
Minimally invasive lumbar decompression in an ambulatory surgery center
Introduction
In recent years, there has been a movement of routine spinal procedures from the inpatient to the outpatient setting. The transformation in practice is owed to the advent of minimally invasive (MIS) techniques requiring a shorter postoperative stay as well as financial pressures incentivizing quality healthcare at reduced costs (1,2). Compared to traditional open procedures, the adoption of MIS techniques allows for effective treatment of the pathology through the smallest surgical footprint which limits tissue damage and blood loss (3). Patients now experience decreased postoperative pain, narcotics usage, and overall accelerated recovery (4). As a result, a handful of spine procedures have become “same-day surgeries” in the last couple of decades.
Along with microdiscectomies, MIS lumbar decompressions (LD) have been the largest proportion of spine cases that have transitioned to the outpatient setting (5,6). Although MIS LD is a relatively low-risk surgery, there is limited data regarding clinical and surgical outcomes as an outpatient procedure. As a certain subset of patients may be better candidates for the outpatient setting due to differences in comorbidities and other risk factors predisposing to poor outcomes, it is important to identify patient selection criteria and discharge protocols to optimize safety and efficacy of outpatient MIS LD. In this context, our purpose is to evaluate a single surgeon’s experience with performing MIS LD in the outpatient versus inpatient setting and determining if there are differences in surgical and clinical outcomes.
Methods
Patient selection
A prospectively-maintained surgical database was retrospectively reviewed for patients undergoing primary, one- to three-level MIS LD. All procedures were conducted by a single surgeon between 2013 and 2018. All inpatient procedures were performed at a single academic institution and all outpatient procedures were performed at a single ambulatory surgery center (ASC). Patients were selected if they underwent a MIS LD for degenerative pathology. Patients were excluded if they were undergoing a revision procedure, had a non-degenerative surgical indication, or had less than 6 months of postoperative follow-up.
Surgical technique
Following fluoroscopic visualization of the index level of pathology, a unilateral approach was performed via a 2-cm paramedian skin incision. Following dissection to the level of the deep fascia, a series of tubular dilators were used to fit either a 16- or 21-mm non-expandable tubular retractor. Next, bony decompression was achieved through laminectomies, facetectomies, and foraminotomies using a high-speed burr. The ligamentum flavum was then resected with a 3-mm Kerrison rongeur. In patients requiring a microdiscectomy, the traversing nerve root was gently retracted medially and the disc fragment was resected using a pituitary rongeur.
Data collection
Patients were stratified by surgical setting: ASC (outpatient) versus hospital (inpatient). Demographic variables included age, gender, body mass index, diabetes status, smoking status, insurance, and comorbidity burden. Comorbidity burden was measured as Charlson Comorbidity Index with the age component removed. Perioperative characteristics included number of operative levels, procedure details, operative time, estimated blood loss, and length of hospital stay. Additionally, immediate postoperative visual analogue scale (VAS) pain scores and total daily narcotics consumption measured in oral morphine equivalents (OME) were collected. Lastly, perioperative and postoperative complications were recorded.
Patient-reported outcomes including Oswestry Disability Index (ODI), VAS back pain, and VAS leg pain were collected in the preoperative period as well as 6 weeks, 3, 6, and 12 months postoperative follow-up. ODI is a 10-item questionnaire that evaluates pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sexual function, social life, and traveling. It is reported as a percentage of total possible points with higher scores indicating greater disability. VAS back and VAS leg assess pain in respective anatomic regions on a scale of 0 (minimum pain) to 10 (maximum pain).
Statistical analysis
Statistical analysis was performed using Stata/MP® 13.1 for Mac (StataCorp LP, College Station, TX, USA). The cohorts were tested for an association with demographic and perioperative characteristics using Chi-square analysis or linear regression for categorical and continuous variables, respectively. The subgroups were tested for an association with immediate postoperative pain and narcotics consumption as well as improvements in ODI and VAS pain scores using linear regression. Statistical significance was set at P<0.05.
Results
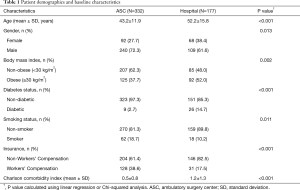
Five hundred and nine consecutive patients undergoing a primary, one- to three-level MIS LD were included in this analysis. Three hundred and thirty-two patients underwent surgery at an ASC and 177 patients underwent surgery at a hospital. Table 1 exhibits demographic data for patients in each cohort. The average age of patients was 46.4 years with 68.6% (n=349) males. Patients undergoing MIS LD in the ASC were younger (43.2 vs. 52.2, years; P<0.001), and were more likely to be male (72.3% vs. 61.6%; P=0.013), smoke (18.7% vs. 10.2%; P=0.011), and carry Workers’ Compensation insurance (38.6% vs. 17.5%; P<0.001). The hospital patients were older (52.2 vs. 43.2, years; P<0.001), more likely to be diabetic (14.7% vs. 2.7%; P<0.001), and had a greater comorbidity burden (1.2 vs. 0.5, modified Charlson Comorbidity Index; P<0.001).
