
Lumbar spinal fusion in the outpatient setting: an update on management, surgical approaches and planning
Introduction
Outpatient spinal surgery increased 5-fold between the years 1994–2006 (1), likely secondary to perceived cost savings and a rise in the number of ambulatory surgical centers (ASCs). This transition from spinal procedures performed in the inpatient setting to ambulatory settings is a function of advances in surgical and anesthesia techniques as well as financial incentives of the various stakeholders (2).
Safety is a prerequisite for outpatient spine surgery and increased complications, readmissions, and unforeseen morbidity can easily offset the proposed clinical and economic benefits of performing outpatient spinal surgery (2). Another consideration is ensuring clinical outcomes when the procedure is transitioned from the in-patient to the ASC environment (2).
The current article will provide a review of the most recent literature on outpatient lumbar fusion surgery. In particular, this review will consider pre-operative factors such as appropriate patient and procedure selection and planning. Furthermore, this review will present the current literature on outcomes of minimally invasive (MIS) and open lumbar fusion techniques in these settings. Finally, post-operative considerations will be presented.
Pre-operative considerations
Patient selection
Given the existence of particular limitations in the outpatient operative setting, such as limited emergency services, it is imperative to appropriately select patients to minimize risk of complications. With the rise in outpatient spine surgeries performed annually (3), there has been a recognition for the need for guidelines on best practices for patient selection. There are currently no universally agreed-upon selection criteria for outpatient spine surgery, and due to the retrospective nature of available studies for outpatient lumbar fusion, there is significant inherent selection bias. Smith et al. (4) recently compared inpatient (>24 h), outpatient (8–24 h), and ambulatory (<8 h) stays following outpatient MIS lateral lumbar interbody fusion (LLIF), and found that factors associated with early postoperative discharge were younger age, male sex, a non-deformity diagnosis, higher preoperative hemoglobin levels, larger preoperative disc height, fewer number of levels treated, and less extensive supplemental fixation. While limited by retrospective study design, this study provides useful guidance in terms of selecting patients for outpatient lateral lumbar fusion. In a national database study, Bovonratwet et al. (5) compared 30-day complications between patients who underwent outpatient lumbar fusion procedures to a matched cohort of patients who underwent lumbar fusion procedures as inpatients. No differences in postoperative complications (except for rate of blood transfusion), or 30-day readmission were found between outpatient and inpatient cohorts. Reasons for 30-day readmission were unfortunately not reported. These results suggest that outpatient lumbar fusion has a similar safety profile to inpatient lumbar fusion procedures in properly selected patients. Despite the lack of specific guidelines for ambulatory lumbar fusion procedures, Mohandas et al. recently made recommendations for patient selection or outpatient anterior cervical surgery based on Delphi expert panel consensus and literature review, and this information can be helpful when considering patients for ambulatory lumbar fusion (6). These recommendations, along with other available information found in the outpatient lumbar fusion literature, are summarized in Table 1.

Full table
Surgical techniques and outcomes
Several studies have examined the efficacy of transforaminal lumbar interbody fusion (TLIF). in the outpatient setting. Emami and colleagues (7) performed a retrospective cohort series of 32 patients who underwent 1- and 2-level MIS TLIF in the outpatient setting to a cohort of 64 patients who underwent the same procedure in an inpatient setting. At a minimum of two-years follow-up, the authors found no significant differences between post-operative complication rates (inpatient: 9.4%; outpatient:14.0%), readmission rates (inpatient: 4.7%; outpatient: 3.1%), or Oswestry Disability Index (ODI) and pain scores. Villavicencio and colleagues (8) reviewed 27 patients who underwent TLIF in the outpatient setting and 25 patients who underwent TLIF in the inpatient setting. The authors found that the complication rate was 14% for the outpatient cohort, but did not differ significantly from the complication rate in the inpatient setting, which was 4%.
