
Traumatic spinal cord injuries in geriatric population: etiology, management, and complications
Introduction
The geriatric population (≥65 years old) represents the fastest growing demographic in the United States (U.S.) (1). It is estimated that one-fifth of the total U.S. population will be 65 years old or older by 2050. People aged 85 and older will constitute 4% of the population by 2050, which is ten-times its percentage in 1950 (2). The aging of the general population corresponds to increased occurrence of injuries due to age-related decline in musculoskeletal function, neurological function, and bone flexibility. The incidence of spinal cord injury (SCI) is also increasing and in part due to this aging population (3). In 2016, the number of people in the U.S. with SCI was estimated at approximately 288,000 (4).
Mechanisms for SCI may be traumatic or non-traumatic. Non-traumatic causes include epidural abscesses, epidural hematomas, metastatic disease with epidural spinal cord compression, intradural tumors, and surgical complications (3,5). However, within the context of a growing geriatric population, the rising number of falls has led to an increase in median age of patients with initial traumatic SCI and remains the leading cause of SCI in patients over 65 years of age (6). Other leading causes of trauma-related SCI include motor vehicle accidents (MVA) and sports and recreation accidents (7).
Surgical treatment of traumatic SCI is typically performed in the form of decompression followed by stabilization with instrumentation (8). However, the presence of comorbidities that may lead to intraoperative mortality of SCI patients can result in the decision to pursue nonoperative management (9). Treatment with corticosteroids for patients with mild central cord syndrome is common and pharmacological agents, such as riluzole and minocycline, have shown promising results in reducing motor neuron loss and improving SCI recovery in clinical trials (10,11). Overall, the risk-benefit analysis of surgical intervention is further heightened in elderly patients, who often have significant comorbidities (9). The decision to pursue surgical or nonsurgical management of SCI remains difficult and requires further characterization of SCI, particularly in the geriatric population.
Despite pharmacological and surgical treatment along with SCI focused rehabilitation, secondary medical complications continue to be common in SCI patients (5,12). Acute and chronic secondary complications include respiratory, cardiovascular, and neurological problems that worsen the mortality and morbidity associated with SCI. These complications include respiratory failure, wound complications, urinary tract infections, and neurogenic shock (5). Intraoperative and postoperative complications have previously been categorized as major and minor by Glassman and colleagues based on consensus agreement of study group surgeons (13). These complications can lead to longer hospital stay, decreased functional recovery at long-term follow-up, and increased rate of mortality (14).
With the increased incidence of geriatric SCI and the management challenges associated with it, there is a need for further evaluation of this patient population. Our objective is to elucidate the demographics, diagnoses, mechanisms of injury, ASIA grade, management, complications, and mortality of traumatic SCI in geriatric patients, with specific examination of four age groups.
Methods
This study was a retrospective evaluation of prospectively collected data. Institutional Review Board approval was obtained (RSRB00062665). Patients 65 years of age and older, with complete medical records, and undergoing surgical or nonsurgical treatment for traumatic SCI at a level 1 trauma center from January 2003 to December 2013 were identified and enrolled. Over the study period, multiple surgeons from a single tertiary care academic center, as well as multiple providers from the inpatient rehabilitation facility located within the academic center, managed the patients. The orthopedic spine surgery service managed the majority of these patients. The main spinal trauma protocol in our center is urgent decompression (within 24 hours) in the setting of an unstable spine or neurological deficit. Over the study period the use of high dose steroids decreased. Most patients are admitted for neurological monitoring and in the setting of neurological deficits, the mean arterial pressure is elevated to >85 mmHg for up to 5 days post-operative. Criteria for surgery were unstable spine as determined on advanced imaging (magnetic resonance imaging or computed tomography). The presence of an epidural process causing compression to the neural elements and associated neurological deficits was also criteria for surgery. All patients enrolled had traumatic spinal cord injuries of the cervical, thoracic, and/or lumbar spine. Patients under 65 years of age, patients 65 years of age and older with incomplete medical records, and individuals identified by the study team as “non-traumatic SCI patients” were excluded from the study.