Full table
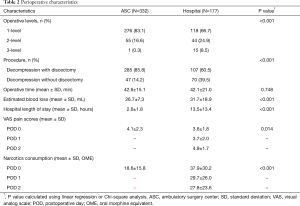
Table 2 represents perioperative characteristics for patients undergoing MIS LD in an ASC or hospital. Patients undergoing MIS LD in a hospital were more likely to have multi-level procedures [one-level: 66.7% (hospital) vs. 83.1% (ASC); two-level: 24.9% (hospital) vs. 16.6% (ASC); three-level: 8.5% (hospital) vs. 0.3% (ASC); P<0.001]. Patients in the ASC setting were more likely to have decompression with discectomy (85.8% vs. 60.5%; P<0.001) compared to patients in the hospital cohort. The operative time was similar between cohorts, however, intraoperative blood loss was higher in the hospital cohort (31.7 vs. 26.7 mL; P<0.001). Furthermore, the hospital subgroup experienced a longer length of stay (13.5 vs. 2.6 hours; P<0.001). Lastly, the patients in the ASC cohort reported higher pain scores on postoperative day (POD) 0 (4.1 vs. 3.6; P=0.014), however, they also consumed less narcotics on POD 0 (18.6 vs. 37.9 OME; P<0.001).
Full table
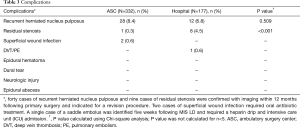
Table 3 compares complications following MIS LD between the ASC and hospital cohort. There were no cases of epidural hematomas, dural tears, permanent neurologic injuries, or epidural abscesses in either cohort. There were two cases of superficial wound infection in the ASC cohort which required oral antibiotic treatment. Next, there was a single case of a saddle embolus in the hospital cohort that was identified five weeks following surgery and required a heparin drip and intensive care unit (ICU) admission. Additionally, a total of 28 (8.4%) patients had recurrent herniated nucleus pulposus in the ASC cohort compared to 12 (6.8%) patients in the hospital cohort (P=0.509). There was one (0.3%) case of residual stenosis in the ASC cohort compared to eight (4.5%) cases in the hospital cohort (P<0.001). All cases of recurrent herniated nucleus pulposus and residual stenosis were recorded within 12-months following the primary MIS LD and were indicated for a revision procedure.
Full table
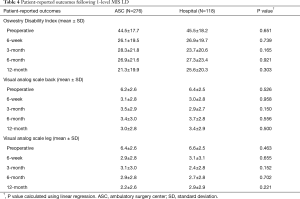
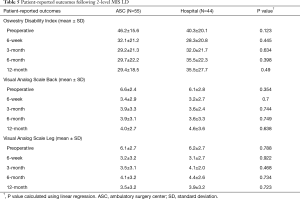
Tables 4 and 5 compare patient-reported outcomes between cohorts preoperatively and at 6-week, 3-, 6-, and 12-month follow-up for one- and two-level decompression, respectively. When comparing clinical outcomes at both one- and two-level, the cohorts demonstrated similar preoperative ODI, VAS back pain, and VAS leg pain scores as well as similar improvement in patient-reported outcomes at every postoperative time point (P>0.05).
Full table
Full table
Discussion
Although MIS LD is a relatively low-risk procedure, there is limited evidence regarding safety and efficacy of performing this surgery in the outpatient setting. Our purpose was to analyze a single surgeon’s experience regarding the performance of MIS LD in the outpatient versus inpatient setting and determine any differences in surgical or clinical outcomes.
Patient selection
When comparing patients undergoing MIS LD between the inpatient and outpatient setting, there were some key differences in demographic and baseline characteristics. In our study, patients undergoing MIS LD in the ASC were younger, and more likely to be males, smokers, and carry Workers’ Compensation insurance. The ASC cohort also was less likely to have diabetes and had a lower comorbidity burden. Additionally, the ASC cohort had a higher proportion of single-level cases (83.1% vs. 66.7%) and lower proportion of two-level cases (16.6% vs. 24.9%); there was only one (0.3%) three-level case performed in the ASC compared to 15 (8.5%) cases in the hospital. Patients in the ASC cohort were also more likely to have a simultaneous microdiscectomy performed with the decompression (85.8% vs. 60.5%). Our case series, in general, reflected a natural selection of more morbid patients and complex cases for inpatient surgery, while generally younger patients and those with Workers’ Compensation benefits were scheduled for outpatient surgery. In relation, using a multi-state ASC database, Bekelis et al. evaluated the selection process of choosing surgical candidates for outpatient lumbar discectomy. In their analysis, patients that were selected for outpatient procedures were younger and more likely to be male, Caucasian, carry private insurance, and have a lower comorbidity burden than patients undergoing an inpatient procedure (7).