A recent retrospective comparative analysis of 70 patients randomized to either LLIF in an inpatient hospital (n=40), or ASC (n=30), evaluated outcomes at two-years post-operatively (9). The authors of the study found no significant differences in baseline demographics or visual analogue scale (VAS) back pain scores at two-year follow-up, while patients in the ambulatory setting had significantly greater improvements in the ODI score (P=0.013). and had significantly lower rates of blood loss (143±39 vs. 56±10 mL, P=0.038), complications (20% vs. 7%). respectively, and had shorter surgical times (224±103 vs. 97±49 min, P=0.005), suggesting superior efficacy and safety in the outpatient setting when controlling for baseline patient demographics. All patients in this study underwent single-level LLIF with posterior fixation at any level from L1–5 for chronic low back pain secondary to degenerative disc disease (DDD) and low-grade spondylolisthesis after failure of 6 months of conservative treatment. All patients had BMI of <42 kg/m2 and American society of Anesthesiologists (ASA) score of 1–3, and patients with prior lumbar surgery, infection, tumor, or deformity were excluded. Smith and colleagues (4) retrospectively assessed 72 patients who underwent lumbar fusion in an ambulatory surgery center [52 treated with extreme lateral interbody fusion (XLIF) and 18 underwent MIS posterior lumbar fusions (PLF)] . The most common indications were degenerative disc disease and stenosis, and no patients were treated for deformity. Thirty nine percent had prior lumbar spine surgery. In the XLIF cohort, mean age was 50.6 years, mean BMI was 28.8, 41% had history of tobacco use, 26% had history of coronary artery disease, and 7% had diabetes. Among the XLIF patients, 57% were one-level cases, 37% were two-level cases, and 6% were three-level cases. No intraoperative complications in this cohort occurred, however there were two postoperative hospitalizations (3.7%): one <24-hour admission for postoperative urinary retention (POUR), and one admission for postoperative pain control after a three-level fusion.
Few studies have reported on the efficacy and feasibility of posterior lumbar interbody fusion (PLIF). in the outpatient setting. Chin and colleagues (10) reported on 16 consecutive patients undergoing this procedure using an open technique and determined that they had an overall fusion rate of 87.5%, as well as statistically significant reductions in VAS back pain and improvements in ODI scores. They also noted that the mean (± standard deviation). operating time and blood loss were 124.85±7.1 min and 161±32 mL, respectively, which allowed same-day discharge (versus 23-hour observation) without a drain in all patients.
Intra-operative considerations
Anesthesia
Intraoperative anesthesia and postoperative analgesia are essential considerations when performing outpatient lumbar fusion surgery. Multiple studies have demonstrated the efficacy of multimodal analgesia (4,11-13). An in-depth discussion of anesthesia is beyond the scope of this article; however commonly used protocols typically include selecting medications to limit postoperative nausea and vomiting (PONV) and urinary retention to facilitate rapid discharge, while reducing interference with intraoperative neuromonitoring (4).
LLIF
Advantages of LLIF include MIS approach with little soft tissue dissection, as well as large interbody fusion area with implants spanning the ring apophysis, which provides more structural stability and increased fusion area. The procedure has been described extensively in recent literature, and has gained popularity due to the shortened recovery time and decreased blood loss (14). However, complication rates are varied in the literature (15). This is likely multifactorial, and considerations include surgeon experience, patient-specific characteristics, use of varied access systems and application across a wide range of spinal pathologies.
The primary procedural access consideration for LLIF is the patient’s retroperitoneal anatomy. The primary concern is the location of the psoas muscle and disc space in relation to the lumbar plexus and great vessels, which can be evaluated on pre-operative MRI. If the psoas muscle is in a more anterior position, it may place the lumbar plexus at risk when attempting to access the disc space from the lateral approach. For this reason, the authors recommend reliable real-time electromyography (EMG) neuromonitoring. Similarly, a more lateral location of the great vessels could place them in the corridor for the lateral approach to the disc. Mai and colleagues (16) demonstrated that scoliosis caused variant anatomy of left-sided vasculature at L2–4, with 94.2% of the variant anatomy found on the convex side of the curvature. Vascular issues in the ASC setting could have catastrophic consequences so that the regional vascular anatomy must be carefully evaluated on pre-operative imaging studies. There is a large variation in complication rates reported in the literature for LLIF (15-18). Hijji et al. (19) performed a systematic review of the literature including over 6,800 patients undergoing LLIF. They found that although there was an overall 36% rate of early “neurologic” complications; these included any postoperative weakness or sensation loss. It should be noted that they included psoas weakness on the side of surgery, which is likely due to psoas muscle pain related to the transpsoas approach. They do not comment on whether the procedures utilized EMG during the cases within the respective studies. In their review, these sensory and motor changes were almost always a transient phenomenon, as the rate of persistent neurologic complications beyond six months was below 4% in all studies. The authors note that the near-complete resolution of symptoms after six months of recovery implies that neurologic complications are likely related to stretch on the lumbar plexus or transient psoas muscle trauma. Other complications, including wound, vascular, pulmonary, cardiac, and urologic complications occurred in less than 2% of patients.
