
Costotransversectomy plus hemilaminectomy as alternative surgical approach for extramedullary intradural thoracic schwannoma resection with and without extradural extension in pediatric population three cases and literature review
Introduction
Extramedullary intradural tumors constitute up to 25% of the spinal tumors. Commonly, schwannomas present with extradural and intradural compromise (1,2), called dumbbell-shaped tumor, because the middle tumor constriction by the dura mater give them an appearance of dumbbell. The most common localization of schwannoma in pediatric population is the thoracic spine, especially in posterior and posterolateral region (3,4).
There are many surgical approaches that aim to total resection as the laminectomy (5,6), however, when the extradural compromise is present, an additional approach must be used like the costotransversectomy or the lateral extracavitary approach (7).
Following, is going to be described three different pediatric cases of thoracic spine dumbbell schwannoma. In all cases, it was performed an additional costotransversectomy to achieve a complete resection.
Case 1
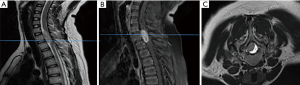
A 12-year-old girl with past history remarkable for type I neurofibromatosis, consults because 5 months history of hypoesthesia and paresthesia in pelvic region, with left predominance and weakness of lower left limb. The patient had not present sphincter compromise. At physical examination, was evident hypoesthesia in T12 to L2 dermatomes, and L1 to L2 left flaccid paresis. The external anal sphincter tone was normal. Simple and contrast-enhanced magnetic resonance imaging (MRI) of the thoracic and lumbar spine was performed (Figure 1). It was disclosing a dumbbell tumor at T12–L1 level, Sridhar classification type IV.

Case 2
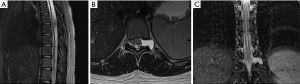
A 13-year-old girl, no history for neurofibromatosis, was brought to the physician because a 4 months-history of weakness of lower limbs, incapable for walking, with gross anesthesia. There was no urinary or fecal incontinence, or urinary retention. The physical examination was remarkable for spastic paresis of lower limbs, 1/5 right and 3/5 left, hypoesthesia in pelvic region toward lower limbs, total absence of abdominal cutaneous reflexes and bilateral presence of Babinski reflex. A simple and contrast enhanced MRI was performed, which disclose an intradural-extramedullary mass at level C7 to T2, classification Sridhar type III (Figure 2).
Case 3
A 14-year-old girl, no history for neurofibromatosis, was brought to the physician because two months history for severe low back pain with right predominance that does not let her seat down. Also, the patient referred belt-like paresthesia at navel level. Physical examination was remarkable for hyperalgesia at T10 and T11 levels; the rest of the examination was unremarkable. Simple and contrast-enhanced MRI were performed, in them was found T4 to T12 syringomyelia associated to an intradural-extramedullary tumor with T10 foraminal extension and T11 epidural compression, Sridhar classification type IV (Figure 3).
Surgical approach
With previous radiologic evaluation and planning, the localization of the costal head and posterior third of the rib contiguous to the surgical site was marked.
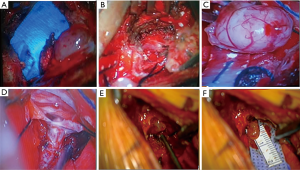
The bone was resected, the costal head and the corresponding lamina, no facetectomy was performed, so as not to destabilize the spine, until was exposed the lateral border of the dural cord and the affected root. The resection was made by microsurgical approach with ultrasonic aspirator.
Since the tumoral localization, hemilaminectomy was performed plus costotransversectomy for initial approach to an accurate dissection of the extradural portion, afterwards, was resected the intradural portion. The main risk of complication was bleeding, which was easily controlled with the technique (Figure 4).
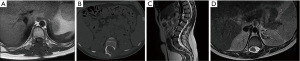
Postoperative images were made to the cases between three to four months of follow up, with adequate tumor resection (Figure 5).
Discussion
Spinal schwannomas constitute almost a third of all the primary spinal tumors. Nevertheless, schwannoma diagnosis is not common between the pediatric population, but they constitute up to 10% of nervous system, and 2.5% to 4% of all spinal tumors in this population (8,9). Distinct to adult population, where the prevalence of this pathology is up to 25% of nervous system tumors (8,9).
The schwannomas in pediatric populations does not show a marked prevalence according to sex, but some authors have established female predilection (1). Additionally, this diagnosis has had a strong association with type I neurofibromatosis (10), actually, the cases without this primary diagnosis are very strange in this population (i.e., schwannoma without neurofibromatosis) (11).
