Navigation in minimally invasive spine surgery
Introduction
Minimally invasive spine (MIS) surgery has been defined by a panel of experts as a procedure that “…by virtue of the extent and means of surgical technique results in less collateral tissue damage” (1). The AO foundation also defines MIS surgery as reducing muscle damage, blood loss and post-operative pain (2). Therefore, MIS surgery relies on limited muscle disruption while still achieving desired surgical goals. Visualization can be through a smaller and narrower dissection in MIS cases. Image guided navigation during spinal surgery can be an invaluable assistant to MIS surgeons as it allows for a larger area of visualization of bony and soft tissues through a smaller area of surgical dissection.
Computer-based navigation systems provide MIS surgeons with guidance while placing instrumentation and also for non-instrumented cases. It is used for localization as well as for adequacy of decompression in addition to instrumentation accuracy. The use of navigation allows for removing traditional fluoroscopy from the operating room. Navigation systems rely on a reference frame followed by cross sectional imaging to develop an interactive image of a patient’s anatomy. These navigation systems allow for real-time image guidance while reducing intra-operative radiation exposure (3-6). Utilization of navigation has been shown to improve accuracy of placement of pedicle screws as well (5,6).
Within this review we will discuss the benefits and barriers to adoption of navigation during MIS surgery as well as a detailed description of the senior author’s technique/workflow to incorporate navigation systems during MIS surgery. This detailed description focuses on the senior author’s operative workflow and unique use of skin-referencing to enhance surgical efficiency and reduce the number of incisions for the patient. We will then discuss potential innovations in the current body of navigation technology.
Benefits and barriers to use of navigation in MIS surgery
There has been substantial research showing the benefits of navigation in spine surgery. As mentioned above, several studies have detailed the improvement in accuracy of lumbar pedicle screw placement during surgery as compared to non-navigated surgeries (4-6). In a highly cited review of the literature by Tian et al., CT-based navigation systems had an accuracy of placement of pedicle screws of 90.76% versus fluoroscopic guided screws that only had an accuracy of 85.48%. In another study by Kim et al. the use of navigation improved accuracy of pedicle screw insertion specifically in the context of MIS surgery (7). Indeed, several articles with reviews of literature support the improved accuracy of lumbar pedicle screws placed with computer-assisted navigation compared to open techniques of insertion (8,9). Due to the unique vascular and neural anatomy of the cervical spine, computer assisted navigation can be very helpful for surgeons attempting to instrument portions of the cervical spine. This includes C1–C2 fixation as well as lateral mass screw placement (10,11).
Another benefit of use of image guided navigation is that it allows for less exposure to radiation for surgeons (12,13). Radiation exposure may impact the rate of solid tumors and risk of cataracts amongst surgeons using large amounts of fluoroscopy during their career (14). Furthermore, there is evidence of increased breast cancer prevalence amongst female orthopaedic surgeons (15). Radiation exposure should be on the forefront of every MIS surgeon, because MIS techniques are associated with increased exposure to radiation among patients, operating room staff and the spine surgeon (16). Data such as this should motivate spinal surgeons to work towards the smallest possible dose of radiation in the operating room.
There are several barriers to adoption of use of navigation during MIS surgery. There is specially designed imaging equipment as well as software that is required to perform navigated surgery which is obviously associated with its own cost (17). This cost might be offset with a reduction in operative time with quicker placement of navigated pedicle screws (18-20). Of note, there hasn’t been a comprehensive cost-effectiveness study of navigation use specifically in the context of MIS surgery. Quicker placement of pedicle screws is dependent on surgeon comfort and workflow in the operating room with use of navigation systems. Learning where to place reference markers and setup guidance systems can be a process. These additional steps can be time consuming and represent a barrier to adoption of computer assisted navigation. The authors of this study feel that once this workflow is setup there is substantial increase in efficiency of pedicle screw insertion.
