The implementation of enhanced recovery after surgery (ERAS) in complex spinal surgery
Introduction
Enhanced recovery after surgery (ERAS) is not a new concept; it was developed in 1997 in Denmark by Professor Kehlet (1) and has since been adopted globally in various surgical specialties. The multimodal approach shows that a better post-operative recovery can be achieved by focusing on a number of factors to reduce the surgical stress response. The concept involves 3 main principles; getting the patient in the best possible condition for surgery, ensuring the patient has the best possible management during their operation and ensuring the patient has the best post-operative rehabilitation (2).
Finance in healthcare is an ongoing global concern, in North America ‘Interest in enhanced recovery has increased in a climate where healthcare providers are keen to implement programmes to improve productivity and meet cost saving targets’ (3). The National Health Service in England (NHS) has faced increasing austerity since 2010 (4), with this likely to continue into the foreseeable future, therefore initiatives to improve patient care at a reduced cost are sought throughout the UK.
ERAS is now widely accepted as the gold standard approach to many elective colorectal surgical pathways within the UK (2), and has successfully been rolled out into areas such as urology and upper GI surgery. Latterly, many areas of elective orthopaedic joint replacements now follow the ERAS approach with elective spinal surgery slowly following suit in some places (3,5).
HES data in the UK 2010/11 shows 8,935 patients admitted with a primary diagnosis suggesting adult spinal deformity. Of these, 725 had open spinal surgery with 421 having instrumented spinal deformity correction. This complex spinal deformity surgery in adults involves a large cost to the provider (6), justified by a significant improvement in patients’ quality of life (7). Little has been published showing the ERAS process and outcomes of implementation within complex spinal surgery. This paper aims to discuss the implementation of such a service and impact on the three principles of ERAS.
ERAS has previously been successfully implemented for the management of patients undergoing adolescent scoliosis correction (8,9), this has not previously been looked at in degenerative spinal deformity patients.
Methods
The aim of this paper is to establish if ERAS can be utilised within complex spinal deformity surgery.
An ERAS service was developed within the orthopaedic spinal service of a tertiary spinal surgical centre in the UK in 2012, following the guidelines from the Department of Health (2). A working group from various professional backgrounds planned the implementation and scope of the service, with a decision to limit the service to patients undergoing elective surgery for adult deformity correction with a posterior instrumented fusion of greater than one level of fusion. The group developed a clear surgical pathway with engagement from all stakeholders prior to implementation, allowing all involved in the patient’s journey to be clear on the daily expectations within the peri- and post-operative in patient periods. Procedure specific updated patient information leaflets were developed in accordance with the national guidelines (10).
The implementation involved changes at various aspects of the patient’s pathway.
Pre-operative
Once the decision to consider complex spinal surgery has been made, rather than the traditional aspect of a waiting list the paradigm is shifted to create a productive waiting time; with the team working to ensure the patients are in the best possible condition to undergo complex spinal surgery. This productive waiting time includes is depicted in Figure 1.
The opportunity for the patient to meet not only the operating surgeons but the multi-disciplinary team that will be involved in their care along with patients who have previously undergone complex spinal surgery is facilitated. Education is provided at each stage and supported with written documents and a dedicated helpline. Therapy prehabilitation to build up muscle activity and promote the importance of physical activity along with equipment provision to improve independence where required. Vitamin D is checked and optimised where indicated as a master regulator of skeletal function and healing; this is done due to high levels of vitamin D deficiency in the UK [34% of the adult population in the winter (11)]. Visits to the ward and critical care can be facilitated to reduce anxiety on arrival. Smoking cessation can be planned and actioned if required.
Pre-operative planning includes not only an MDT discussion involving the surgical team but also a comprehensive anaesthetic assessment where moulds are made if required to optimise surgical positioning and reduce the risk of pressure area breakdown due to a lengthy surgical procedure. The surgeon ultimately discusses the treatment options; making a joint decision that surgery is an appropriate pathway.
Peri-operative
Patients are loaded with carbohydrate to reduce the bodily strain associated with a long anaesthetic. A prescribing pharmacist performs medicines reconciliation in the surgical admissions lounge to ensure no medications are omitted, along with a comprehensive analgesia regime to allow early mobilisation.
