
Objective monitoring of activity and Gait Velocity using wearable accelerometer following lumbar microdiscectomy to detect recurrent disc herniation
Introduction
Surgical management of spinal pathologies have been associated with substantial resource management and cost (1,2). Therefore, efficient monitoring and evaluation of pre- and post-surgical outcome is imperative for the patient, healthcare provider and also from a community perspective (3). Monitoring of surgical technique effectiveness, discharge disposition and functional outcome of patients are essential for efficient delivery of care as well as facilitating identification of appropriate resource allocation (4). This increases the need for the use of objective measuring tools to monitor mobility and post intervention recovery of patients (5).
Traditionally, quantification and comparison of recovery or outcomes in patient’s post-spinal procedures used subjective rating scores such as Oswestry Disability Index (ODI), Visual Analogue pain Scale scores (VAS), Short Form Health (SF-12, SF-36) survey scores amongst a variety of others (6-8). However, the major problem in utilizing these scores is their subjectivity and the inherent bias with self-appraisal, as different individuals perceive and tolerate pain differently (9). Recent literature states that the ODI should not be a stand-alone tool for evaluating walking limitation in patients with lumbar spinal stenosis (10). For comprehensive assessment of walking ability, an objective walking test should be utilized in order to assess walking capacity. Wearable technologies such as accelerometers should be incorporated as a standardized tool for measuring walking performance; used in conjunction with the walking test (10,11).
There have been multiple case studies on the effectiveness of wearable accelerometers post spinal surgery, for instance recovery post minimally invasive fusion (9). The first clinical series using accelerometers for monitoring post spinal surgery recovery was published in 2016 (12). With the recent advancement in medical wearables/wireless accelerometers, we have the capability to monitor and track, in real time, up-to-date patient’s functional mobility including step counts and daily walking/running distance (13). The benefit of such technology is the ability to provide a continuous objective measure of the patient’s daily activity to the surgeon, or health care practitioner. This data stream can be used as a measure of the extent of recovery and ambulatory function. Coupled with the follow-up reports of subjective measures (such as pain and disability scores), an improved understanding of a patient’s progress can be achieved.
This case report explores the use of wireless accelerometer technology in a patient that had a lumbar microdiscectomy, with objective mobility and functional outcomes measured [distance travelled and Gait Velocity (GV)] both preoperatively and up to 3-month postoperatively.
Case presentation
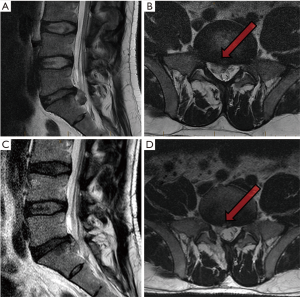
A 39-year-old male presented with sciatica over a period of 6 months. His symptoms had a negative effect on quality of life, both personal and work-related. His medical history was unremarkable. MRI revealed a large volume L5/S1 disc herniation (Figure 1A,B), with no improvement with prolonged conservative care; a lumbar microdiscectomy was recommended.
The patients’ distance travelled (kms), daily step count (DSC) and GV were monitored for 1-week pre-operative, and subsequently over 3-month post operation using an Apple Watch (Apple, San Francisco, CA, USA). Accelerometers are common tools used for quantification of physical activity, free from the bias of traditional subjective measuring methods. The Apple Watch monitored and tracked the DSC, focused activity (minutes), estimated caloric expenditure, distance travelled and GV. The advantage is that individual patient parameters can be adjusted according to user age, weight, sex and height. The Apple Watch was worn during all waking hours.
An L5/S1 microdiscectomy was performed with no perioperative complications experienced. The patient was discharged within 24 hours, and returned to his accounting occupation and light duties after 2 weeks. Accelerometer data in the week prior to the operation showed the patient averaging a DSC of less than 2,500, over a daily distance of less than 1.6 km, with a GV of 0.97 m/s. In the first postoperative week, the patient’s mobility was slightly improved, with a daily distance over 3 km, with a slight increase in GV over 1.0 m/s. By the second postoperative week, the parameters had improved well beyond baseline levels, continuing to increase in the subsequent weeks (Figures 2,3). At 1-month follow-up, the patient averaged over 4,500 DSC, for a distance of 3.8 km, and a GV of 1.58 m/s; a 60% improvement in both steps taken and GV in comparison to pre-operation numbers (Figure 3).