The giant spinal schwannomas are a rare form of presentation; locating more commonly in thoracic spine, followed by cervical, lumbar and sacral spine (12). The classic form is originated from posterior and posterolateral region of the thoracic spine, and its presentation is mostly intradural-extramedullary in up to 50% of cases, being the intramedullary form very rare (3,4). The dumbbell-shape presentation is 10% to 15% of the cases, we presented three cases with this growth pattern, which resection is a surgical challenge because the size these tumors can reach and, as has been said, by its localization.
Dumbbell-shaped schwannomas clinical manifestations, varies from asymptomatic or nonspecific low back pain to motor, sensitive and/or sphincter compromise (3). After the clinical suspicion, the MRI constitutes the most accurate diagnostic imaging to confirm the diagnostic impression, and also helps to establish an adequate surgical planning (13). Additionally, the spine CT and X-rays, as complementary studies, helps to evaluate the bone compromise and widened of the foramina (14).
To achieve an adequate classification of the spinal schwannoma, it most taken into account the anatomy, size and tumor localization to define the most appropriate surgical approach. According to Sridhar et al., it’s necessary that the schwannoma compromise two contiguous vertebral bodies with an extraspinal extension more than 2.5 cm to be classified as giant, with exception of giant intraosseous schwannoma (15). Sridhar modified classification was designed for thoracic, thoracolumbar and sacral spine tumors, in contrast with Asazuma classification, which is utilized for only cervical spinal lesions (16,17). The three cases presented were documented as type III, IV and V in Sridhar classification, also called dumbbell-shaped tumors.
Given its usual benign behavior, the surgery must target a complete resection, with very good prognosis for disease-free period if this is achieved (8,9). Mostly, these tumors can be approach through total laminectomy, but with high risk of great spinal instability and kyphosis, particularly in children because the damage of the components of the posterior column. To avoid this, a fusion or spinal fixation must be done.
A classic posterior approach is the most commonly selected approach for tumors smaller than 2.5 cm (14,15), but in the case of giant, invasive and dumbbell-shaped tumors, a most extensive approach should be planned. The hemilaminectomy plus costotransversectomy is a suitable approach to paraspinal extension (5,6).
In pediatric population, the costotransversectomy had been used since 1894, when Menard (18) described the first one as an approach to a spinal tuberculosis abscess. Subsequently, Ahlgren and Herkowitz described an alternative posterolateral technique to thoracic spine for paraspinal tumor resection and disc decompression at this level (19).
Currently, the costotransversectomy has been used in pediatrics in multiple conditions like thoracic disc decompression, spinal schwannomas and resection of ventral intraspinal tumors (20). Additionally, it has been useful for congenital kyphoscoliosis correction because also permits, through a posterior approach, the hemivertebra resection and instrumentation with transpedicular screws, achieving good results (20).
The surgical indications in pediatric population for this approach, stated by Smith are: thoracic disc hernia, thoracic spinal schwannoma resection, hemivertebra resection, spinal osteotomy or, simply, lesions that occupy the anterior space at this level. Also, there are some contraindications like: lordosis and patients with only one functional lung, given the high risk for pleural surgical injury (20).
Many authors had studied the surgical approach of the thoracic spine region. Lubelski et al. developed a useful algorithm for decision-making regarding when should be chosen the costotransversectomy over the lateral extracavitary surgery. This algorithm was used in the three previously presented cases, pointing to take the best surgical decision in the context of challenging tumor localization. In the three cases was accomplished a posterolateral access, without pleural injury, for ventral decompression of the spinal cord.
The costotransversectomy is used when only one level is the one to be intervened. In contrast with the lateral extracavitary approach, which permits a more widened exposition with the possibility of approach to two or more vertebral levels (7). The complications in costotransversectomy are reported from 13% to 38%, specially regarding to bleeding, post-surgical infection or pleural injury. However, the selection of the appropriate approach (i.e., depending of each case) and the adequate bone resection can diminish, substantially, these complications (21-23).
This technique was widely sought in the literature in the pediatric population, and there are no case series, case reports or studies with extensive experience, only this technique have performed in adults.
In our cases, the lesions were intradural-extramedullary, with extradural and paraspinal extension, whereby was chosen the costotransversectomy plus hemilaminectomy approach, previously applying the prior mentioned criteria stated by Lubelski et al. (7), extrapolating these criteria from adult to pediatric population. We achieve complete surgical resection, low mortality and no perioperative complications.
Conclusions
The thoracic spinal intradural-extramedullary schwannomas, with paraspinal extension that presents in pediatric population, can be safety treated through the classical posterior and posterior modified approaches, joining them, as the costotransversectomy plus hemilaminectomy, this approach combination allows a wider exposition, giving more chances and safety for a complete resection in the context of a benign tumor.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: It does not require any approval of the ethics committee, since it is a study only followed. Patients were not intervened by us.