The pathway facilitates the routine use of intraoperative lignocaine infusions for analgesia and facilitating early mobilisation along with routine use of pre-incision ketamine boluses and post op ketamine infusions. The use of these medications intra operatively avoids the use of anaesthetic agents with long recovery/half-life and therefore allows early mobilisation post operatively.
The ERAS pathway allows multimodal post op analgesia regimes with PCA opioids/ketamine and IV paracetamol.
Immediate post-operative stage
A care pathway was designed involving all the professional disciplines responsible for the patients care with daily goals and expectations, including but not limited to: drain removal, thromboprophylaxis, wound care, bowel regime, analgesia expectations and mobilisation. Any deviations from the expected pathway require documented justification and are highlighted to the consultant spinal surgeon.
All involved in the patients’ care including the patient are fully aware of the goals and expectations at each step of the recovery period both in high dependency and on the ward, with timely discharge a clear focus for all.
Discharge
Patients have a dedicated support line provided by the ERAS team; they all receive a call at day one and three post discharge and then clinic review at 6 days. They are currently followed up by the surgeon, although the future will involve a multi-disciplinary follow up for these patients.
Data was gathered using hospital coding for length of stay (LOS) and readmissions. The Eurospine outcome measures international registry Spine TANGO was used to collect patient reported outcome measures and an anonymous survey monkey with 10 simple questions was designed and sent to all staff involved in the patients journey (surgeons, anaesthetists, nurses, therapists) 26 surveys were completed.
Analysis
Demographics and pre-operative patients’ characteristics were compared between pre-ERAS and post-ERAS groups using Fisher’s exact test for categorical variables and Wilcoxon rank test for non-normally distributed variables.
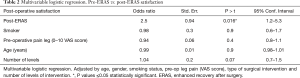
Multivariable logistic regression of patient’s Satisfaction pre/post-ERAS was performed to determine whether the introduction of ERAS is the responsible for the improvement of satisfaction rates. The model was adjusted by age, gender, smoking status, pre-op leg pain (VAS score), type of surgical intervention and number of levels of intervention.
Results
Since the implementation of the ERAS pathway in this institution 214 patients have been managed using the pathway, each having a fixation of one or more levels of the spine; often including a correction of deformity. The results have been collated over a 2-year period and compared to the 3 years prior to the implementation of the ERAS service.
The patient demographics of each group were statistically comparative and are summarised in Table 1. There were more female patients in both groups, the ages ranged from 16 to 83 with the mean age slightly younger in the pre ERAS group. The American Society of Anaesthesiologists (ASA) classification of physical status pre operatively was comparable between the groups, with similar numbers of smokers; although smoking cessation was strongly encouraged and support offered for this prior to listing for surgery. The patient reported pain and functional levels [measured using the core outcome measures index (COMI-back) score] were also similar between groups. The number of levels fused during the operation was similar between groups, most had either a posterior lumbar interbody fusion (PLIF) or a scoliosis correction (both adolescent and degenerative).

Full table
Vitamin D is now much improved when measured pre operatively, with 100% patients having optimum vitamin D at the time they undergo surgery, in comparison to previous levels which were inconsistent.
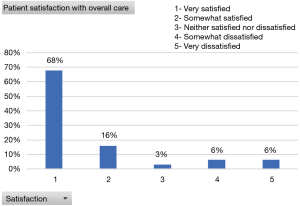
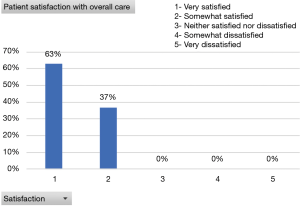
Patient satisfaction
Patient satisfaction, measured using the Core Outcome Measures Index (COMI-back) score which has been validated for use in spinal degenerative surgery (12). The data is collected and anonymised via spine TANGO, COMI-back has shown an improvement since the implementation of the ERAS service, with 100% of patients post ERAS satisfied post-operatively compared to 84% prior to the service (Figures 2,3). The small proportion of dissatisfied patients is no longer present (Figure 3).
