Vertebral height restoration following kyphoplasty
Introduction
More than 700,000 individuals experience vertebral compression fractures (VCFs) each year in the United States. (1,2) Worldwide, VCFs affect 30–50% of people over 50 years of age (3). Patients are typically elderly and fractures are painful. Pain may result in marked functional impairment. VCFs can result from advanced osteoporosis or less commonly, from metastases, osteolytic lesions or trauma. The presentation of patients with VCFs varies depending on the level(s) affected; however, patients often report discrete onset axial back pain after lifting or bending, uncommonly with radiation. Pain is typically positional, most often associated with lying supine and with any weight-bearing activities. In the elderly, this may often lead to quite limited activity, polypharmacy, social isolation, loss of independence and depression. Patients rarely have neurologic deficit and management consists primarily of rest, analgesic medications, and immobilization in an orthotic. Supplemental treatments including bisphosphonates, calcitonin, and parathyroid hormone have been shown to offer some benefit in pain control and function.
Surgery tends to be employed rarely and as a last resort in osteoporotic patients. Bone quality often precludes traditional surgical treatments such as limited bony decompression, dorsal internal fixation and fusion. Kyphoplasty is a minimally invasive treatment option for these patients and has been shown to reduce pain and improve function (4-8). Kyphoplasty involves transpedicular or extrapedicular insertion of an inflatable bone tamp into the compressed vertebral body (VB). The tamp is inflated to create a cavity for a subsequent low-pressure injection of bone cement providing potential for vertebral height restoration.
The goals of kyphoplasty are to reduce and stabilize the fracture, restore vertebral height, decrease kyphotic angulation, prevent the progression of kyphosis, and reduce or eliminate pain. Successful treatment leads to improved function and quality of life. Few have attempted to correlate restoration of VB height and clinical outcomes other than pain and activity levels. One study completed in 2014 found that kyphoplasty increased vertebral height and decreased both pain scores and opiate requirements while improving functional status in 67 patients (9). Lee et al. also demonstrated that in those with anterior vertebral compression ratios greater than 70%, kyphoplasty reduced pain, restored anterior vertebral height and maintained kyphotic angle (10). Feltes et al. in a study of thirteen patients undergoing kyphoplasty, reported a 90–100% reduction in pain without findings of VB height improvement (11). We sought to add to the limited literature examining the effects of vertebral height restoration and its correlation with validated clinical scales measuring pain, disability and quality of life in patients undergoing kyphoplasty.
Methods
Study design
Retrospective case series.
Patient selection
Following institutional review board approval, demographic, historical, imaging, and outcomes data were extracted retrospectively from the medical records of 59 patients at our tertiary care, academic referral center. Fifty-nine patients with one to three painful VCFs between T5 and L5 due to osteoporosis (n=40) or cancer (n=19) who underwent kyphoplasty using the KyphonTM Balloon Kyphoplasty System (Medtronic Spinal and Biologics, Memphis, TN, USA) between 12/1/2003 and 3/10/2011 were included in the analysis. Eighty-six vertebrae in these 59 patients were treated by two neurosurgeons. Non-consecutive patients are included, as measurable postoperative imaging was not available for all patients operated over the given time span. The diagnosis of a compression fracture was made by preoperative history and physical examination followed by radiographs, CT, MR and/or nuclear bone scan imaging studies. All patients had persistent, life-altering pain and were classified as failures to respond to at least four weeks of preoperative conservative management including rest, orthotic immobilization and support, and analgesic medications. The diagnosis of osteoporosis was made by dual axial absorptiometry (DXA, Hologic and GE Lunar) scanning and the diagnosis was made at variable times prior to surgery with many patients having had been diagnosed years prior. For some patients, the vertebral fracture is actually what led to the diagnosis of osteoporosis. Osteoporosis was defined as a value of bone mineral density (BMD) 2.5 standard deviations or more below the young adult mean (T score <−2.5). Osteopenia (decreased bone mass) was defined as a value of BMD of more than one standard deviation below the mean for a young adult, but less than 2.5 standard deviations below this value (T score −2.5).
Surgical technique
Kyphoplasty was performed under general anesthesia using simultaneous anterior-posterior and lateral biplanar fluoroscopic guidance. An 11-gauge working channel was passed into the affected vertebrae in transpedicular fashion in the lumbar spine or extrapedicular fashion in the thoracic spine. A precision drill was then advanced through the cannula to create a channel that extended to the junction of the anterior and middle third of the VB. The kyphoplasty balloon was then inserted and gradually inflated to create an intervertebral cavity. Under fluoroscopic guidance, semi-solid poly methyl-methacrylate (PMMA) bone void filler containing radiopaque contrast was injected under low pressure. AP and lateral fluoroscopic imaging was used throughout the procedure to ensure that bone void filler positioning was contained within the affected VB after removal of the cannulas.