References
- Dorsi MJ, Belzberg AJ. Paraspinal nerve sheath tumors. Neurosurg Clin N Am 2004;15:217-22. [Crossref] [PubMed]
- Rosemberg S, Fujiwara D. Epidemiology of pediatric tumors of the nervoussystem according to the WHO 2000 classification: a report of 1,195 cases from a single institution. Childs Nerv Syst 2005;21:940-4. [Crossref] [PubMed]
- Celli P, Trillò G, Ferrante L. Spinal extradural schwannoma. J Neurosurg Spine 2005;2:447-56. [Crossref] [PubMed]
- Conti P, Pansini G, Mouchaty H, et al. Spinal neurinomas: retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol 2004;61:34-43; discussion 44. [Crossref] [PubMed]
- Sim JE, Noh SJ, Song YJ, et al. Removal of intradural-extramedullary spinal cord tumors with unilateral limited laminectomy. J Korean Neurosurg Soc 2008;43:232-6. [Crossref] [PubMed]
- Nakamura H, Komagata M, Nishiyama M, et al. Resection of a dumbbell-shaped thoracic neurinoma by hemilaminectomy: a case report. Ann Thorac Cardiovasc Surg 2007;13:36-9. [PubMed]
- Lubelski D, Abdullah KG, Mroz TE, et al. Lateral extracavitary vs. costotransversectomy approaches to the thoracic spine: reflections on lessons learned. Neurosurgery 2012;71:1096-102. [Crossref] [PubMed]
- Loh JK, Lin CK, Hwang YF, et al. Primary spinal tumors in children. J Clin Neurosci 2005;12:246-8. [Crossref] [PubMed]
- Wilson PE, Oleszek JL, Clayton GH. Pediatric spinal cord tumors and masses. J Spinal Cord Med 2007;30 Suppl 1:S15-20. [Crossref] [PubMed]
- Safaee MM, Lyon R, Barbaro NM, et al. Neurological outcomes and surgical complications in 221 spinal nerve sheath tumors. J Neurosurg Spine 2017;26:103-11. [Crossref] [PubMed]
- Eljebbouri B, Gazzaz M, Akhaddar A, et al. Pediatric intramedullary schwannoma without neurofibromatosis: case report. Acta Med Iran 2013;51:727-9. [PubMed]
- Ozdemir N, Bezircioğlu H, Akar O. Giant erosive spinal schwannomas: surgical management. Br J Neurosurg 2010;24:526-31. [Crossref] [PubMed]
- Engelhard HH, Villano JL, Porter KR, et al. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina. J Neurosurg Spine 2010;13:67-77. [Crossref] [PubMed]
- Barnowsky L, Dalal R. Extradural schwannoma Management of Thoracolumbar Schwannomas manifested as an expansile vertebral lesion. AJR Am J Roentgenol 1992;159:1352-3. [Crossref] [PubMed]
- Sridhar K, Ramamurthi R, Vasudevan MC, et al. Giant invasive spinal schwannomas: definition and surgical management. J Neurosurg 2001;94:210-5. [PubMed]
- Asazuma T, Toyama Y, Maruiwa H, et al. Surgical strategy for cervical dumbbell tumors based on a three-dimensional classification. Spine 2004;29:E10-4. [Crossref] [PubMed]
- Park SC, Chung SK, Choe G, et al. Spinal intraosseous schwannoma: a case report and review. J Korean Neurosurg Soc 2009;46:403-8. [Crossref] [PubMed]
- Menard V. Etude Pratique Sur Le Mal de Pott. Paris: HACHETTE LIVRE-BNF, 1900.
- Ahlgren BD, Herkowitz HN. A modified posterolateral approach to the thoracic spine. J Spinal Disord 1995;8:69-75. [Crossref] [PubMed]
- Smith JT. Costotransversectomy. In: Tolo VT, Skaggs DL. editors. Master Techniques in Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins, 2008.
- Cybulski GR, Stone JL, Opesanmi O. Spinal cord decompression via a modified costotransversectomy approach combined with posterior instrumentation for management of metastatic neoplasms of the thoracic spine. Surg Neurol 1991;35:280-5. [Crossref] [PubMed]
- Thorat JD, Rajendra T, Thirugnanam A, et al. Single-stage posterior midline approach for dumbbell tumors of the thoracic spine, with intraoperative CT guidance. Surg Neurol Int 2011;2:31. [Crossref] [PubMed]
- Wiggins GC, Mirza S, Bellabarba C, et al. Perioperative complications with costotransversectomy and anterior approaches to thoracic and toracolumbar tumors. Neurosurg Focus 2001;11:e4. [Crossref] [PubMed]


