
Patient education in an ambulatory surgical center setting
Introduction
Advancements in surgical technology over the past decade have resulted in the ability to perform complex surgical procedures on the spine with decreased morbidity and advanced recovery. With an increased national focus on decreasing health expenditures, spine surgery has been particularly highlighted as having potential to make significant changes in the current landscape (1). This has resulted in a recent push towards further streamlining various spine procedures in an effort to decrease postoperative pain, minimize narcotic use, promote faster recovery, and decrease complications without compromising the quality of the procedure performed. Minimally invasive techniques have the potential to pave the way for surgeons to execute safe and effective procedures directed at achieving these goals. In partnership with anesthesiologists, the door has been opened for a number of spine surgeries to be performed in an ambulatory surgical center (ASC) setting.
There is growing evidence in support of minimally invasive techniques for a number of spine surgeries that were traditionally performed in an open fashion (2-4). Additionally, there is evidence that performing these surgeries in an ASC setting can decrease medical costs compared to similar procedures previously performed in the hospital setting (5). However, for the surgeon considering performing ASC spine surgeries, there are a number of considerations that may not be immediately apparent. Certainly, the decision requires significant planning and should be made in light of a thorough understanding of the potential complications that could affect a patient in the early postoperative period away from the direct monitoring of health care professionals. For the surgeon, it can be easy to overlook the amount of postoperative care and education that can occur over a short period of time while in the hospital that would not occur in an ASC without the appropriate structure. The benefit of overall cost reduction and the prospect of earlier return to activity that is appealing can quickly be overturned with unnecessary readmissions due to inadequate education, poor patient selection, and lack of structure and communication amongst the perioperative team.
Ethical and legal responsibilities
For the surgeon offering spine procedures in an outpatient setting, it is important to present information fairly, clearly, accurately and compassionately to patients. This becomes increasingly true when there is financial investment in an ASC where there is a responsibility to disclose all ownership interests. In 2014, Baird et al. showed that there was a trend toward surgeons performing a greater number of high-risk procedures on an ambulatory basis if they had financial interest in the ASC (6). The decision to perform a surgery at an ASC should be devoid of financial incentive, with patient safety as the primary concern.
Additionally, there are legal implications that are important to understand pertaining to ownership in an ASC. The HITECH act of 2009 (7) addressed the privacy and security concerns associated with electronic transmission of health information and provided several provisions for civil and criminal enforcement of HIPPA rules. These were subsequently extended to providers who work in or have ownership in ASCs. While surgeons are familiar with general HIPPA standards, the legal implications of transferring patient information from another site into or out of an ASC can create situations for unintentional infringement. Obtaining or disclosing protected health information without authorization could be subject to criminal penalties. Further, HIPPA agreements might be important to consider between an ASC and vendors such as health information exchange organizations, e-prescribing gateways, and personal health record vendors.
Patient selection
In 2017, Chin et al. (8) proposed a patient eligibility criteria for ambulatory spine surgeries (Table 1). First, it is important that they live or have arrangements to stay within 30 minutes of the hospital that they would be instructed to present to if a problem were to arise. It is important that a responsible adult is living or willing to stay with the patient for at least 24 hours after the surgery in the unlikely event of a significant postoperative complication. A patient’s current health status must also be critically evaluated. Any patient with a chronic medical illness should be cleared by their primary care physician and any history of cardiac disease should prompt preoperative evaluation by a cardiologist with an ECG or stress test. Additionally, a BMI cut-off of 42 is recommend. Finally, only low-moderate anesthetic risk patients should be considered for outpatient surgery (i.e., ASA <3).

Full table
Anesthesia and pain control
Close partnership with anesthesiologists is important to decrease medication-related issues that can result in the need for admission. Two of the most common reasons for unexpected transfer for admission are excessive nausea and urinary retention. Perioperative narcotic dosing should be minimized to avoid these issues. However, inadequate pain control is also a common reason for admission, thus, a well thought out postoperative regimen is required. There is substantial evidence supporting the use of multimodal analgesia following spine surgery including short-term use of NSAIDS (<14 days), neuromodulating medications such as gabapentin or pregabalin, acetaminophen, neuraxial blockades and local anesthetic injection (9). However, patients will often have preconceived expectations regarding the efficacy of these medications for managing surgical pain and commonly neglect to include them. Therefore, preoperative education regarding the importance of adhering to the multimodal program is important to prevent patients tipping the balance too heavily in favor of opioids.