Other authors have also noted that postoperative transient mild proximal thigh sensory loss and hip flexion weakness usually resolves by six months (20-22). Tohmeh et al. (20) found that 17.5% of patients developed transient postoperative thigh numbness, and 27.5% had mild hip flexion weakness, all of which resolved at six months follow-up. Caputo et al. (21) reported that in their series of 30 patients, all cases of post-operative hip flexion weakness resolved within four weeks (1). Reducing psoas retraction time may be a key component of preventing this phenomenon. Uribe et al. (22) showed in a prospective study with a trans-psoas approach, that patients with symptomatic neuropraxia had an average open retractor time of 32.3 min, versus 22.6 min for those without. Bendersky et al., in a retrospective review of 107 patients, had no instances of postoperative weakness or plexopathy when retraction time was kept under 20 min (23).
Limited clinical data suggests that LLIF may be safely performed in the outpatient setting, but requires careful consideration in terms of patient selection (Table 2) and a high degree of surgical expertise to prevent complications. The ideal patient would be a younger patient requiring one-level fusion without significant spinal deformity, with minimal comorbidities and retroperitoneal anatomy that lends itself to the lateral approach (5,9).
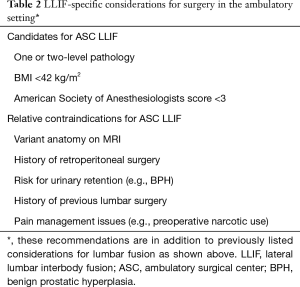
Full table
MIS TLIF
Historically, postoperative pain management concerns associated with conventional, open surgical approaches for PLF have limited the adoption of outpatient PLF. However, MIS approaches for lumbar fusion, such as the MIS TLIF, have demonstrated reduced intraoperative blood loss, decreased postoperative pain control requirements, and decreased postoperative length of stay while maintaining similar long-term outcomes to traditional open approaches (5). In properly selected patients, these procedures have therefore been able to be successfully migrated to the outpatient setting (8,24).
One of the most important technical considerations when considering outpatient MIS TLIF is experience with the procedure. Only when a provider is sufficiently experienced with performing MIS TLIF should they begin performing these as ambulatory procedures. MIS TLIF is technically challenging and has been associated with a steep learning curve, with significant differences in surgical time, blood loss, and intraoperative fluid volume reported between a surgeon’s early cases and later cases (25,26). Extended operative time and tissue dissection can significantly affect a patient’s recovery from anesthesia and postoperative pain control, respectively (25,26).
Other important intraoperative considerations of the MIS TLIF are related to the general tenets of performing a technically adequate TLIF procedure: ensuring appropriate decompression, disc space preparation, and instrumentation. In MIS TLIF, due to limited soft tissue dissection and visualization, performing adequate decompression can be challenging, but is necessary in order to have a successful clinical outcome. In cases with a prior decompression at the same level, scar formation and dural adhesions may increase the risk of dural tear, which can complicate the surgical procedure, the patient’s recovery and the ability to discharge the patient on the same day in an outpatient setting. Disc space preparation during TLIF must be performed diligently in order to maximize fusion rates. Violation of the disc space anteriorly can result in possible injury to the great vessels, a rare but potentially fatal complication that has limited treatment options in the ambulatory setting (27). Other technical factors than can affect a patient’s recovery following TLIF include the amount of nerve root and/or thecal retraction and should be minimized. Instrumentation with pedicle screws is typically performed in less-invasive fashion during MIS TLIF, and care must be taken to ensure radiographic visualization is optimal in order to avoid misplaced screws. Despite the technical challenges, multiple series have demonstrated the safe and effective adoption of MIS TLIF in the outpatient setting (2,4,7,8,24).