Outcomes measurements
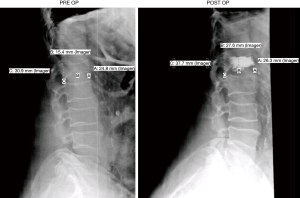
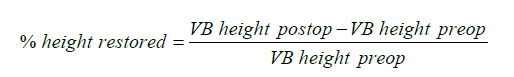
AP and lateral radiographs were taken pre-operatively and between two and six weeks post-operatively for each patient. Pre-and post-operative measurements of anterior, middle and posterior VB heights were made and compared independently by three investigators, two neurosurgery residents (JM, PGY 2 and JA, PGY 7) and one medical student (MS, MS3) using lateral radiographs on the Phillips iSite image viewer. The investigators underwent a single training session before beginning measurements to minimize inter-observer variability. Measurements randomly and independently audited by the two neurosurgeons (MRC and PRP). An example of one such set of measurements can be seen in Figure 1. Percent height restored was measured for the anterior, middle and posterior portions of each VB using the following formula.
Pain was measured prospectively using the Visual Analog Scale (VAS) [range: 0 (none) to 10 (worst)] before and after surgery. Pre-operative measurements were taken at the pre-operative evaluation within one week of surgery and postoperative evaluations were completed at two and six weeks after surgery and at subsequent specific catchment points: March 2007 and September 2012. Pre and post-operative disability and quality of life were retrospectively measured via patient surveys using the Roland Morris Disability Index (RMDI) [range: 0 (no disability) to 24 (high disability)] and EuroQol5-Domain instrument (EQ5D) [range: −0.11 (poor quality of life) to 1.0 (perfect health)], respectively. Pre and post-operative narcotic analgesic usage was recorded from medical records.
Statistical analysis
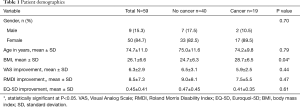
Demographic characteristics were summarized by descriptive statistics according to cancer status (Table 1). Age and BMI were presented as continuous variables with mean values and standard deviations. Differences in continuous variables were analyzed using independent t-tests. The categorical variable gender was reported as counts and frequencies with statistical comparisons performed using chi-square test. Improvement in outcomes scores (VAS score for pain, EQ-5D score to measure quality of life, and RMDI score for disability) was defined as the difference in the pre- and post-operative score. Pearson’s correlation coefficient, r, was used to determine possible correlations between anterior, middle and posterior VB height improvements and patient outcomes. Simple and multiple linear regressions were used to explore predictors of improvement in patient outcomes. Statistical significance was defined as P<0.05. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Full table
Results
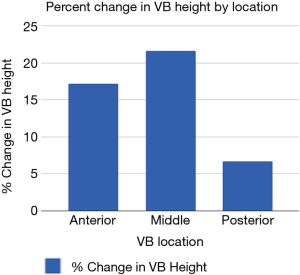
Of the 59 patients undergoing kyphoplasty for painful VCF’s, 19 had VCF’s resulting from cancer and 40 had VCF’s due to osteoporosis. Table 1 presents patient demographics. The mean patient age was 74.7±11.0 standard deviation (SD) and 84.7% of patients were female. The mean BMI was 26.1±6.6 SD. Most patients had reduced pain (n=58; 98.3%), reduced disability (n=55; 93.2%) and improved quality of life (n=55; 93.2%) with reduction/improvement defined as any positive change in each of the validated measurement instruments. The average improvement in VAS, RMDI and EQ-5D scores for all patients was 6.3, 8.5 and 0.45, respectively. These values were not significantly different between cancer and non-cancer patients. As shown in Figure 2, the average percent change in anterior, middle and posterior VB heights was 17.2, 21.7 and 6.7, respectively. No correlations or associations were found between anterior, middle or posterior VB height improvements and any of the patient outcomes (VAS, RMDI, EQ-5D). Pearson correlation coefficients ranged from 0.001–0.152, indicating little correlation between VB height improvements and outcomes measures (Table 2). Linear regression revealed limited evidence for age, gender, body mass index (BMI), or VB height change as predictors of clinical improvement, with R2 values ranging from 0.001–0.113. None of the results were statistically significant.

Full table
Of the 86 VBs treated, 63 (73.3%) had anterior height restoration, 66 (76.7%) showed middle height restoration and 57 (66.3%) demonstrated posterior height restoration after kyphoplasty. Forty-two of the VBs (48.8%) demonstrated an increase in all three measurements and 78 (90.7%) had an increase in at least one measurement (anterior, middle or posterior height). Thirty-eight patients (64.4%) reported pre-operative narcotic use and this decreased to 15 patients (25.4%) post-operatively.
Discussion
This retrospective review is one of the largest analyses to date using validated instruments to measure associations between vertebral height restoration and subsequent improvements in pain, quality of life and disability following kyphoplasty.