Educating the patient
There are a number of pitfalls that can compromise successful ASC surgeries. However, patient education is certainly one of the most important considerations and can easily be overlooked. The process should be seen as an investment and requires making yourself available to your patients and your team. Preoperative education for each procedure offered in the ASC setting needs to be ironed out well in advance (Table 2). Patients need to be made aware that there are particular circumstances that might prompt admission to an inpatient facility. If a patient is aware of this possibility ahead of time the situation becomes much less anxiety provoking. Simple, easy to follow, and yet procedure-specific postoperative instructions are a necessity and perioperative nurses must be trained on the education required for each procedure. Frequent assessment and in-services can be helpful to ensure the highest quality of perioperative communication.
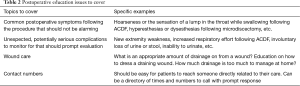
Full table
Procedure-specific preoperative education
Patients who undergo inpatient procedures rely heavily on the nurses, residents or advanced care providers to answer questions which they did not anticipate beforehand. In many cases, surgeons have become accustomed to this process taking place with specific postoperative instructions provided during the discharge process. For many patients, the comfort of knowing that they are in the hospital allows them to “trust the process” and typically alleviates a significant amount of anxiety, especially over the first night following surgery. Patients might have unrealistic expectations regarding what they should expect following a minimally invasive procedure. Without appropriate patient preparation and education much of the gains that are attainable with ASC spine surgery can easily be lost with unnecessary readmissions or emergency department visits. In fact, patients who maintain apprehension or anxiety about the prospect of outpatient surgery should be considered for inpatient surgery even in the absence of other contraindications. Ultimately, there are a number of procedure-specific issues that we focus on educating patients on preoperatively to avoid this issue.
Minimally invasive lumbar decompression
Dysesthetic pain can occur due to dorsal root ganglion irritation, most often following outside-in foraminal decompressions or far lateral microdiscectomy. This pain can be alarming to patients, often resulting in unnecessary emergency department visits. In such cases, advanced imaging is typically ordered early in the process and rarely provides any additional guidance and patients are often discharged on a higher dose of narcotics. If the patient is appropriately educated that this pain is a possibility, the patient can often be managed successfully in the outpatient setting (10). It is our practice that patients who undergo decompression procedures are provided with a prescription for a Medrol dose pack with specific instructions for filling the prescription in the case of recurrent or new dysesthetic pain. This symptom most often occurs around 2–14 days postoperatively after a short period of symptom relief and can be extremely anxiety-provoking for a patient that had been initially happy with the early improvement that they might have experienced. However, patients also need to be informed that new pain after the 2-week period is unlikely due to DRG irritation and can, alternatively, be due to recurrent herniation prompting clinic evaluation.
TLIF
Although there are some described regional anesthetic blocks for MIS TLIF, it is not uncommon that patients have greater than anticipated postoperative pain. However, with an effort to set this expectation preoperatively and with education regarding the necessity to begin oral pain control prior to the onset of increased pain as local anesthetics begin to wear off, we find that this can be effectively managed. We do not brace patients postoperatively but patients are given specific activity precautions for the first 2 weeks prior to their first postoperative visit.
ACDF/ADR
Anterior cervical discectomy and fusion (ACDF) is a very successful surgery with a great track record for clinical improvement. More recently there has been growing evidence of the clinical success of artificial disc replacement (ADR) as well. Single level procedures are now categorized as ambulatory procedures by Medicare and a majority of private insurance companies. However, these procedures also have the potential to be lethal in the early postoperative course with the rare case of an expanding hematoma causing airway compromise. In addition to hematoma formation, soft tissue swelling plays a role and is increased with multilevel surgeries. Some suggest that anything more than single level ACDF or ADR should prompt inpatient observation overnight (11) while others support that two level surgeries can safely be performed on an outpatient basis in the correct population (5). These catastrophic events, while rare, can occur and can be devastating if not addressed immediately which can occur with delayed presentation or with presentation to a facility that is not familiar with the appropriate management of this complication. Patients must be educated that some dysphagia can be normal and appropriate dietary modifications should be explained. Any difficulty breathing must be evaluated immediately and caregivers must know where to bring the patient and who to inform as rapid decompression of an obstructing hematoma by opening the incision at bedside can be lifesaving.