Patient demographics including age, sex, race, and ethnicity were identified. Clinical characteristics collected were: mortality, management (surgical versus nonsurgical), mechanism of injury, diagnoses, American Spinal Injury Association (ASIA) grade, and complications during acute hospitalization (major or minor based on an article published by Glassman and colleagues in 2007) (13). Diagnoses were sorted into: spine tumors and metastatic disease, fractures, central cord syndrome, disc herniation, cauda equina syndrome, epidural hematoma, unspecified myelopathy, or multiple diagnoses. Using demographic data, patients were separated into four groups based on age (65–69, 70–74, 75–79, and ≥80 years) to create four groups that are roughly equal in number (13, 16, 12, and 12, respectively). Diagnoses, ASIA grade, complications during acute hospitalization, and management were evaluated for each age group.
Statistical analysis
The Chi-square test, Fisher’s exact test, and logistic regression were used to determine significance, set at P<0.05.
Results
Demographics
Seven hundred and fifty-seven SCI patients were identified and 53 met our inclusion criteria, with 35 (66.0%) males and 18 (34.0%) females (Table 1). The average age was 74 years (range, 65 to 91 years). Thirteen (24.5%) patients were 65–69 years of age, 16 (30.2%) were 70–74, 12 (22.6%) were 75–79, and 12 (22.6%) were 80 or older. Forty-six (86.8%) patients were Caucasian, 4 (7.5%) were African American, 1 (1.9%) was Asian, and 2 (3.8%) did not state their race. Two (3.8%) patients were Hispanic or Latino, 31 (58.5%) were not Hispanic or Latino, and 20 (37.7%) did not state their ethnicity. As of September 2015, 17 (32.1%) patients were alive and 17 (32.1%) were deceased, with 14 (26.4%) deceased within 7 years after discharge and 20 (37.7%) alive after 7 years.
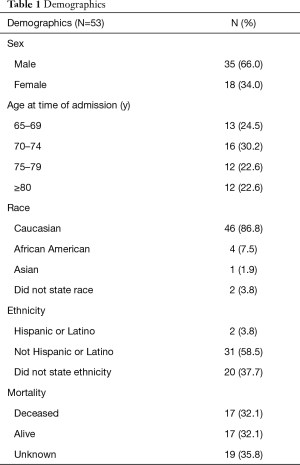
Full table
Diagnoses, mechanism of injury, and ASIA grade
Fracture (43.4%) was the most common diagnosis, followed by central cord syndrome (28.3%), multiple diagnoses (11.3%), and disc herniation (7.5%) (Table 2). One (1.9%) patient had cauda equina syndrome, 1 (1.9%) had an epidural hematoma, 2 (3.8%) had underlying spinal tumors, and 1 (1.9%) had an unspecified myelopathy. Traumatic SCI was most commonly the result of falls (36, 67.9%) and MVAs (9, 17.0%) (Table 3). Eight (15.1%) patients experienced traumatic SCI as a result of other trauma, such as being struck by an object. For all patients, ASIA grades were as follows: A 5 (9.4%), B 3 (5.7%), C 5 (9.4%), D 40 (75.5%) (Table 3). Fractures accounted for all 5 patients with ASIA A, as well as all 3 patients with ASIA B. Higher ASIA grades (ASIA A and ASIA B) had a significant association with fractures compared to lower ASIA grades (ASIA C and ASIA D) (P<0.001). Out of the 5 patients with ASIA C, 3 had central cord syndrome and 2 had fractures. Out of the 40 patients with ASIA D, 2 had spinal mass, 1 had unspecified myelopathy, 13 had central cord syndrome, 1 had epidural hematoma, 4 had disc herniation, 1 had cauda equina syndrome, 13 had fractures, and 5 had multiple diagnoses.