Open PLF
While MIS TLIF has been more often described in the outpatient setting, PLF has also been reported successfully in this setting. One technical modification to PLF that has been used in the outpatient setting includes the use of midline cortical bone trajectory pedicle screws to reduce the amount of muscle dissection while maintaining acceptable fusion rates (28). In this study of 60 patients, Chin et al. were able to transition lumbar fusions to the outpatient setting by using cortical screws instead of traditional pedicle screws. They found significant improvements in VAS back scores, VAS leg scores, and ODI scores at 2-year follow-up for the outpatient cortical screw cohort. Additionally, they reported greater improvements in VAS back scores and ODI at final follow-up in the cortical screw cohort compared to the traditional pedicle screw trajectory cohort. Using national registry data, Bovonratwet et al. (5) compared complication and readmission rates in matched cohorts of 1,440 inpatient and 360 outpatient PLF patients. This study was limited in that as a national database study, surgical details were not available, and each cohort likely included both MIS and open procedures. Nonetheless, while blood transfusion was greater in the inpatient cohort (10.8% vs. 2.8% in outpatient cohort), all other complication rates were similar, along with readmission rates (outpatient 3.6% vs. inpatient 4.4%, P=0.503). Additionally, while open TLIF in the outpatient setting is much less common compared to MIS TLIF, Chin et al. demonstrate that this can be done safely in a preliminary case series of 16 patients using either traditional trajectory or cortical trajectory pedicle screws (10). Post-operative considerations
Pain control
In addition to intraoperative anesthesia, postoperative analgesia is a critical component of multimodal pain management protocols that have facilitated outpatient spine surgery (11-13). Several published postoperative pain control protocols have been shown to be effective (13,29). The overall goal of multimodal pain management is use of a mixture of local, systemic, short-acting, and long-acting medications with varying mechanisms of action that target all components of postoperative pain. When selecting analgesic medications for fusion surgery, consideration must be given to medications that may affect bone healing such as non-steroidal anti-inflammatories. While full discussion of postoperative pain management is outside the scope of this current article, when implementing a multimodal pain management protocol, it is important for the surgical and anesthesia teams to engage in shared decision-making in order to optimize pain control for the patient.
Nausea and vomiting
PONV is one of the more common barriers to early discharge following spine surgery (29). Patients should be screened preoperatively for risk of developing PONV, and a transdermal scopolamine patch applied preoperatively can effectively prevent PONV in patients with no contraindications. Opioid medications also contribute to PONV, so limiting the usage of opioids by using liberal local anesthetic intraoperatively and relying upon non-opiate analgesia medications can significantly reduce PONV (29). Other recommendations for reducing PONV include promoting aggressive hydration and administering dexamethasone or ondansetron and famotidine on arrival (6). For persistent nausea and vomiting, metoclopramide can be used as rescue therapy.
Urinary retention
POUR following lumbar fusion is another potential barrier to early discharge. While isolated POUR often resolves without serious sequelae, concern for this complication in lumbar fusion patients is heightened by the fact that it may be a symptom of cauda equina syndrome from a compressive postoperative epidural hematoma. The rate of POUR has been reported to be as high as 20% following MIS single-level lumbar fusion (30). Risk factors identified for POUR include usage of medications such as phenylephrine and neostigmine (30). Preoperative identification of patients at risk, in addition to avoidance of these medications may potentially reduce the rate of this complication, and this is an active area of research as lumbar fusion procedures are being transitioned into the outpatient setting.