XLIF
Younger, healthy patients have been shown to be good candidates for even multilevel lumbar fusion via a minimally invasive lateral approach (12). The ability to place robust interbody cages through small, muscle-sparing incisions, with percutaneously placed posterior instrumentation has allowed for more rapid recovery with decreased postoperative pain. Some of the most common early concerns expressed by patients can be related to psoas trauma with painful hip flexion and the rare case of femoral neuropraxias. The former can be reasonably managed as an outpatient; however, the latter may warrant admission and monitoring.
Posterior cervical foraminotomy
In general, this procedure is very safe with rare complications. The incidence of symptomatic epidural hematoma in cervical spine surgery as a whole is extremely low. Patients typically present several days postoperatively with new neurologic deficits and a delay in diagnosis or treatment has been shown to be associated with compromised neurologic recovery. However, factors identified to be associated with an increased risk are age >60, surgery involving greater than 6 levels and an INR >2.0 in the first 48 hours of surgery (13). Ultimately, the risk for a posterior cervical lamino-foraminotomy is remarkably low, although there are documented reports in the literature (14). Therefore, patients must be advised that any new neurologic deficit needs to be urgently evaluated and the treating surgeon needs to have a low threshold to get an MRI if the patient’s symptoms persist despite an adequate decompression.
Surgeon-controlled variables in successful ambulatory spine surgery
Even with the correct surgical plan, optimal preoperative education and postoperative pathway structure, and an anesthesiologist who is on board and attentive, success hinges on a technically well-performed surgery. Although hemostasis is important for spine surgeries in general, special attention is required if a patient is going to be considered for discharge home from an ASC. We do not place drains for these procedures, although some surgeons will place drains that can be pulled several hours after the procedure while others include specific drain care and removal instructions as part of their education process. In cases where drains are to be implemented, preoperative education on this will likely avoid unnecessary phone calls and can prevent causing additional anxiety for the patient. Additionally, avoiding durotomy is essentially a requirement to successfully discharge a patient same day. Finally, surgeries must be performed efficiently to decrease operative time which has been shown to be associated with decreased risk of anesthetic complications, airway complications following ACDF (15), and symptomatic neuropraxia following lateral lumbar interbody fusions (16).
Postoperative management
It is important that patients can have their concerns addressed on an urgent basis. A plan must be in place for addressing postoperative issues as they arise. This starts in the operating room with identifying any potential issues that might warrant admission such as durotomy or neuromonitoring abnormalities during the surgery. After leaving the operating room, the care team needs to be attuned to various issues that should prompt escalation for possible admission. Such issues might include excessive nausea, uncontrolled pain, difficult to control blood pressures or change in the neurologic exam. The process for transfer to an inpatient facility should be streamlined and patients and their families or caregivers need to be reassured that this is a controlled part of the process that you and your team are prepared for. The surgeon and the ambulatory team should display confidence and the transition to the inpatient team should feel seamless which cannot occur without having the steps planned out with a team well-trained on the specific process. If they have been educated ahead of time that this change in plan is possible given particular circumstances, the patient is more likely to maintain confidence in the process.
If, however, everything goes as planned and the patient is discharged from the ambulatory center, there must be a well-thought-out method by which patient concerns are addressed. Extra vigilance is required in settings where a call service might be utilized with advanced practice providers or residents/fellows responsible for triaging phone calls. If the surgeon is not willing to make themselves directly available to the patients, the first line of response must be made aware of the general protocols and the surgeon must ultimately be available for urgent matters.
Conclusions
Ambulatory spine surgery is growing in response to a number of patient-driven variables. While advances in technologies have allowed surgeons to perform advanced procedures including cervical and lumbar fusions in this setting, it takes more than having privileges at an ASC to safely and effectively perform any number of surgeries in that setting. The process can result in improved patient satisfaction, streamlined practice efficiency, and decreased medical cost utilization. Spine surgeons looking to incorporate the ASC setting into their practice are encouraged to lay a foundation of preoperative and postoperative education that will maximize patient trust and ultimately patient safety.