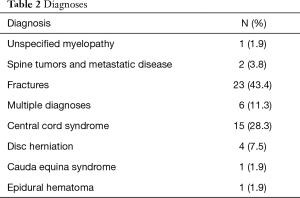
Full table
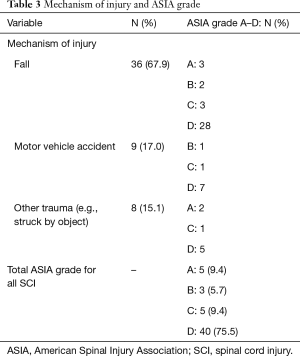
Full table
Inpatient hospital complications
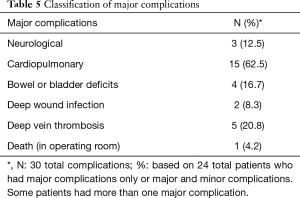
Thirty-four (64.2%) traumatic SCI patients experienced at least one complication during the acute hospitalization period (Table 4). Five (9.4%) patients sustained only major complications, 10 (18.9%) sustained only minor complications, and 19 (35.8%) had both major and minor complications (defined by Glassman et al.’s criteria) (13). Among the 24 total patients who sustained major complications, 30 total counts of complications were reported (Table 5). Cardiopulmonary complications (15, 62.5%) were the most common out of the major complications. Five (20.8%) patients had deep vein thrombosis, 4 (16.7%) experienced bowel or bladder deficits, and neurological complications occurred in 3 (12.5%) patients. Deep wound infections (2, 8.3%) and death (1, 4.2%) were the other two major complications that were noted in these patients.
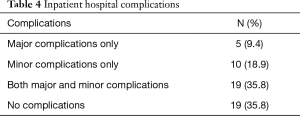
Full table
Full table
Diagnoses, management, ASIA grade, and inpatient complications by age group
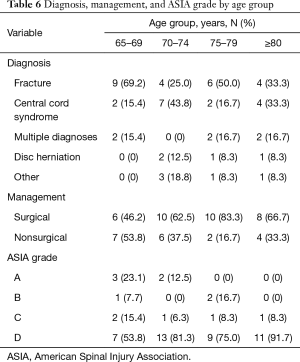
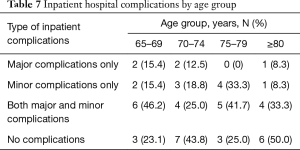
Diagnoses, management, ASIA grade, and complications varied across the four geriatric age groups. The 65–69 age group had the highest rate of fractures (69.2%), with the next highest rate being 50% in the 75–79 age group. Central cord syndrome was the most common diagnosis in the 70–74 age group (43.8% compared to 33.3% in the next highest group, ≥80 years) (Table 6). Management with surgery was increasingly utilized with age across the first three age groups—46.2% of patients aged 65–69 underwent operative management, 62.5% of those 70–74, and 83.3% of those 75–79. The rate of surgical management decreased back down to 66.7% in the ≥80 group. ASIA A grade was more common in the younger two groups (n=5) and decreased with age (n=0 in the two older groups, P=0.004). The youngest age group had the highest rate of major complications (15.4%) as well as the highest rate of major and minor complications (46.2%), while patients aged 75–79 had the highest rate of minor complications (33.3%) (Table 7). Patients ≥80 years had the lowest overall rate of complications (50%).
Full table
Full table
Discussion
Spinal cord injuries commonly occur due to traumatic events. Geriatric patients are more vulnerable to traumatic SCI than the general patient population due to various age-related factors. These factors include susceptibility for fall-related injuries due to decreased neurological reserve, increased prevalence of cervical spinal stenosis with underlying myelopathy, and decline in bone mineral density (3). A recent study of an SCI database from a single institution reported that the number of SCI-related hospital admissions of geriatric patients increased fivefold from 1980 to 2005 (compared to a 60% increase in the general population during that period). Considering that the incidence of traumatic SCI in the elderly is increasing, the aging of the general (U.S.) population will greatly influence the future of spine trauma and spine rehabilitation centers (3,15).