Postoperative monitoring
While there is no generally accepted amount of time that patients should be monitored postoperatively in the outpatient setting, general discharge criteria after a lumbar fusion often includes a patient tolerating oral intake, adequate pain control, voiding, stable vital signs, and stable neurologic exam. With appropriate preoperative planning and intraoperative measures, these goals can be achieved within a few hours after the procedure. A Delphi panel study on outpatient anterior cervical surgery by Mohanda and colleagues (6) recommended that nurses should follow-up via home visit or phone the morning after surgery to check on the patient regarding vital signs and neurologic status, ability to tolerate oral intake, surgical site drainage, effectiveness of analgesia, and ambulatory status.
Conclusions
Outpatient lumbar spinal fusion surgery has been reported to have similar functional outcomes, complication rates, and rates of readmission in carefully selected patients to its in-patient counter-part. Although the available data suggests the clinical and economic benefits of outpatient lumbar fusion surgery (2), particular attention must be paid to patient selection, surgical techniques, anesthesia protocols, and postoperative pain control and monitoring in order to ensure the safety and efficacy of these procedures.
Acknowledgments
None.
Footnote
Conflicts of Interest: FM Phillips receives royalties from Nuvasive, Stryker, DePuy, Medtronic; has stock/options in SAB; Nuvasive, SI Bone, Expanding Orthopaedics, Providence, Spinal Kinetics, Mainstay, Safe Orthopaedics; has BODs with Theracell, Vital 5, Edge Surgical. The other authors have no conflicts of interest to declare.
References
- Mundell BF, Gates MJ, Kerezoudis P, et al. Does patient selection account for the perceived cost savings in outpatient spine surgery? A meta-analysis of current evidence and analysis from an administrative database. J Neurosurg Spine 2018;29:687-95. [Crossref] [PubMed]
- Sivaganesan A, Hirsch B, Phillips FM, et al. Spine Surgery in the Ambulatory Surgery Center Setting: Value-Based Advancement or Safety Liability? Neurosurgery 2018;83:159-65. [Crossref] [PubMed]
- Ahn J, Bohl DD, Tabaraee E, et al. Current Trends in Outpatient Spine Surgery. Clin Spine Surg 2016;29:384-6. [Crossref] [PubMed]
- Smith WD, Wohns RN, Christian G, et al. Outpatient Minimally Invasive Lumbar Interbody: Fusion Predictive Factors and Clinical Results. Spine (Phila Pa 1976) 2016;41 Suppl 8:S106-22. [PubMed]
- Bovonratwet P, Ottesen TD, Gala RJ, et al. Outpatient elective posterior lumbar fusions appear to be safely considered for appropriately selected patients. Spine J 2018;18:1188-96. [Crossref] [PubMed]
- Mohandas A, Summa C, Worthington WB, et al. Best Practices for Outpatient Anterior Cervical Surgery: Results From a Delphi Panel. Spine (Phila Pa 1976) 2017;42:E648-59. [Crossref] [PubMed]
- Emami A, Faloon M, Issa K, et al. Minimally Invasive Transforaminal Lumbar Interbody Fusion in the Outpatient Setting. Orthopedics 2016;39:e1218-22. [Crossref] [PubMed]
- Villavicencio AT, Nelson EL, Mason A, et al. Preliminary results on feasibility of outpatient instrumented transforaminal lumbar interbody fusion. J Spinal Disord Tech 2013;26:298-304. [Crossref] [PubMed]
- Chin KR, Pencle FJ, Coombs AV, et al. Lateral Lumbar Interbody Fusion in Ambulatory Surgery Centers: Patient Selection and Outcome Measures Compared With an Inhospital Cohort. Spine (Phila Pa 1976) 2016;41:686-92. [Crossref] [PubMed]
- Chin KR, Coombs AV, Seale JA. Feasibility and patient-reported outcomes after outpatient single-level instrumented posterior lumbar interbody fusion in a surgery center: preliminary results in 16 patients. Spine (Phila Pa 1976) 2015;40:E36-42. [Crossref] [PubMed]