Navigation systems
There are numerous computer-assisted navigation systems available to surgeons and hospitals. The most commonly used intra-operative imaging platforms are the O-arm™ (Medtronic©, Minneapolism, MN, USA), Airo® mobile intra-operative CT (Brainlab©, Feldkirchen, Germany) and the Ziehm Vision RFD 3D™ (Ziehm Imaging©, Orlando, USA). These systems work with navigation instrumentation/software. These software/instrumentation systems include the StealthStation S8 (Medtronic©, Minneapolis, MN), 7D Surgical System (7D Surgical©, Toronto, ON, USA) and Stryker Spinal Navigation with Spine Mask© (Stryker©, Kalamzoo, MI, USA). This is not a comprehensive list of navigation systems, but we believe this is the most commonly used technology in today’s operating rooms.
The three imaging platforms with which the majority of navigation procedures are performed have specific advantages and disadvantages. The Airo® mobile intra-operative CT was approved for use by the Food and Drug Administration (FDA) in 2013 (8). It has a relatively large diameter of scanner which can accommodate larger patients. The platform on which patients are placed can also be rotated which can be helpful for anesthesia staff during intubation and line placement and moving equipment into/out of the operating room. The Airo® has a 360-degree scanning capability which provides for images to be analyzed by the specified Brainlab© software. It is also portable which is beneficial for surgeons working in large centers with multiple working operating room with spine cases.
The O-arm™ has been used widely as a tool to provide 2D/3D imaging. It has the capability of moving under and above the operating room table as a “C” shaped imaging tool which then closes its gantry to provide 360-degree visualization of anatomy. It works well with the StealthStation navigation software also by Medtronic©.
The Ziehm Vision™ imaging system at first appears like an ordinary C-arm. It has the capability, however, of producing high quality intra-operative CT-scans by rotating automatically around the operative patient. The Ziehm Vision™ can interface with any of the navigation software listed above.
Senior author’s MIS navigation surgical technique
The senior author’s MIS surgical technique is centered around navigation when performing specific portions of his operations. We will outline the operating room setup, data acquisition for tracking, registration of instrumentation/patient, and operative steps while performing navigated lumbar surgery. This same setup can be used while performing nearly any MIS surgery.
Operating room setup
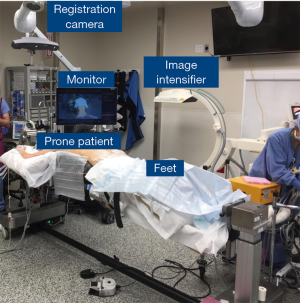
The senior author (SA) sets up the operating room with the patient prone in the center of the operating room. The image intensifier comes in from the right side of the room (as seen from the foot of the patient). The monitor with the navigation guide stays above the right side of the patient’s right shoulder. The registration camera is above the head of the bed. A labeled picture of relevant portions of the operating room are shown in Figure 1.
Data acquisition and registration
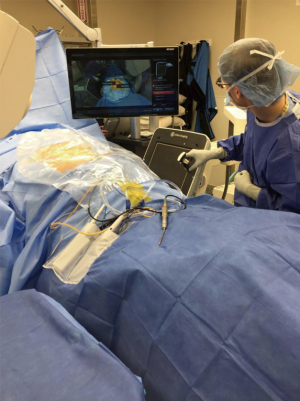
The data acquisition portion of the procedure refers to registering equipment and the patient position after prepping/draping the patient. The SA utilizes a skin-based navigation (Stryker SpineMask©) system to provide a registration point for the navigation software. The SA feels that this is the optimal method of registration for his technique of MIS surgery given the limited incisions/dissection that he utilizes. Once prepping and draping is completed, the imaging system employed (Ziehm Vision™) is used as a fluoroscopic tool to localize the location of interest for the surgery. The SA uses a trackerless registration option where an instrument is placed on specific portions of the Ziehm vision™ C-arm to orient the navigation software. A picture of this process is shown in Figure 2. After registration is performed with the Ziehm Vision™ image enhancer, a CT scan is performed. Registration is confirmed when a sterile probe is placed on known anatomic landmarks on the patient’s anatomy.