There are no well-established standards to quantify the percentage of vertebral height regained following kyphoplasty. Other investigators have quantified spinal deformity as percent restoration of VB height previously lost and percent VB height increase or degree of correction of the resultant angular deformity (12-14). Gaitanis et al. in an analysis of thirty-two consecutive patients with osteoporotic VCFs (27 patients, 49 VBs) or VB tumors (5 patients, 12 VBs) treated with kyphoplasty, utilized lateral radiographs to measure height loss and resultant improvement after kyphoplasty. These authors used anterior and mid-vertebral heights defined as the distance between the upper and lower end plates at the anterior VB wall and center of the VB respectively finding that anterior wall height was restored in 43/49 VBs (88%) and mid vertebral height was restored in 45/49 VBs (92%) in the osteoporotic VCF group (12). Lieberman et al. in a study of seventy consecutive kyphoplasty procedures in 30 patients with osteoporotic VCFs measured vertical height of fractured vertebrae before and after surgery with vertebral height defined as the distance (endplate to endplate) at the center of the VB on the lateral radiograph. They then calculated height regained as: post-treatment height minus pretreatment fractured height and height restored as: (height regained/height lost) ×100. The authors found that kyphoplasty restored 47% of the lost height in 70% of the vertebral bodies (14). The method of using three VB height measurements (anterior, middle and posterior) has also been reported previously in the literature (15). In this study, de Falco et al. examined sixty-one patients undergoing kyphoplasty for traumatic thoracolumbar fractures finding statistically significant improvement in all three VB height measurements post-treatment. Since vertebral height restoration can vary from anterior to posterior, the use of three vertebral height measurements improves the level of detail in quantification of VB height improvement. In the present study, the greatest improvement in VB height was seen at the middle of the VB, followed by the anterior and posterior locations. One explanation for this is that the greatest loss in VB height tends to occur in the middle of the VB and thus this area has the greatest potential for height restoration with kyphoplasty (Figure 1). Additionally, placement of the balloon tamp results in the greatest expansion in the middle of the VB.
In our patients, kyphoplasty restored some degree of radiographic vertebral deformity in all but 8 of the 86 (9.3%) treated vertebrae. Increases in height were observed by anterior, middle, and posterior VB measurements. An increase in at least one of these measurements was evident in 90.7% of VBs after kyphoplasty. These results are consistent with previous literature that has reported height restoration varying between 58–92% (12,16).
Complications from kyphoplasty such as cement leakage, pulmonary embolism, radiculopathies, rib fractures, subsequent vertebral fractures, and spinal cord or neural compression have been described in the literature (17-19). These were not encountered in our study patients. There were no procedure related infections, cardiac complications, or pneumothoraces.
No optimal degree of height restoration has been established for improved pain, function and quality of life. While no significant relationships between height restoration and outcomes were seen in our results, the VAS, RMDI and EQ-5D scores all improved from pre- to post-operatively indicating that kyphoplasty had a positive effect on pain, functionality and quality of life in this patient population. A larger study population may be needed to discover significant associations between height restoration and improvements in outcomes.
Study limitations
As can be seen in Figure 1, it is difficult to measure a 3-dimensional object such as a VB with 2-dimensional fluoroscopic imaging. The height of the VB may vary from medial to lateral and result in multiple superior and inferior VB edges. Subjectivity may compromise measurement accuracy. This was addressed by choosing a point between the two potential edges (seen in Figure 1 post-op image, top of line B). Cement leakage can obscure the superior and inferior edges of the VB, further complicating measurement. Additionally, although every effort was made to standardize the measurement process, inter-observer variability of measurements cannot be overlooked (3 independent measurers). Since this study was retrospective in nature, unobserved confounding variables might have affected the results. While the VAS was collected prospectively, the RMDI and EQ5D were collected retrospectively, introducing the possibility of recall bias. However, the rate of improvement in RMDI and EQ5D after kyphoplasty follows the same trend as the VAS results, which were collected prospectively. Furthermore, no patient had a worse score post-operatively in any of the three domains, supporting the strength of this trend. Despite the retrospective collection, the data accurately reflect patients’ improvement in quality of life and functional outcome following kyphoplasty. The possibility of placebo effect on outcomes following any treatment also cannot be excluded.
VCF etiologies included both cancer and osteoporosis, creating a heterogeneous group. However, improvements in outcomes were identical when evaluated as subgroups by etiology, supporting the efficacy of kyphoplasty across a wide range of pathologies. Results of the evaluations were analyzed by etiology subgroup, and found to be identical to the overall trend in improvement found in the group as a whole.