After multivariable logistic regression we found that ERAS was independently associated with the improvement in patient satisfaction (OR: 2.5, P=0.016) (Table 2).
Full table
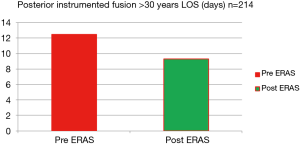
LOS
LOS has improved, specifically in the degenerative scoliosis population; with the average LOS for the 56 multi-level degenerative scoliosis correction patients reduced from 11 to 8 days. This is hypothesised to be due to the strict adherence to the pathway and access to the ERAS team for reassurance for the patient, their family and also the nursing staff caring for the patient. The patients undergoing complex fixation with or without bone grafting have also seen a reduction in the LOS from 7 to 5.2 days (Figure 4).
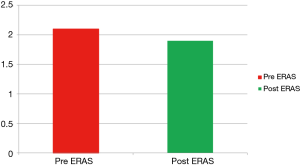
Readmissions
There is a concern when LOS is reduced that patients may experience complications requiring readmission to hospital. The readmission rate within 30 days, shown as a percent of total admissions, were therefore reviewed to ensure this was not the case as this would be counter intuitive to early discharge. The 30-day readmissions have actually reduced from 2.1% to 1.9% (Figure 5). Although this is not a statistically significant reduction, they have reduced despite a reduction in the LOS.
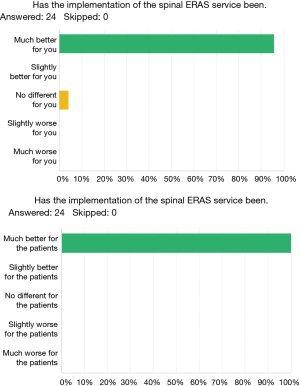
An anonymous survey (survey monkey) of staff satisfaction revealed high levels of satisfaction across the service from spinal surgeons to health care assistants on the ward (Figure 6). All staff feel the service is better for the patients and only one member of staff felt the service had no impact on them personally, highlighting the role the ERAS team play across the multi-disciplinary team.
With many positive comments shared by the team, when asked for examples of how the ERAS service has impacted (supplementary). The staff feel that the ERAS process has provided a positive impact on the team and the patients’ journey. The trust friends and family test has also received positive comments from patients following their experience of the ERAS service (Figure S1).
Discussion
The general population worldwide is undoubtedly ageing and therefore requiring increased access to healthcare to remain as active as possible (13-15). For the small number of people in this population with spinal deformity this can cause a significant impact on their daily life and ability to remain in good health. Complex spinal surgery is an option for these patients and available in the UK only at specialised centres commissioned to perform such procedures (7).
ERAS is well established in many areas of surgery (16), so much so there is a world ERAS society and associated congress. NHS England defines the process as the gold standard of care in the UK for elective surgery (2). It has been shown to be an effective way of managing patients undergoing the less complex spinal procedures within the USA (5,17,18). The ERAS pathway is a shift in overall focus from initial listing with the involvement of all members of the MDT to focus on the patient and has shown favourable results in other areas of elective surgery (16); this change in focus and optimisation for surgery is especially important in the elderly population (15). Hospital beds in the UK are finite; patients requiring prolonged stay under the care of surgical specialities may result in the cancellation of surgical procedures for other patients. Such cancellations also cause a significant cost to the organisation (4) along with distress for the patient awaiting the elective procedure. Initiatives to reduce the LOS whilst maintaining high standards of patient care are actively encouraged both locally and nationally (19). The current study showed that the ERAS service has resulted in a reduction in LOS for all patient groups undergoing complex spinal surgery over a 2-year period.
When a patient is undergoing complex spinal surgery it is important the patient experiences the best possible care throughout their journey, to ensure full engagement in their overall care as rehabilitation is vital to the success of the majority of Orthopaedic procedures. The present study suggests not only are the surgical outcome favourable, also the patient’s satisfaction of their overall care is also extremely favourable; all patients reporting being satisfied or extremely satisfied with their care. Previous studies looking at ERAS within spinal surgery have reviewed only the LOS without considering of the impact on the patient (10,17).