Although MIS LD has become a routine outpatient procedure, morbidity and mortality can be minimized through a judicious patient selection process. Chin et al. established guidelines in choosing patients for outpatient spine surgery taking into consideration several factors. First, the authors established a maximum BMI cutoff of 42 kg/m2. Patients with a chronic medical illness must be in stable condition and cleared by a primary care physician; similarly, those with a history of heart disease must be cleared with a formal cardiology evaluation. According to the authors, patients should also have a low to moderate American Society of Anesthesiologists score (class I to III). Lastly, the authors recommend that patients live within 30 minutes from the outpatient surgery center and are with a responsible adult who is able to provide care and supervision for at least 24 hours following surgery (8).
Postoperative course
As uncontrolled postoperative pain is the most common reason for an extended stay following MIS LD, adequate pain control is necessary for a timely discharge (9). Interestingly, in our analysis, the ASC cohort had slightly higher pain scores compared to the hospital cohort (4.1 vs. 3.6; P=0.014), however the ASC patients consumed about half of the amount of narcotics on POD 0 (18.6 vs. 37.9 OME; P<0.001). Although statistically significant, the small difference (0.5 point) in pain scores are not likely clinically significant, and in conjunction with a multimodal analgesia regimen, the ASC patients consumed considerably less narcotics than the hospital cohort. Providing adequate pain control with minimal narcotic utilization may allow for avoidance of side effects such as constipation or respiratory depression, which are common causes for an extended postoperative stay (10,11). This balance of pain management is partly responsible for an average discharge time of 2.6 hours following surgery in the ASC cohort.
When comparing patient-reported outcomes following MIS LD, it was determined that both ASC and hospital cohorts reported similar preoperative and postoperative pain and disability scores throughout 12-month follow-up. Most patients experienced dramatic improvement in ODI and VAS pain scores by the 6-week time point and had continued improvement at a more moderate pace thereafter. Comparable improvements in clinical outcomes following MIS LD are expected regardless of surgical setting as all procedures were performed by a single surgeon and are presumably identical in technique in both environments.
Complications
In our combined cohort of 509 patients, there were no serious complications directly related to MIS LD including epidural hematomas, dural tears, permanent neurologic injury, or epidural abscesses. However, there were two patients in the ASC cohort with a superficial wound infection that were identified in the early weeks following surgery and required oral antibiotics. Furthermore, there was one patient in the hospital cohort that experienced a pulmonary embolism five weeks following surgery and required heparin therapy and admission to the ICU. In accordance to our study, the literature supports relatively low complication rates for MIS LD. In their systematic review evaluating spine surgery in the ambulatory setting, Sivaganesan et al. reported a complication rate ranging from 0.4–3.3% following MIS LD (9). Specifically, in their case review of 1,073 lumbar decompressions and discectomies, Helseth et al. report the most common complications as durotomies (1.3%), deep infections (1.2%), and epidural hematomas (0.7%). The authors also reported that the rate of readmission to a hospital within 90 days was 1.7% following these procedures (12). In relation, Sivaganesan et al. concluded that there were no complications or mortalities following discharge from an ASC that could have been prevented from performing the same procedure in a hospital setting (9). Thus, our results in corroboration with the literature support MIS LD as a relatively safe procedure with minimal serious complications.
In our study, we identified 40 patients with recurrent herniated nucleus pulposus, 28 (8.4%) in the ASC cohort and 12 (6.8%) in the hospital cohort (P=0.509). Additionally, the hospital cohort had eight patients (4.5%) requiring reoperation for residual stenosis versus only one patient (0.3%) in the ASC cohort (P<0.001). However, the hospital cohort had more multi-level decompressions and decompressions without discectomy which may play attribute to these differences. In relation, Helseth et al. determined that revision procedures within 12 months are relatively rare and are most commonly due to repeat disc herniation (2.7%), decompression of another level or side (2.1%), or for inadequate primary decompression (1.0%) (12). Although our investigation focused on primary operations, Hirsch et al. evaluated patients receiving revision MIS LD in an outpatient setting and determined that complications are minimal and comparable to those in an inpatient setting (13).