As this was a cross-sectional study, long term patient follow up (beyond six weeks) was completed at specific catchment points (March 2007 and September 2012) rather than at a standard time period post-procedure and a wide range of follow up was represented (17–1,472 days). While this may limit reproducibility, it enhances generalizability and demonstrates that the results found in kyphoplasty are rapidly effective and durable, confirming both immediate and sustained pain relief.
Future directions
Although a prospective randomized control trial examining outcomes after various levels of height restoration would be ideal to address these limitations, it would be difficult ethically to predetermine a cement volume or degree of height and angular restoration when the surgeon’s judgment may call for more tailored treatment. In order to more accurately quantify VB height restoration following kyphoplasty, CT volumetric analysis may be utilized. Volumetric analysis would eliminate the previously discussed difficulties in measuring height changes of the 3-dimensional VB. Additionally, since adjacent level compression fractures have been reported after kyphoplasty in the past, eliciting controversy regarding the cause, examination of a relationship between height restoration and adjacent level fracture rate is warranted. An examination of kyphotic angle reduction and its’ association with height restoration and patient outcomes may also be performed in the future.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All authors hereby declare that all experiments have been examined and approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All authors declare that written informed consent was obtained from the approved parties for publication of this manuscript and accompanying images.
References
- Felsenberg D, Silman AJ, Lunt M, et al. Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 2002;17:716-24. [Crossref] [PubMed]
- Riggs BL, Melton LJ 3rd. The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone 1995;17:505S-511S. [Crossref] [PubMed]
- Ballane G, Cauley JA, Luckey MM, et al. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 2017;28:1531-42. [Crossref] [PubMed]
- Eidt-Koch D, Greiner W. Quality of life results of balloon kyphoplasty versus non surgical management for osteoporotic vertebral fractures in Germany. Health Econ Rev 2011;1:7. [Crossref] [PubMed]
- Kicielinski KP, Pritchard PR, Ruiz H, et al. Patient Experience Following Kyphoplasty: Safety, Efficacy and Patient Satisfaction. Br J Med Med Res 2015;10:1-11. [Crossref]
- Papanastassiou ID, Phillips FM, Van Meirhaeghe J, et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J 2012;21:1826-43. [Crossref] [PubMed]
- Van Meirhaeghe J, Bastian L, Boonen S, et al. A randomized trial of balloon kyphoplasty and nonsurgical management for treating acute vertebral compression fractures: vertebral body kyphosis correction and surgical parameters. Spine (Phila Pa 1976) 2013;38:971-83. [Crossref] [PubMed]
- Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 2009;373:1016-24. [Crossref] [PubMed]
- Tolba R, Bolash RB, Shroll J, et al. Kyphoplasty increases vertebral height, decreases both pain score and opiate requirements while improving functional status. Pain Pract 2014;14:E91-7. [Crossref] [PubMed]
- Lee JH, Lee DO, Lee JH, et al. Comparison of radiological and clinical results of balloon kyphoplasty according to anterior height loss in the osteoporotic vertebral fracture. Spine J 2014;14:2281-9. [Crossref] [PubMed]
- Feltes C, Fountas KN, Machinis T, et al. Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus 2005;18:e5. [Crossref] [PubMed]
- Gaitanis IN, Hadjipavlou AG, Katonis PG, et al. Balloon kyphoplasty for the treatment of pathological vertebral compressive fractures. Eur Spine J 2005;14:250-60. [Crossref] [PubMed]
- Phillips FM, Ho E, Campbell-Hupp M, et al. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2003;28:2260-5; discussion 2265-7. [Crossref] [PubMed]
- Lieberman IH, Dudeney S, Reinhardt MK, et al. Initial outcome and efficacy of "kyphoplasty" in the treatment of painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2001;26:1631-8. [Crossref] [PubMed]
- de Falco R, Bocchetti A. Balloon kyphoplasty for pure traumatic thoracolumbar fractures: retrospective analysis of 61 cases focusing on restoration of vertebral height. Eur Spine J 2014;23 Suppl 6:664-70. [Crossref] [PubMed]
- Ates A, Gemalmaz HC, Deveci MA, et al. Comparison of effectiveness of kyphoplasty and vertebroplasty in patients with osteoporotic vertebra fractures. Acta Orthop Traumatol Turc 2016;50:619-22. [Crossref] [PubMed]
- Padovani B, Kasriel O, Brunner P, et al. Pulmonary embolism caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJNR Am J Neuroradiol 1999;20:375-7. [PubMed]
- Deramond H, Depriester C, Galibert P, et al. Percutaneous vertebroplasty with polymethylmethacrylate. Technique, indications, and results. Radiol Clin North Am 1998;36:533-46. [Crossref] [PubMed]
- Mika A, Unnithan VB, Mika P. Differences in thoracic kyphosis and in back muscle strength in women with bone loss due to osteoporosis. Spine (Phila Pa 1976) 2005;30:241-6. [Crossref] [PubMed]