In this study, 53 geriatric patients were identified, with an average age of 74 years. Sixty-six percent of traumatic SCI patients were male. A total of 26.4% were deceased within seven years after discharge, and more than half of all patients (64.2%) underwent surgical management. Well over one-third of patients (43.4%) were diagnosed with fracture. The next most common diagnoses were central cord syndrome (28.3%), multiple diagnoses (11.3%) and disc herniation (7.5%). Fall was by far the most common mechanism of injury, causing 67.9% of all traumatic SCI. About two-thirds of patients experienced at least one type of complication during the acute hospitalization period (64.2%). Most of these patients experienced both major and minor complications (35.8%). The four geriatric age groups were each represented by approximately one-fourth of the SCI patients.
Examination of the diagnoses, management, ASIA grade, and complications of patients within the four geriatric age groups yielded important information regarding geriatric SCI care. While diagnoses did not significantly change with age, surgical management increased with age within the first three age groups but decreased in the ≥80 age group (46.2%, 62.5%, 83.3%, and 66.7%, respectively). Most notably, ASIA A grade was only associated with the two youngest age groups, while no patients greater than 74 years of age had an SCI grade of ASIA A. In addition, fractures accounted for all 8 patients with ASIA A or ASIA B SCI.
Literature has shown that the proportion of SCI patients ≥65 years of age is rising rapidly and may be greater than previously expected (16,17). This is probably due to the aging of the U.S. population and increased frequency for older patients to sustain injury from relatively minor falls. Previous studies have noted that falls are the predominant mechanism of SCI in patients older than 45 years. Geriatric patients are particularly at greater risk for SCI secondary to falls due to inherent age-related decline in musculoskeletal functioning and degeneration of the spine (9). Our study revealed that 67.9% of geriatric traumatic SCI was caused by falls, which is in line with other studies, some of which have reported falls accounting for as much as 77% of cases (15). These falls may give rise to fractures and central cord syndrome, which were the two most prevalent diagnoses in our study.
Our data showed that the most severe SCI (ASIA A and ASIA B) occurred almost exclusively in the geriatric patients aged 65–74. This may be due to riskier behavior in the younger geriatric patients—for example, half of the youngest geriatric age group experienced traumatic SCI due to falls from height (e.g., off a ladder) or secondary to risky behaviors (e.g., snowmobiling, horse riding), both of which were not present in any patient ≥80 years. Other studies have shown that increasing age is associated with a decrease in the mean fall height (18). As such, although there is an increased risk of SCI that comes with age, there may not be an increased severity of injury.
Surgical management of traumatic SCI increased with age, up to a certain point. The 65–69 age group had the lowest rate of nonoperative care (46.2%), which may be due to the perceived risk of complications among older patients and ambiguity about optimal treatment for SCI, causing surgeons to deliberate for years before making a clear therapeutic decision. While the 75–79 age group had the highest rate of operative management (83.3%), only 66.7% of patients ≥80 underwent surgery. Like the 65–69 age group, the ≥80 group may experience decreased surgical management due to perceived risk of complications (17,19,20). However, the age of 80 may represent a time period during which the potential benefits of surgical intervention are opposed by the risk of perioperative or postoperative complications, ultimately preventing any operative care for the remainder of the patient’s life. In fact, Graffeo and colleagues performed a single-center retrospective review of operative and nonoperative management of cervical fractures within octogenarians from 1998 to 2014, noting no significant difference in survival advantage or mean time to death for either management strategy (21).
Life expectancies of SCI patients are still below those of people without SCI, although the gap is shortening (22). In our study, 37.7% of patients survived at least seven years post discharge. This is greater than DeVivo et al.’s study, which reported a 7-year survival rate in patients older than 50 years of 22.7% (compared to 86.7% in the general population) (23). A significant difference in SCI mortality rate between geriatric and younger patients has been reported in previous studies (3,24,25). This is most likely due to inpatient complications, such as respiratory distress. For example, Harrop et al. determined that patients 45 years and older with ASIA A injuries were more likely to require tracheostomy than younger patients. These differences in tracheostomy requirement were believed to be due to decreased muscular protection of the airway, vital capacity, and reserve volumes (26). Furthermore, this association of complications and severe ASIA grade was also evident in the 65–69 age group, which had the highest rate of ASIA A SCI and both major and minor complications. The use of halo immobilization in the nonoperative treatment of spinal fractures has also been associated with increased in-hospital mortality rates in patients older than 65 years (27,28). Similarly, the 65–69 age group, which had the highest rate of nonoperative care, also had the highest rate of major (life-threatening) complications.