Tracking during the surgical procedure
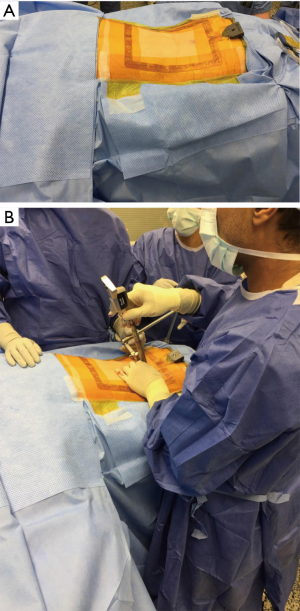
Once the SA has completed the registration process, he will use the navigation software to plan incisions/dissection for his MIS procedures. Once this location is confirmed with navigation, the SA makes a 1–2 cm incision for a MIS lumbar decompression. A series of tubes are dropped over the area of decompression as shown in Figure 3A over the lumbar spine. For certain procedures such as a MIS lumbar decompression, the surgery can be performed with the frame of the SpineMask™ as shown in Figure 3B. The SpineTracker™ is completely visible to the registration camera at the top of the bed as well.
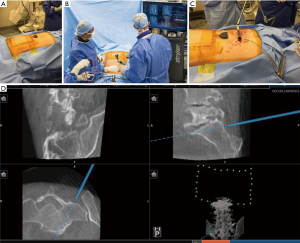
When performing a MIS transforaminal lumbar interbody fusion (TLIF) a similar setup is employed by the SA but with some slight modifications. During the MIS TLIF the SpineTracker™ is placed well above the surgical field (but within the sterile field). This new location is shown in Figure 4A. The SA then cannulates bilateral pedicles at the levels of an attempted fusion. The first step in this process involves placing percutaneous pedicle screws which is shown in Figure 4B. At this point, a tubular retractor is placed at the disc space with the assistance of the navigation equipment. This tubular retractor provides the necessary visualization and working space for the MIS TLIF. Of note, the tubular retractor is affixed firmly to the lower left side of the bed. Once the TLIF is placed, final pedicle screws are placed at each level of the fusion over guide wires. These guide wires and the location of the tubular retractor are both shown in Figure 4C. An example of the navigation interface is shown in Figure 4D. The trajectory of a S1 pedicle screw is outlined based upon the location of the probe on the sacrum.
Future research and innovations in MIS navigation surgery
There are several areas of innovation being explored to assist surgeons performing MIS navigated spinal surgery. The Augmedics xvision™ technology has been developed to assist surgeons to see instruments and computer-assisted navigation images without looking up to a monitor. This system is attached to the surgeon’s head and allows the surgeon to see clearly the images in front of the surgical field. This may assist surgeon workflow to allow for a more efficient operative technique. There is also significant research being conducted on the use of MIS surgical instrumentation combined with robotic technology (21). This integration of technology will require additional education of old and young surgeons. Further research is required to determine whether addition of this technology would assist surgeons in patient care to justify increased costs.
Conclusions
Navigation in MIS surgery offers surgeons significantly advanced visualization of a patient’s anatomy through the limited dissection that is the definition of MIS surgery. There are several different imaging platforms and navigation software available to surgeons for integration of MIS techniques with computer assisted navigation. This navigation likely helps with accuracy of pedicle screw placement and dramatically reduces intra-operative radiation. Further research is necessary to determine how robotic technology and augmented reality products will enhance patient care.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- McAfee PC, Phillips FM, Andersson G, et al. Minimally Invasive Spine Surgery. Spine (Phila Pa 1976) 2010;35:S271-3. [Crossref] [PubMed]
- Haertl R, Korge A. Minimally invasive spine surgery – techniques, evidence and controversies. 1st ed. New York: Georg Thieme Verleg, 2013.