From the results yielded, there was a considerable improvement in all subjective measurements (VAS back and leg pain scores, ODI and SF-12) observed at 1-month follow-up compared to baseline scores; with VAS leg pain reduced from 8 to 2, and ODI reduced from 46 to 8. Thus, an intrinsic correlation between changes in ODI score and physical improvement at follow-up was quantified by accelerometer data.
On day 57, accelerometer data recorded an acute deterioration in DV and activity levels, correlating with the patient experiencing a recurrence of pain. Based on subjective information as well as the objective findings of gait deterioration, an MRI scan was organized (Figure 1C,D) which demonstrated a recurrent disc herniation. Redo surgery was performed on day 62 using a tubular retractor system, once more, with no perioperative complications. In the following days, the patient experienced rapid functional restoration and return to his continued progression prior to the recurrent episode in regards to the objective parameters of DSC, distance travelled and GV.
Discussion
Although there is a rising number of pilot studies reporting the use of accelerometers for evaluating function and recovery following a medical intervention (14-16), there have been limited studies in which medical wearables have been utilized within the scope of spine surgery. With regards to this case, postoperative objective accelerometer measurements demonstrated improvements of 60% in distance walked per day, number of steps taken and GV at 1-month follow-up, compared to pre-operative measures. The sudden drop in functional status at day 57 was prominent, thus verifying the value of objective measurements with assistance in identifying the postoperative complication, such as recurrent disc herniation, a common yet undesirable outcome of microdiscectomy (17,18).
As discussed, functional recovery post spinal procedures is currently reported via proxy parameters such as quality of life, pain and functional scores (VAS, ODI, SF12/SF36, Roland Morris disability index), and duration of hospital stay (8). However, subjective measures alone are strongly influenced by inherent bias and individual variation. As patients have different expectations of pain and functional tolerance, these subjective measurements inevitably result in a lack of standardization of outcomes evaluation across different surgical procedures (19,20). Compensation, psychological influences and litigious activity which may or may not be associated with their surgical interventions can confer potentially signification variances of self-reported measures of quality of life scores (21).
Advances in medical wearables including accelerometers, gyroscopes and global positioning systems (GPS), have led to the dawn of real-time recording, reporting and assessing objective patient recovery, free of subjectivity. Our report is an example of the benefits of wireless technology in assessing the outcome of microdiscectomy surgery, with real-time reporting to the health care professional, with rapid identification of the relevant complication of recurrent disc herniation.
The use of GV as an instrument for objective measurement has long been deliberated in the literature (22), with evidence leading to the conclusion that it serves as an accurate indicator of a patient’s level of physical mobility and general health status. Step count has been investigated for its use (23) in the clinical setting, and has led to the result that with an average of at least 4,300 steps per day, this translates to one less day in hospital per 3 years of life; giving credibility to its association with musculoskeletal conditions. Objective gait parameters serve the purpose to convert the observation of impaired mobility, into an objective ‘scorable’ context. This leads into avenues of utilizing these instruments as a potent screening tool to allow for efficient identification and treatment of musculoskeletal and neurological injury/disease in patients, as shown by this case report, by the use of simple wearable technologies.
In the time period before the recurrence on day 57, all three objective measurements (DSC, GV, Activity) show constant improvement and thus reflect a positive post-operative outcome. At the return of pain and the short period thereafter, a depression in the all three indicators is noted which subsequently facilitated the MRI scan, and diagnosis of recurrent disc herniation. This diagnosis may not have been made as efficiently if it were not for the measurement of gait velocity, step distance and count as objective tools used in the monitoring of this patient pre- and post-operation; potentially evading further consequence.
The data obtained from the accelerometer showed a strong improvement in GV, distance travelled and steps taken; all within the first month post-surgery. Self-reported scores such as ODI were taken at the standard time points of 6 weeks and 3 months, however they were not predictive of deterioration in function as seen in this patient. A continuous stream of objective information via the wearable accelerometer proved to be essential in the early detection of complications, and efficient delivery of appropriate follow on care.