Existing literature has identified a growing need to further evaluate geriatric SCI given the country’s aging population. Therefore, this study evaluates the demographic and clinical characteristics of traumatic SCI within a geriatric population. The youngest geriatric patients experienced the highest proportion of ASIA A SCI and highest rate of major complications. The 75–79 age group utilized surgery in four-fifths of patients, which was considerably greater than the two adjacent age groups (which each utilized surgery in roughly two-thirds of patients). Surprisingly, patients in the oldest age group were most likely to complete SCI admission without a complication. Taken together, these results indicate that despite geriatric patients commonly being considered as one population group, the severity, management, and complications of SCI in elderly patients are more nuanced than previously thought.
There are a few limitations to this study. First, electronic medical records were not fully complete in some patients, and nearly 50 records were not updated regarding mortality information. Although steps were taken to obtain this information (i.e., reaching out to primary physicians, researching obituaries online), only a few results were salvaged this way. Second, there is a lack of diversity in demographics, as the vast majority of patients were Caucasian (86.8%), while only 7.5% of patients were African-American (the second-most common racial group in this study). According to one study, when accounting for all age groups, 22% of SCI in the U.S. occurs in African-Americans (29). Third, there were no patient reported outcomes (PRO) collected for the SCI patients. Since these patients were managed by multiple providers from various medical specialties, there were no standard PRO used among the care teams during the study period. Lastly, we did not evaluate each surgical intervention performed since the goal of this study was not to comment on surgical treatment, but rather on complications and mortality following SCI.
Conclusions
By evaluating and comparing traumatic SCI in the geriatric population at a level I trauma center, knowledge of etiology, management, and complications was ascertained. Fractures and central cord syndrome were the most common diagnoses, and typically due to falls. The complication rate in this population is high: 9.4% of patients had major complications, 18.9% had minor complications, and 35.8% had both major and minor complications. Younger age was associated with highest percentage of ASIA A SCI and increased rate of major complications. Orthopedic research concerning geriatric SCI patients should be of high priority due to the complexities of traumatic injury within this demographic and the increasing average age of the U.S. population.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was a retrospective evaluation of prospectively collected data. Institutional Review Board approval was obtained (RSRB00062665).
References
- Etzioni DA, Ko CY. The Aging Population and Its Impact on the Surgery Workforce. Ann Surg 2003;238:170-7. [Crossref] [PubMed]
- Congressional Budget Office. Rising Demand for Long-Term Services and Supports for Elderly People, 2013.