- Bourgeois AC, Faulkner AR, Bradley YC, et al. Improved Accuracy of Minimally Invasive Transpedicular Screw Placement in the Lumbar Spine With 3-Dimensional Stereotactic Image Guidance: A Comparative Meta-Analysis. J Spinal Disord Tech 2015;28:324-9. [Crossref] [PubMed]
- Costa F, Cardia A, Ortolina A, et al. Spinal navigation: standard preoperative versus intraoperative computed tomography data set acquisition for computer-guidance system: radiological and clinical study in 100 consecutive patients. Spine (Phila Pa 1976) 2011;36:2094-8. [Crossref] [PubMed]
- Tian NF, Xu HZ. Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop 2009;33:895-903. [Crossref] [PubMed]
- Kim TT, Johnson JP, Pashman R, et al. Minimally Invasive Spinal Surgery with Intraoperative Image-Guided Navigation. Biomed Res Int 2016;2016:5716235. [Crossref] [PubMed]
- Kim TT, Drazin D, Shweikeh F, et al. Clinical and radiographic outcomes of minimally invasive percutaneous pedicle screw placement with intraoperative CT (O-arm) image guidance navigation. Neurosurg Focus 2014;36:E1. [Crossref] [PubMed]
- Overley SC, Cho SK, Mehta AI, et al. Navigation and Robotics in Spinal Surgery: Where Are We Now? Neurosurgery 2017;80:S86-99. [Crossref] [PubMed]
- Shin BJ, James AR, Njoku IU, et al. Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine 2012;17:113-22. [Crossref] [PubMed]
- Schlenzka D, Laine T, Lund T. Computer-assisted spine surgery. Eur Spine J 2000;9 Suppl 1:S57-64. [Crossref] [PubMed]
- Welch WC, Subach BR, Pollack IF, et al. Frameless stereotactic guidance for surgery of the upper cervical spine. Neurosurgery 1997;40:958-63; discussion 963-4. [Crossref] [PubMed]
- Klingler JH, Sircar R, Scheiwe C, et al. Comparative Study of C-Arms for Intraoperative 3-dimensional Imaging and Navigation in Minimally Invasive Spine Surgery Part II: Radiation Exposure. Clin Spine Surg 2017;30:E669-76. [Crossref] [PubMed]
- Mendelsohn D, Strelzow J, Dea N, et al. Patient and surgeon radiation exposure during spinal instrumentation using intraoperative computed tomography-based navigation. Spine J 2016;16:343-54. [Crossref] [PubMed]
- Hayda RA, Hsu RY, DePasse JM, et al. Radiation Exposure and Health Risks for Orthopaedic Surgeons. J Am Acad Orthop Surg 2018;26:268-77. [Crossref] [PubMed]
- Valone LC, Chambers M, Lattanza L, et al. Breast Radiation Exposure in Female Orthopaedic Surgeons. J Bone Joint Surg Am 2016;98:1808-13. [Crossref] [PubMed]
- Yu E, Khan SN. Does less invasive spine surgery result in increased radiation exposure? A systematic review. Clin Orthop Relat Res 2014;472:1738-48. [Crossref] [PubMed]
- Boon Tow BP, Yue WM, Srivastava A, et al. Does Navigation Improve Accuracy of Placement of Pedicle Screws in Single-level Lumbar Degenerative Spondylolisthesis?: A Comparison Between Free-hand and Three-dimensional O-Arm Navigation Techniques. J Spinal Disord Tech 2015;28:E472-7. [Crossref] [PubMed]
- Al-Khouja L, Shweikeh F, Pashman R, et al. Economics of image guidance and navigation in spine surgery. Surg Neurol Int 2015;6:S323-6. [Crossref] [PubMed]
- Richter M, Cakir B, Schmidt R. Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine (Phila Pa 1976) 2005;30:2280-7. [Crossref] [PubMed]
- Sasso RC, Garrido BJ. Computer-assisted spinal navigation versus serial radiography and operative time for posterior spinal fusion at L5-S1. J Spinal Disord Tech 2007;20:118-22. [Crossref] [PubMed]
- Madhavan K, Kolcun JPG, Chieng LO, et al. Augmented-reality integrated robotics in neurosurgery: are we there yet? Neurosurg Focus 2017;42:E3. [Crossref] [PubMed]