Acknowledgments
None.
Footnote
Conflicts of Interest: S Qureshi: Currently receiving consulting fees from Zimmer-Biomet, Stryker Spine, Globus Medical, Inc., K2M, OnPoint Surgical, Inc., Paradigm Spine; shareholder interest in Avaz Surgical, Vital 5; and royalties from RTI, Zimmer-Biomet, Stryker Spine; board membership at Healthgrades, Minimally Invasive Spine Study Group. The other authors have no conflicts of interest to declare.
References
- Sivaganesan A, Hirsch B, Phillips FM, et al. Spine Surgery in the Ambulatory Surgery Center Setting: Value-Based Advancement or Safety Liability? Neurosurgery 2018;83:159-65. [Crossref] [PubMed]
- Kwon B, Kim DH. Lateral Lumbar Interbody Fusion: Indications, Outcomes, and Complications. J Am Acad Orthop Surg 2016;24:96-105. [Crossref] [PubMed]
- Gutman G, Rosenzweig DH, Golan JD. Surgical Treatment of Cervical Radiculopathy: Meta-analysis of Randomized Controlled Trials. Spine (Phila Pa 1976) 2018;43:E365-72. [Crossref] [PubMed]
- Stieber JR, Brown K, Donald GD, et al. Anterior cervical decompression and fusion with plate fixation as an outpatient procedure. Spine J 2005;5:503-7. [Crossref] [PubMed]
- Gornet MF, Buttermann GR, Wohns R, et al. Safety and Efficiency of Cervical Disc Arthroplasty in Ambulatory Surgery Centers vs. Hospital Settings. Int J Spine Surg 2018;12:557-64. [Crossref] [PubMed]
- Baird EO, Brietzke SC, Weinberg AD, et al. Ambulatory spine surgery: a survey study. Global Spine J 2014;4:157-60. [Crossref] [PubMed]
- Office for Civil Rights (OCR). HITECH Act Enforcement Interim Final Rule. Available online: https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html
- Chin KR, Pencle FJ, Coombs AV, et al. Eligibility of Outpatient Spine Surgery Candidates in a Single Private Practice. Clin Spine Surg 2017;30:E1352-8. [Crossref] [PubMed]
- Kurd MF, Kreitz T, Schroeder G, et al. The Role of Multimodal Analgesia in Spine Surgery. J Am Acad Orthop Surg 2017;25:260-8. [Crossref] [PubMed]
- Lewandrowski KU. Readmissions After Outpatient Transforaminal Decompression for Lumbar Foraminal and Lateral Recess Stenosis. Int J Spine Surg 2018;12:342-51. [Crossref] [PubMed]
- Gennari A, Mazas S, Coudert P, et al. Outpatient anterior cervical discectomy: A French study and literature review. Orthop Traumatol Surg Res 2018;104:581-4. [Crossref] [PubMed]
- Smith WD, Wohns RN, Christian G, et al. Outpatient Minimally Invasive Lumbar Interbody: Fusion Predictive Factors and Clinical Results. Spine (Phila Pa 1976) 2016;41 Suppl 8:S106-22. [PubMed]
- Schroeder GD, Hilibrand AS, Arnold PM, et al. Epidural Hematoma Following Cervical Spine Surgery. Global Spine J 2017;7:120S-6S. [Crossref] [PubMed]
- Choi JH, Kim JS, Lee SH. Cervical spinal epidural hematoma following cervical posterior laminoforaminotomy. J Korean Neurosurg Soc 2013;53:125-8. [Crossref] [PubMed]
- Lim S, Kesavabhotla K, Cybulski GR, et al. Predictors for Airway Complications Following Single- and Multilevel Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:379-84. [Crossref] [PubMed]
- Uribe JS, Isaacs RE, Youssef JA, et al. Can triggered electromyography monitoring throughout retraction predict postoperative symptomatic neuropraxia after XLIF? Results from a prospective multicenter trial. Eur Spine J 2015;24:378-85. [Crossref] [PubMed]


