B, Fu KM, et al. The Health Impact of Symptomatic Adult Spinal Deformity: Comparison of Deformity Types to United States Population Norms and Chronic Diseases. Spine (Phila Pa 1976) 2016;41:224-33. [Crossref] [PubMed]
- Sinikallio S, Aalto T, Airaksinen O, et al. Lumbar spinal stenosis patients are satisfied with short-term results of surgery - younger age, symptom severity, disability and depression decrease satisfaction. Disabil Rehabil 2007;29:537-44. [Crossref] [PubMed]
- Hamilton DK, Kong C, Hiratzka J, et al. Patient Satisfaction After Adult Spinal Deformity Surgery Does Not Strongly Correlate With Health-Related Quality of Life Scores, Radiographic Parameters, or Occurrence of Complications. Spine (Phila Pa 1976) 2017;42:764-9. [Crossref] [PubMed]