- Devin CJ, McGirt MJ. Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes. J Clin Neurosci 2015;22:930-8. [Crossref] [PubMed]
- Dunn LK, Durieux ME, Nemergut EC. Non-opioid analgesics: Novel approaches to perioperative analgesia for major spine surgery. Best Pract Res Clin Anaesthesiol 2016;30:79-89. [Crossref] [PubMed]
- Singh K, Bohl DD, Ahn J, et al. Multimodal Analgesia Versus Intravenous Patient-Controlled Analgesia for Minimally Invasive Transforaminal Lumbar Interbody Fusion Procedures. Spine (Phila Pa 1976) 2017;42:1145-50. [Crossref] [PubMed]
- Ozgur BM, Aryan HE, Pimenta L, et al. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 2006;6:435-43. [Crossref] [PubMed]
- Lehmen JA, Gerber EJ. MIS lateral spine surgery: a systematic literature review of complications, outcomes, and economics. Eur Spine J 2015;24 Suppl 3:287-313. [Crossref] [PubMed]
- Mai HT, Schneider AD, Alvarez AP, et al. Anatomic Considerations in the Lateral Transpsoas Interbody Fusion: The Impact of Age, Sex, BMI, and Scoliosis. Clin Spine Surg 2019;32:215-21. [Crossref] [PubMed]
- Berjano P, Lamartina C. Minimally invasive lateral transpsoas approach with advanced neurophysiologic monitoring for lumbar interbody fusion. Eur Spine J 2011;20:1584-6. [Crossref] [PubMed]
- Campbell PG, Nunley PD, Cavanaugh D, et al. Short-term outcomes of lateral lumbar interbody fusion without decompression for the treatment of symptomatic degenerative spondylolisthesis at L4-5. Neurosurg Focus 2018;44:E6. [Crossref] [PubMed]
- Hijji FY, Narain AS, Bohl DD, et al. Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J 2017;17:1412-9. [Crossref] [PubMed]
- Tohmeh AG, Rodgers WB, Peterson MD. Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine 2011;14:31-7. [Crossref] [PubMed]
- Caputo AM, Michael KW, Chapman TM Jr, et al. Clinical outcomes of extreme lateral interbody fusion in the treatment of adult degenerative scoliosis. ScientificWorldJournal 2012;2012:680643.
- Uribe JS, Isaacs RE, Youssef JA, et al. Can triggered electromyography monitoring throughout retraction predict postoperative symptomatic neuropraxia after XLIF? Results from a prospective multicenter trial. Eur Spine J 2015;24 Suppl 3:378-85. [Crossref] [PubMed]
- Bendersky M, Sola C, Muntadas J, et al. Monitoring lumbar plexus integrity in extreme lateral transpsoas approaches to the lumbar spine: a new protocol with anatomical bases. Eur Spine J 2015;24:1051-7. [Crossref] [PubMed]
- Eckman WW, Hester L, McMillen M. Same-day discharge after minimally invasive transforaminal lumbar interbody fusion: a series of 808 cases. Clin Orthop Relat Res 2014;472:1806-12. [Crossref] [PubMed]
- Nandyala SV, Fineberg SJ, Pelton M, et al. Minimally invasive transforaminal lumbar interbody fusion: one surgeon's learning curve. Spine J 2014;14:1460-5. [Crossref] [PubMed]
- Lee JC, Jang HD, Shin BJ. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: our experience in 86 consecutive cases. Spine (Phila Pa 1976) 2012;37:1548-57. [Crossref] [PubMed]
- Bae HJ, Cho TG, Kim CH, et al. Aortic Injury during Transforaminal Lumbar Interbody Fusion. Korean J Spine 2017;14:118-20. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Clinical Outcomes With Midline Cortical Bone Trajectory Pedicle Screws Versus Traditional Pedicle Screws in Moving Lumbar Fusions From Hospitals to Outpatient Surgery Centers. Clin Spine Surg 2017;30:E791-7. [Crossref] [PubMed]
- Buvanendran A, Thillainathan V. Preoperative and postoperative anesthetic and analgesic techniques for minimally invasive surgery of the spine. Spine (Phila Pa 1976) 2010;35:S274-80. [Crossref] [PubMed]
- Mayo BC, Louie PK, Bohl DD, et al. Effects of Intraoperative Anesthetic Medications on Postoperative Urinary Retention After Single-Level Lumbar Fusion. Spine (Phila Pa 1976) 2016;41:1441-6. [Crossref] [PubMed]