Conclusions
As demonstrated in this case, the use of a continuous objective measuring tool is invaluable particularly in detecting sudden change or deterioration of function. Until 12 months post-operation the patient continued to wear the Apple Watch with no further issues and maintained a GV of over 1.5 m/s. Self-reported subjective index scores were not used for long-term follow-up. As a result of this case study, we recommend the use of accelerometers for quantifying physical activity post spine surgery as a feasible outcomes measurement tool. Combined with subjective measurements, wearable devices that monitor objective outcomes provide substantial benefit in tracking patient progress. Further advancement or improvements of objective measurements may eventually replace the current subjective measurement tools, and the elimination of bias; however, their use and benefits should be validated in larger prospective studies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the South Eastern Local Health District Human Research Ethics Committee, with the reference number 17/184. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Deyo RA, Gray DT, Kreuter W, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30:1441-5; discussion 1446-7. [Crossref] [PubMed]
- Weinstein JN, Lurie JD, Olson PR, et al. United States' trends and regional variations in lumbar spine surgery: 1992-2003. Spine (Phila Pa 1976) 2006;31:2707-14. [Crossref] [PubMed]
- Wearables in spine surgery: Beginnings, research and real-world applications. In: spinal news international. 2017. Available online: https://spinalnewsinternational.com/wearables/. Accessed 30/11/2018.
- Soegaard R, Christensen FB. Health economic evaluation in lumbar spinal fusion: a systematic literature review anno 2005. Eur Spine J 2006;15:1165-73. [Crossref] [PubMed]
- Pryce R, Johnson M, Goytan M, et al. Relationship between ambulatory performance and self-rated disability in patients with lumbar spinal stenosis. Spine (Phila Pa 1976) 2012;37:1316-23. [Crossref] [PubMed]
- Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63:S240-52. [Crossref] [PubMed]
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- Teles AR, Khoshhal KI, Falavigna A. Why and how should we measure outcomes in spine surgery? Journal of Taibah University Medical Sciences 2016;11:91-7. [Crossref]
- Phan K, Mobbs RJ. Long-Term Objective Physical Activity Measurements using a Wireless Accelerometer Following Minimally Invasive Transforaminal Interbody Fusion Surgery. Asian Spine J 2016;10:366-9. [Crossref] [PubMed]
- Jespersen AB, Gustafsson M. Correlation between the Oswestry Disability Index and objective measurements of walking capacity and performance in patients with lumbar spinal stenosis: a systematic literature review. Eur Spine J 2018;27:1604-13. [Crossref] [PubMed]
- Sun J, Liu YC, Yan SH, et al. Clinical Gait Evaluation of Patients with Lumbar Spine Stenosis. Orthop Surg 2018;10:32-9. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Maharaj M, et al. Physical Activity Measured with Accelerometer and Self-Rated Disability in Lumbar Spine Surgery: A Prospective Study. Global Spine J 2016;6:459-64. [Crossref] [PubMed]
- Rand D, Eng JJ, Tang PF, et al. How active are people with stroke?: use of accelerometers to assess physical activity. Stroke 2009;40:163-8. [Crossref] [PubMed]
- Culhane KM, Lyons GM, Hilton D, et al. Long-term mobility monitoring of older adults using accelerometers in a clinical environment. Clin Rehabil 2004;18:335-43. [Crossref] [PubMed]
- Dalton A, Khalil H, Busse M, et al. Analysis of gait and balance through a single triaxial accelerometer in presymptomatic and symptomatic Huntington's disease. Gait Posture 2013;37:49-54. [Crossref] [PubMed]
- Sumukadas D, Laidlaw S, Witham MD. Using the RT3 accelerometer to measure everyday activity in functionally impaired older people. Aging Clin Exp Res 2008;20:15-8. [Crossref] [PubMed]
- Choy WJ, Phan K, Diwan AD, et al. Annular closure device for disc herniation: meta-analysis of clinical outcome and complications. BMC Musculoskelet Disord 2018;19:290. [Crossref] [PubMed]
- Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus 2003;15:E10. [PubMed]
- Bassett DR Jr, Cureton AL, Ainsworth BE. Measurement of daily walking distance-questionnaire versus pedometer. Med Sci Sports Exerc 2000;32:1018-23. [Crossref] [PubMed]
- Tudor-Locke CE, Myers AM. Challenges and opportunities for measuring physical activity in sedentary adults. Sports Med 2001;31:91-100. [Crossref] [PubMed]
- Mobbs RJ, Gollapudi PR, Chandran NK. Outcome following anterior cervical discectomy in compensation patients. J Clin Neurosci 2001;8:124-5. [Crossref] [PubMed]
- Montero-Odasso M, Schapira M, Varela C, et al. Gait velocity in senior people. An easy test for detecting mobility impairment in community elderly. J Nutr Health Aging 2004;8:340-3. [PubMed]
- Ewald BD, Oldmeadow C, Attia JR. Daily step count and the need for hospital care in subsequent years in a community-based sample of older Australians. Med J Aust 2017;206:126-30. [Crossref] [PubMed]