Discharge protocol
Although major complications following outpatient MIS LD have been reported in few numbers, a protocol is warranted for immediate postoperative surveillance, as most major complications are likely to be detected during this period (14). Helseth et al. developed a protocol suggesting that patients should be monitored for at least three hours following lumbar procedures to ensure that patients are safe for discharge. The authors recommend mobilization of lumbar patients one hour after surgery and permit discharge if the patients meet the following guidelines: adequate pain control, wound hemostasis, stable neurologic status, and ability to walk, drink liquids, and urinate. Furthermore, patients are recommended to have a family member closely monitor them during the first night after surgery and a spine surgeon available for any concerns or emergencies (12).
Strengths and limitations
This study has both strengths and limitations. All procedures were performed by a single surgeon at either a single academic hospital or a single outpatient surgery center, which reduces variability in surgical experience and technique. However, our investigation may be limited by its retrospective nature which might introduce an element of selection bias. Additionally, the clinical selection of patients into either inpatient or outpatient cohorts based on demographics, comorbidities, or pathology inherently places a bias in our study. Furthermore, complications occurring immediately after discharge along with readmission data were not collected. Lastly, clinical follow-up was limited to one-year in this analysis. Moving forward, large-scale prospective studies evaluating surgical and clinical outcomes of MIS LD in the outpatient versus inpatient setting are warranted for confirming the safety and efficacy of MIS LD as a same-day procedure.
Conclusions
In the last couple of decades, MIS LD has made a transition into becoming a routine outpatient procedure. As a result of our single surgeon’s experience in performing outpatient MIS LD, we demonstrated the procedure to be as safe and effective in an ASC compared to a hospital. Although MIS LD is a relatively low-risk procedure, appropriate patient selection and optimal postoperative protocols are imperative in minimizing complications and optimizing safety and efficacy in the outpatient setting.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board (ORA #14051301).
References
- Johans SJ, Amin BY, Mummaneni PV. Minimally invasive lumbar decompression for lumbar stenosis: review of clinical outcomes and cost effectiveness. J Neurosurg Sci 2015;59:37-45. [PubMed]
- Fabricant PD, Seeley MA, Rozell JC, et al. Cost Savings From Utilization of an Ambulatory Surgery Center for Orthopaedic Day Surgery. J Am Acad Orthop Surg 2016;24:865-71. [Crossref] [PubMed]
- Phan K, Mobbs RJ. Minimally Invasive Versus Open Laminectomy for Lumbar Stenosis: A Systematic Review and Meta-Analysis. Spine (Phila Pa 1976) 2016;41:E91-100. [Crossref] [PubMed]
- Oppenheimer JH, DeCastro I, McDonnell DE. Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurg Focus 2009;27:E9. [Crossref] [PubMed]
- Idowu OA, Boyajian HH, Ramos E, et al. Trend of Spine Surgeries in the Outpatient Hospital Setting Versus Ambulatory Surgical Center. Spine (Phila Pa 1976) 2017;42:E1429-36. [Crossref] [PubMed]
- Best MJ, Buller LT, Eismont FJ. National Trends in Ambulatory Surgery for Intervertebral Disc Disorders and Spinal Stenosis: A 12-Year Analysis of the National Surveys of Ambulatory Surgery. Spine (Phila Pa 1976) 2015;40:1703-11. [Crossref] [PubMed]
- Bekelis K, Missios S, Kakoulides G, et al. Selection of patients for ambulatory lumbar discectomy: results from four US states. Spine J 2014;14:1944-50. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Eligibility of Outpatient Spine Surgery Candidates in a Single Private Practice. Clin Spine Surg 2017;30:E1352-8. [Crossref] [PubMed]
- Sivaganesan A, Hirsch B, Phillips FM, et al. Spine Surgery in the Ambulatory Surgery Center Setting: Value-Based Advancement or Safety Liability? Neurosurgery 2018;83:159-65. [Crossref] [PubMed]
- Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician 2008;11:S105-20. [PubMed]
- Walid MS, Hyer L, Ajjan M, et al. Prevalence of opioid dependence in spine surgery patients and correlation with length of stay. J Opioid Manag 2007;3:127-8, 130-2. [Crossref] [PubMed]
- Helseth O, Lied B, Halvorsen CM, et al. Outpatient Cervical and Lumbar Spine Surgery is Feasible and Safe: A Consecutive Single Center Series of 1449 Patients. Neurosurgery 2015;76:728-37; discussion 737-8. [Crossref] [PubMed]
- Hirsch BP, Khechen B, Patel DV, et al. Safety and Efficacy of Revision Minimally Invasive Lumbar Decompression in the Ambulatory Setting. Spine (Phila Pa 1976) 2019;44:E494-9. [Crossref] [PubMed]
- Bednar DA. Description and Results of a Comprehensive Care Protocol for Overnight-Stay Spine Surgery in Adults. Spine (Phila Pa 1976) 2017;42:E871-5. [Crossref] [PubMed]