- Fassett DR, Harrop JS, Maltenfort M, et al. Mortality rates in geriatric patients with spinal cord injuries. J Neurosurg Spine 2007;7:277-81. [Crossref] [PubMed]
- Lee JS, Kim SW, Jee SH, et al. Factors Affecting Quality of Life Among Spinal Cord Injury Patients in Korea. Int Neurourol J 2016;20:316-20. [Crossref] [PubMed]
- Sekhon LHS, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976) 2001;26:S2-12. [Crossref] [PubMed]
- Etzioni DA, Liu JH, Maggard MA, et al. The aging population and its impact on the surgery workforce. Ann Surg 2003;238:170-7. [Crossref] [PubMed]
- Jackson AB, Dijkers M, DeVivo MJ, et al. A demographic profile of new traumatic spinal cord injuries: Change and stability over 30 years. Arch Phys Med Rehabil 2004;85:1740-8. [Crossref] [PubMed]
- Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the surgical timing in acute spinal cord injury study (STASCIS). PLoS One 2012;7:e32037. [Crossref] [PubMed]
- Jabbour P, Fehlings M, Vaccaro AR, et al. Traumatic spine injuries in the geriatric population. Neurosurg Focus 2008;25:E16. [Crossref] [PubMed]
- Brodell DW, Jain A, Elfar JC, et al. National trends in the management of central cord syndrome: an analysis of 16,134 patients. Spine J 2015;15:435-42. [Crossref] [PubMed]
- Ahuja CS, Martin AR, Fehlings M, et al. Recent advances in managing a spinal cord injury secondary to trauma. F1000Res 2016;5. [Crossref] [PubMed]
- Ikpeze TC, Mesfin A. Spinal Cord Injury in the Geriatric Population: Risk Factors, Treatment Options, and Long-Term Management. Geriatr Orthop Surg Rehabil 2017;8:115-8. [Crossref] [PubMed]
- Glassman SD, Hamill CL, Bridwell KH, et al. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007;32:2764-70. [Crossref] [PubMed]
- Wilson JR, Arnold PM, Singh A, et al. Clinical prediction model for acute inpatient complications after traumatic cervical spinal cord injury: a subanalysis from the Surgical Timing in Acute Spinal Cord Injury Study. J Neurosurg Spine 2012;17:46-51. [Crossref] [PubMed]
- Hagen EM, Aarli JA, Gronning M. The clinical significance of spinal cord injuries in patients older than 60 years of age. Acta Neurol Scand 2005;112:42-7. [Crossref] [PubMed]
- Chen Y, He Y, DeVivo MJ. Changing Demographics and Injury Profile of New Traumatic Spinal Cord Injuries in the United States, 1972-2014. Arch Phys Med Rehabil 2016;97:1610-9. [Crossref] [PubMed]
- Ge L, Arul K, Ikpeze T, et al. Traumatic and Nontraumatic Spinal Cord Injuries. World Neurosurg 2018;111:e142-8. [Crossref] [PubMed]
- Con J, Friese RS, Long DM, et al. Falls from ladders: age matters more than height. J Surg Res 2014;191:262-7. [Crossref] [PubMed]
- Faciszewski T, Winter RB, Lonstein JE, et al. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine (Phila Pa 1976) 1995;20:1592-9. [Crossref] [PubMed]
- McDonnell MF, Glassman SD, Dimar JR, et al. Perioperative complications of anterior procedures on the spine. J Bone Joint Surg Am 1996;78:839-47. [Crossref] [PubMed]
- Graffeo CS, Perry A, Puffer RC, et al. Deadly falls: operative versus nonoperative management of Type II odontoid process fracture in octogenarians. J Neurosurg Spine 2017;26:4-9. [Crossref] [PubMed]
- National Spinal Cord Injury Statistical Center. Spinal Cord Injury Facts and Figures at a Glance 2012. Available online: https://www.nscisc.uab.edu
- DeVivo MJ, Kartus PL, Stover SL, et al. Seven-year survival following spinal cord injury. Arch Neurol 1987;44:872-5. [Crossref] [PubMed]
- Jackson AP, Haak MH, Khan N, et al. Cervical Spine Injuries in the Elderly: Acute Postoperative Mortality. Spine (Phila Pa 1976) 2005;30:1524-7. [Crossref] [PubMed]
- Lieberman IH, Webb JK. Cervical spine injuries in the elderly. J Bone Joint Surg Br 1994;76:877-81. [Crossref] [PubMed]
- Harrop JS, Sharan AD, Scheid EH, et al. Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg 2004;100:20-3. [PubMed]
- Majercik S, Tashjian RZ, Biffl WL, et al. Halo vest immobilization in the elderly: a death sentence? J Trauma 2005;59:350-6; discussion 356-8. [Crossref] [PubMed]
- Tashjian RZ, Majercik S, Biffl WL, et al. Halo-Vest Immobilization Increases Early Morbidity and Mortality in Elderly Odontoid Fractures. J Trauma 2006;60:199-203. [Crossref] [PubMed]
- National Spinal Cord Injury Statistical Center. Spinal Cord Injury Facts and Figures at a Glance 2016. Available online: https://www.nscisc.uab.edu