The development of a robust pathway is vital to allow all members of the team including the patient to understand the expectations on each day following admission. Early mobilisation has been shown to reduce complications in the elderly population undergoing spinal surgery (7). The present study did not compare complications with the group prior to ERAS but certainly the earlier mobilisation would appear to have impacted on LOS and the rate of reported complications has not increased.
The cost of such a service requires goodwill from all personnel in the first instance to agree the parameters required throughout the overall patient experience (2). There is then a financial requirement form the institution to release staff to become part of the ERAS team. These savings will be offset when the reduced length of patient stay is realised and more operations can be performed, clearly a clinically important parameter.
- Spinal bed £300 per night;
- ERAS nurse £36,428.4 PA;
- Assistant Practitioner £25,262 PA;
- Total bed days saved =508.6 days = £152,580;
- £121,735 saving.
Complex adult spinal deformity surgery is a complex procedure and therefore carries a high tariff from NHS England; this is justified by a huge impact on the quality of life for this group of patients which could cause a reduction in their financial burden in other areas of society. Lee et al. presented their LOS for this group of patients as 13 days (20); however there is little published data comparing the LOS for this group of patients as surgery varies considerably depending on the needs of the individual patient. A reduction in LOS for this group from 12.5 to 9.3 days does reduce the cost to the organisation for patients undergoing this procedure and has improved overall patient satisfaction.
ERAS has previously been successfully implemented for the management of patients undergoing adolescent scoliosis correction (8,9), the current study found equally favourable results in the older cohort of patients undergoing correction of degenerative deformity.
Conclusions
Despite the well-established benefits of ERAS programs as effective and economically viable, challenges arise when introducing ERAS pathways into routine practice. Barriers to implementation may be attributed to patient-related, staff-related and practice-related factors.
ERAS is a process that commences in the preoperative phase that ensures optimisation before surgery, continues into the intraoperative/perioperative phase followed by discharge planning and post-discharge phase.
We have successfully implemented an ERAS service within the context of corrective surgery for degenerative scoliosis. In this study ERAS results in improved patient and staff satisfaction with a significant reduction in LOS and therefore an overall cost saving to the organisation when used within a tertiary centre for complex spinal surgery.
Do you have any specific examples of how the enhanced recovery after surgery (ERAS) service has improved patient care?
Patient with complex biopsychosocial factors was managed better in their expectations.
Patients are better optimised. I can triage patients more effectively depending on the urgency of the surgery. Discussion about risks and morbidity is more meaningful.
My patients for the lumbar fusion are better informed and know exactly what to expect from the surgery and understand their role in getting better.
Very clear and consistent service provision.
Patients have contact details for the nurse and she is easy to contact.
Encourages patients to engage and participate in their care, seamless, timely and positive hospital journey.
Joint assessments with ERAS are beneficial for patients and therapists.
Offering opportunities for patients to talk to previously operated patients.
This service empowers patients to help themselves through an enhanced recovery care pathway which is key to achieving optimal recovery in the shortest possible time.
Our ERAS nurse reviews patients in regular basis ensuring issues are identified at an early stage and addressed appropriately. Few examples such as: close wound monitoring preventing delay in healing process, coordinating post op rehabilitation and safe discharge planning.
Patients form a trusting relationship with the eras nurse. They know exactly what is happening and going to happen throughout their patient stay.
Having one nurse who both supports the patient and the ward staff assisting the patient with their daily goals.
Seeing a familiar face throughout a daunting experience is always a good thing.
The ERAS role has improved patient experience as she is a go to port of contact for any questions and concerns the patients have. The ERAS nurse ensures the patients are receiving the specific to their needs, she also encourages the patient journey to be more time specific and meets aimed discharge dates by encouraging mobility, working with physio and removing lines in a timely manner or reminding staff when lines need to be removed.
Patient feedback is better.
Patients are able to mobilise sooner and have devices removed sooner.
No.
Patients appear to have more confidence in the process of surgery and recovery.
Excellent feedback from patients, close monitoring of their perioperative.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: NHS Rec approval not required for this service evaluation. Written consent gained from all patients to use collected data.
References
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [Crossref] [PubMed]
- Enhanced Recovery Partnership Programme. 2010. Delivering enhanced recovery; Helping patients to get better sooner after surgery. Available online: www.dh.gov.uk/publications
- Wainwright TW, Immins T, Middleton RG. Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best Pract Res Clin Anaesthesiol 2016;30:91-102. [Crossref] [PubMed]
- Robertson R, Wenzel L, Thompson J, et al. Understanding NHS financial pressures: how are they affecting patient care? The Kings Fund, London, UK, 2017.
- Ali ZS, Ma TS, Ozturk AK. Pre-optimisation of spinal surgery patients: Development of a neurosurgery Enhanced recovery after surgery (ERAS) protocol. Clin Neurol Neurosurg 2018;164:142-53. [Crossref] [PubMed]
- Yeramaneni S, Ames CP, Bess S. Center variation in episode-of-care costs for adult spinal deformity surgery: results from a prospective, multicenter database. Spine J 2018;18:1829-36. [Crossref] [PubMed]
- Adogwa O, Elsamadicy AA, Fialkoff J, et al. Early Ambulation Decreases Length of Hospital Stay, Perioperative Complications and Improves Functional Outcomes in Elderly Patients Undergoing Surgery for Correction of Adult Degenerative Scoliosis. Spine 2017;42:1420-5. [Crossref] [PubMed]
- Gornitzky AL, Flynn JM, Muhly WT. Case Series: A rapid recovery pathway for adolescent idiopathic scoliosis that improves pain control and reduces time to inpatient recovery after posterior spinal fusion. Spine Deform 2016;4:288-95. [Crossref] [PubMed]
- Muhly WT, Sankar WN, Ryan K. Rapid recovery pathways after spinal fusion for idiopathic scoliosis. Paediatrics 2016;137(4).
- National Institute for Clinical Excellence. Patient experience in adult NHS services: improving the experience of care for people using adult NHS services CG 138. Feb 2012, London, UK, 2012.
- Scientific Advisory Committee on Nutrition. 2016. Vitamin D and Health. London, UK. Available online: https://www.gov.uk/government/groups/scientific-advisory-committee-on-nutrition
- Mannion AF, Vila-Casademunt A, Domingo-Sàbat M, et al. The Core Outcome Measures Index (COMI) is a responsive instrument for assessing the outcome of treatment for adult spinal deformity. Eur Spine J 2016;25:2638-48. [Crossref] [PubMed]
- He W, Goodkind D, Kowal P. An Aging World: International Population reports. United States Census Bureau, Washington, USA, 2016.
- Fit for Frailty, Consensus best practice guidance for the care of older people living with frailty in community and outpatient settings. BGS 2014. Available online: http://ageing.oxfordjournals.org/content/35/5/526.full
- Harari D, Hopper A, Dhesi J, et al. Proactive care of older people undergoing surgery ('POPS'): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing 2007;36:190-6. [Crossref] [PubMed]
- Bagnall NM, Malietzis G, Kennedy RH, et al. A systematic review of enhanced recovery care after colorectal surgery in elderly patients. Colorectal Dis 2014;16:947-56. [Crossref] [PubMed]
- Wang MY, Chang PY, Grossman J. Development of an Enhanced Recovery After Surgery (ERAS) approach for lumbar spinal fusion. J Neurosurg Spine 2017;26:411-8. [Crossref] [PubMed]
- Blackburn J, Madhaven P, Leung YL. An enhanced recovery programme for elective spinal surgery patients. JCOM 2016;23.
- Wainwright TW, Wang MY, Middleton RG. Enhanced Recovery after Surgery (ERAS) – Concepts, components and application. Semin Spine Surg 2018;30:104-10. [Crossref]
- Lee R, Mokawem L. Anterior Column Reconstruction in Primary Adult Degenerative Scoliosis Correction Surgery: Restoring Lordosis and Achieving Indirect Decompression with Minimally Invasive Lateral Cages. Spine J 2017;17. [Crossref] [PubMed]